- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
Scroll Down
Popular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Free CalculatorTopical Finasteride Calculator
- Free Interactive GuideInteractive Guide: What Causes Hair Loss?
- Free ResourceFree Guide: Standardized Scalp Massages
- Free Course7-Day Hair Loss Email Course
- Free DatabaseIngredients Database
- Free Interactive GuideInteractive Guide: Hair Loss Disorders
- Free DatabaseTreatment Guides
- Free Lab TestsProduct Lab Tests: Purity & Potency
- Free Video & Write-upEvidence Quality Masterclass
- Free Interactive GuideDermatology Appointment Guide
More
Articles100+ free articles.
-
Hims Hair Growth Reviews: The Pros, Cons, and Real Results
-
Topical Finasteride Before and After: Real Case Studies
-
How to Reduce the Risk of Finasteride Side Effects
-
10 Best DHT-Blocking Shampoos
-
Best Minoxidil for Men: Top Picks for 2026
-
7 Best Oils for Hair Growth
-
Switching From Finasteride to Dutasteride
-
Best Minoxidil for Women: Top 6 Brands of 2026
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
Before-Afters- Transformation Photos
Our library of before-after photos.
- Client Testimonials
Read the experiences of members
Before-Afters/ Client Testimonials- Popular Treatments
-
Articles
Finasteride is an FDA-approved medication for androgenic hair loss in men. Clinical studies suggest that 1 mg daily of finasteride can improve hair loss in 80-90% of men with androgenic alopecia (AGA) – with 5- and 10-year studies demonstrating hair maintenance in a large portion of users who continue treatment.
As such, many consider finasteride to be the gold-standard medical therapy for AGA.
But what happens when someone stops using finasteride? How long are hair gains preserved? When does hair loss resume? And can someone quit finasteride, but keep their hair gains by replacing finasteride with other treatments and/or therapies?
This article explores some of the studies attempting to answer these questions.[1]https://pubmed.ncbi.nlm.nih.gov/9777765/[2]https://pubmed.ncbi.nlm.nih.gov/11809594/[3]https://www.oatext.com/Long-term-(10-year)-efficacy-of-finasteride-in-523-Japanese-men-with-androgenetic-alopecia.php
Interested in Oral Finasteride?
Oral finasteride & minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Happens If I Stop Using Finasteride?
Package inserts for the drug Propecia® (brandname finasteride) suggest that within 3-12 months of quitting finasteride, hair loss resumes and hair counts return to where they were prior to starting the drug.
But what’s the basis for this statement? In other words, where’s the scientific support?
The evidence actually comes from the original Phase II and Phase III clinical trials that granted finasteride FDA-approval for the treatment of androgenic alopecia.[4]https://pubmed.ncbi.nlm.nih.gov/9777765/
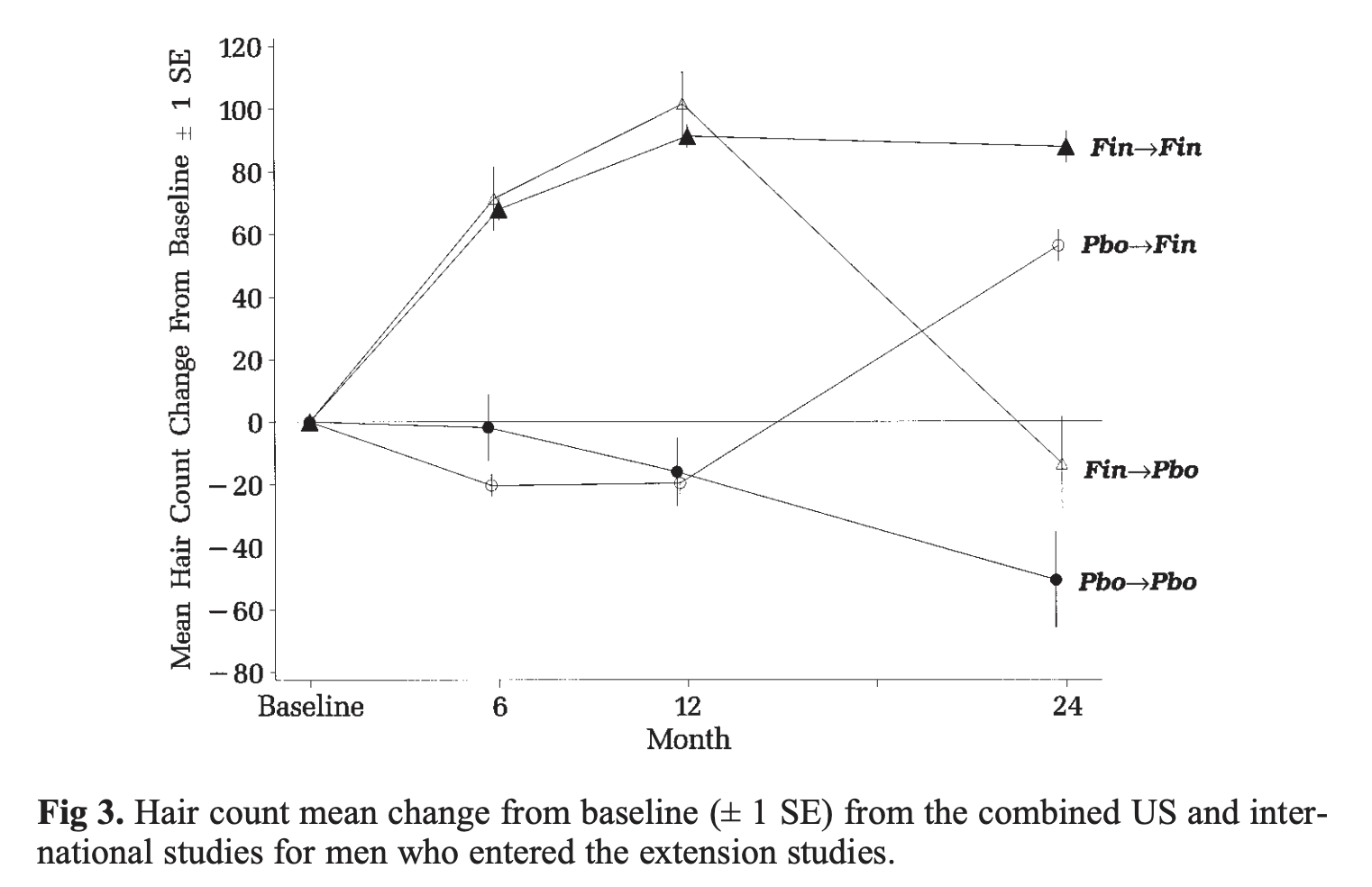
In a subset of finasteride users, participants were given the drug for a full year, then unknowingly switched into the placebo (i.e., sugar pill) group for the second year (i.e., months 12-24).
The investigators then charted these participants’ hair count changes from months 0-24, and compared those changes to those who continued using finasteride and those who were always receiving the placebo pill.
The results: unknowingly quitting finasteride led to a return to month 0 hair counts (actually, slightly below baseline) after 12 months of discontinuance. Just see the following chart. The group labeled Fin→Pbo is the group who took finasteride for year one, and a placebo pill for year two.
Kaufman KD, Olsen EA, Whiting D, Savin R, DeVillez R, Bergfeld W, Price VH, Van Neste D, Roberts JL, Hordinsky M, Shapiro J, Binkowitz B, Gormley GJ. Finasteride in the treatment of men with androgenetic alopecia. Finasteride Male Pattern Hair Loss Study Group. J Am Acad Dermatol. 1998 Oct;39(4 Pt 1):578-89. doi: 10.1016/s0190-9622(98)70007-6. PMID: 9777765.
This chart provides the scientific backing for the claims made within the Propecia® package insert. It’s also the reason why manufacturers of finasteride state that the drug must be used for a lifetime in order to maintain any of the hair gained and/or preserved by the drug.
What If I Stop Taking Finasteride Temporarily?
Under some circumstances, it is possible to stop taking finasteride temporarily, and without losing much (or any) hair. This is because there is a delay between the time at which finasteride is discontinued and when hair loss resumes.
The reason for this delay is because of the way finasteride behaves in the body – i.e., the drug’s pharmacokinetics. More specifically, finasteride’s metabolism and timing of effects on the body depend on factors such as its:
- Terminal half-life
- Biological half-life
- Tissue dissociation timings
For a deep-dive into these topics, see these articles.
- Finasteride: How Long Does It Stay In The Bloodstream?
- Finasteride: How Long Does It Stay Active In Scalp Tissue?
Otherwise, here are the key takeaways:
1. Finasteride’s biological effects can last up to 30 days after quitting
Due to finasteride’s terminal half-life of 5-7 hours and tissue dissociation timing of 4-5 days, the drug can actually exert biological effects on hormone profiles even up to ~30 days after quitting.
That means that finasteride can continue to therapeutically lower scalp levels of dihydrotestosterone (DHT), even for weeks after quitting the medication.
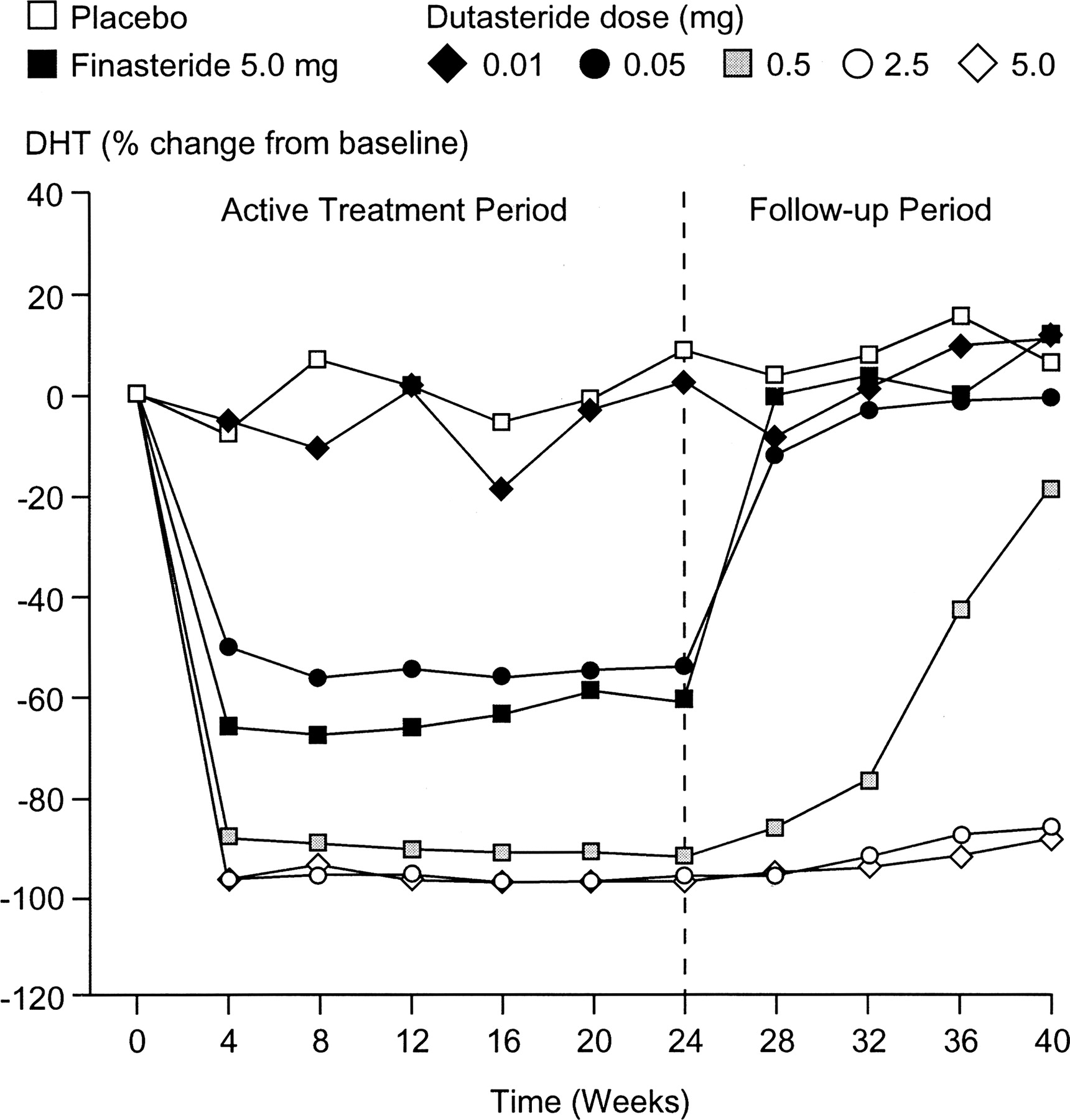
Just see this chart, which shows that even after men quit using finasteride, it still took several weeks before their serum DHT levels returned to baseline.[5]https://academic.oup.com/jcem/article/89/5/2179/2844345
Richard V. Clark, David J. Hermann, Glenn R. Cunningham, Timothy H. Wilson, Betsy B. Morrill, Stuart Hobbs, Marked Suppression of Dihydrotestosterone in Men with Benign Prostatic Hyperplasia by Dutasteride, a Dual 5α-Reductase Inhibitor, The Journal of Clinical Endocrinology & Metabolism, Volume 89, Issue 5, 1 May 2004, Pages 2179–2184
(Note: these relationships assume that finasteride reachced full tissue distribution and a steady-state plasma level commensurate with 1-5 mg of daily use over a number of weeks. For those who only took finasteride a handful of times, the drug’s effects may only take a matter of days to reverse).
2. Users can take advantage of the pharmacokinetics of finasteride to reduce drug exposure and still preserve their hair gains
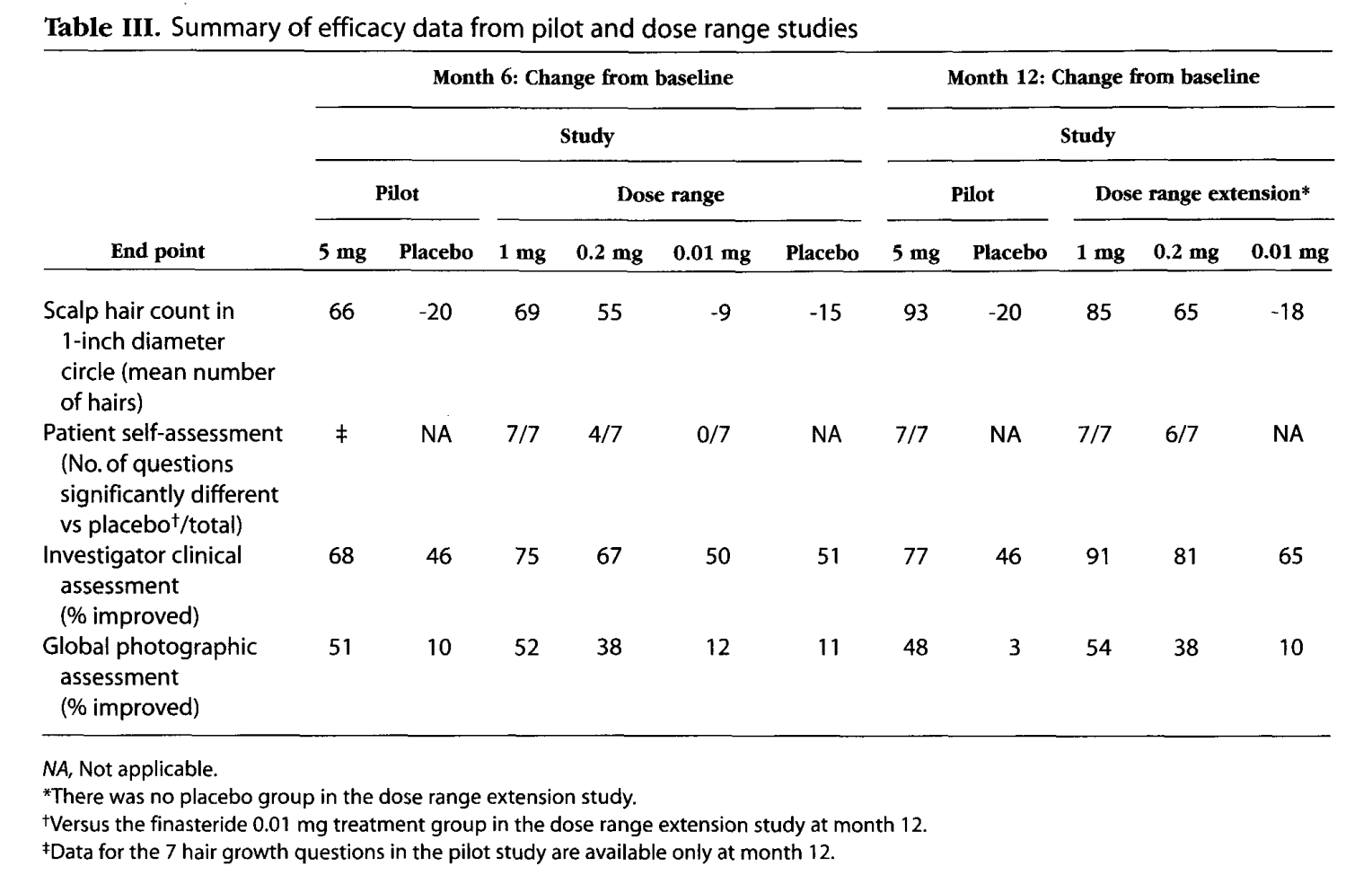
Finasteride is FDA-approved for androgenic alopecia at 1 mg daily doses. However, given the pharmacokinetics of the drug, some researchers have wondered if daily dosing is necessary.
One investigation group decided to explore this by putting a group of men on 1 mg of finasteride daily for a year. But for year two, they randomized the men into two groups: one group who would continue taking finasteride every day, and the other group who would start a 30 days-on, 30 days-off dosing approach.
The researchers found that both groups achieved comparable hair parameter improvements in year two – even despite the second group only technically using finasteride for half the time (i.e., a total of 6 months versus 12 months).[6]https://jaad.org/retrieve/pii/S0190962220319289
The hypothesis: that finasteride’s pharmacokinetics allow for dosing schedules that alternate month-to-month. For those wanting to lower their drug exposure or simply “take breaks” from the medication – for any reason – this type of dosing might allow for this to happen without sacrificing much (or any) hair gains.
What If I Stop Finasteride For Longer Than One Month?
Say you’re troubleshooting side effects, or trying to conceive, and you decide to pause your use of finasteride for longer than one month.
Under these circumstances, there is a higher likelihood of hair loss resuming versus the 30-day withdrawal window. We see this reflected clinically in the withdrawal studies on finasteride, as well as anecdotally amongst members of our membership community.
This is because after 30 days of withdrawal, the effects of finasteride on scalp DHT levels have mostly worn off. This means that scalp DHT levels return to baseline, and under these circumstances, hair loss will eventually resume.
However, for many people, the resumption of hair loss doesn’t happen immediately. While there aren’t any studies of which we’re aware that track finasteride withdrawal versus hair count changes on a month-by-month basis, we have communicated with many finasteride users who’ve consistently reported, after quitting, that hair shedding and hair loss didn’t seem to pick back up again until months 2, 3, and beyond.
Even still, if you’re considering pausing finasteride use for any reason, try to keep the window of time beyond 30 days to a minimum. In doing so, you’ll put yourself in the best possible position for drug-related hair maintenance.
What If I Quit Finasteride And Replace It With Other Treatments?
We get this question all the time, and unfortunately, there’s no good clinical data to answer this question.
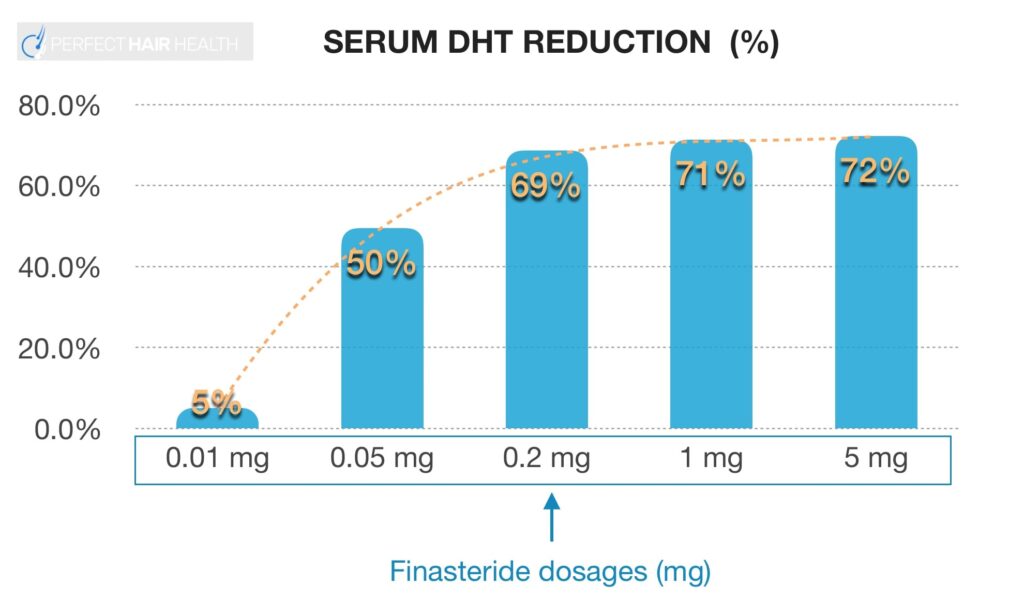
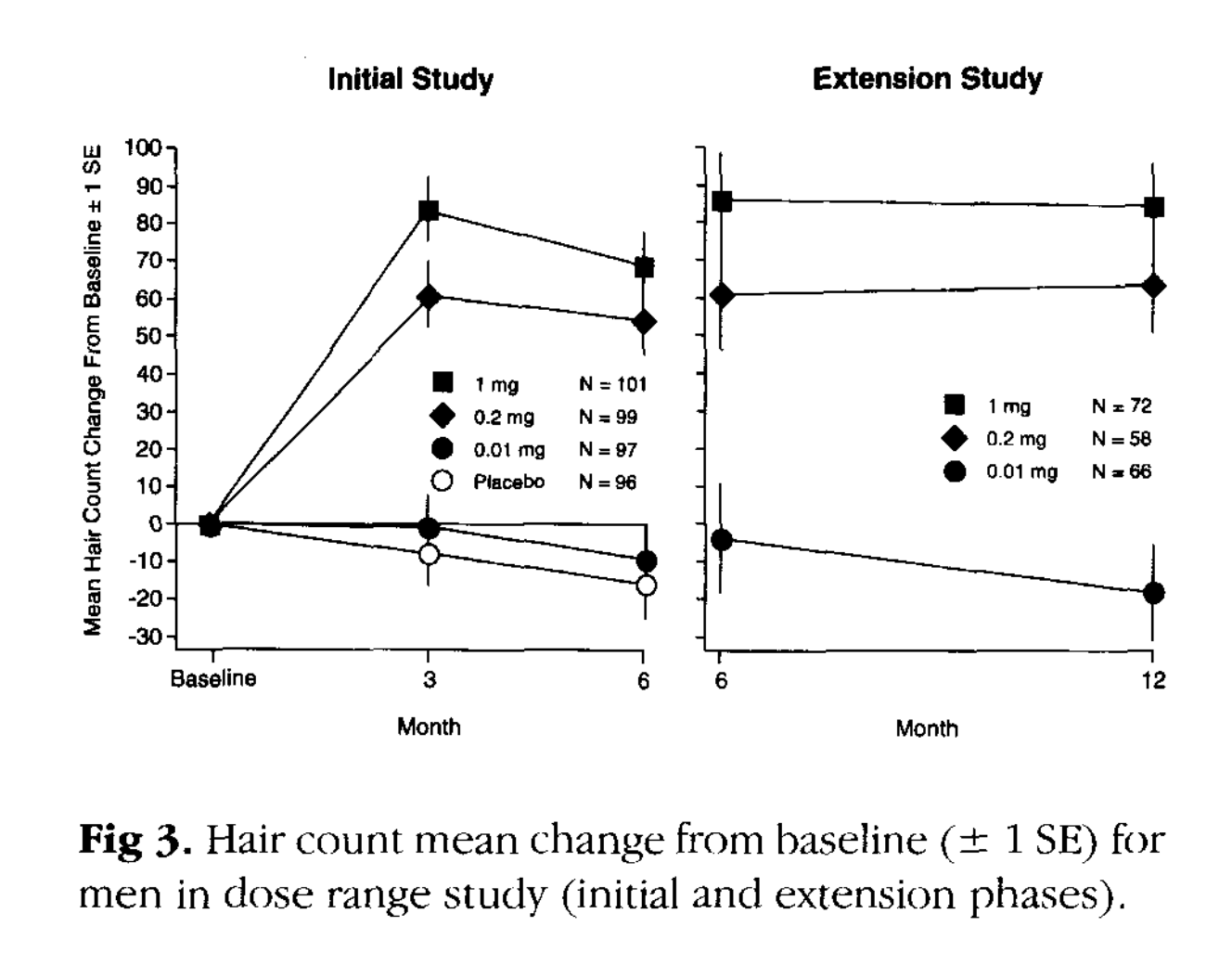
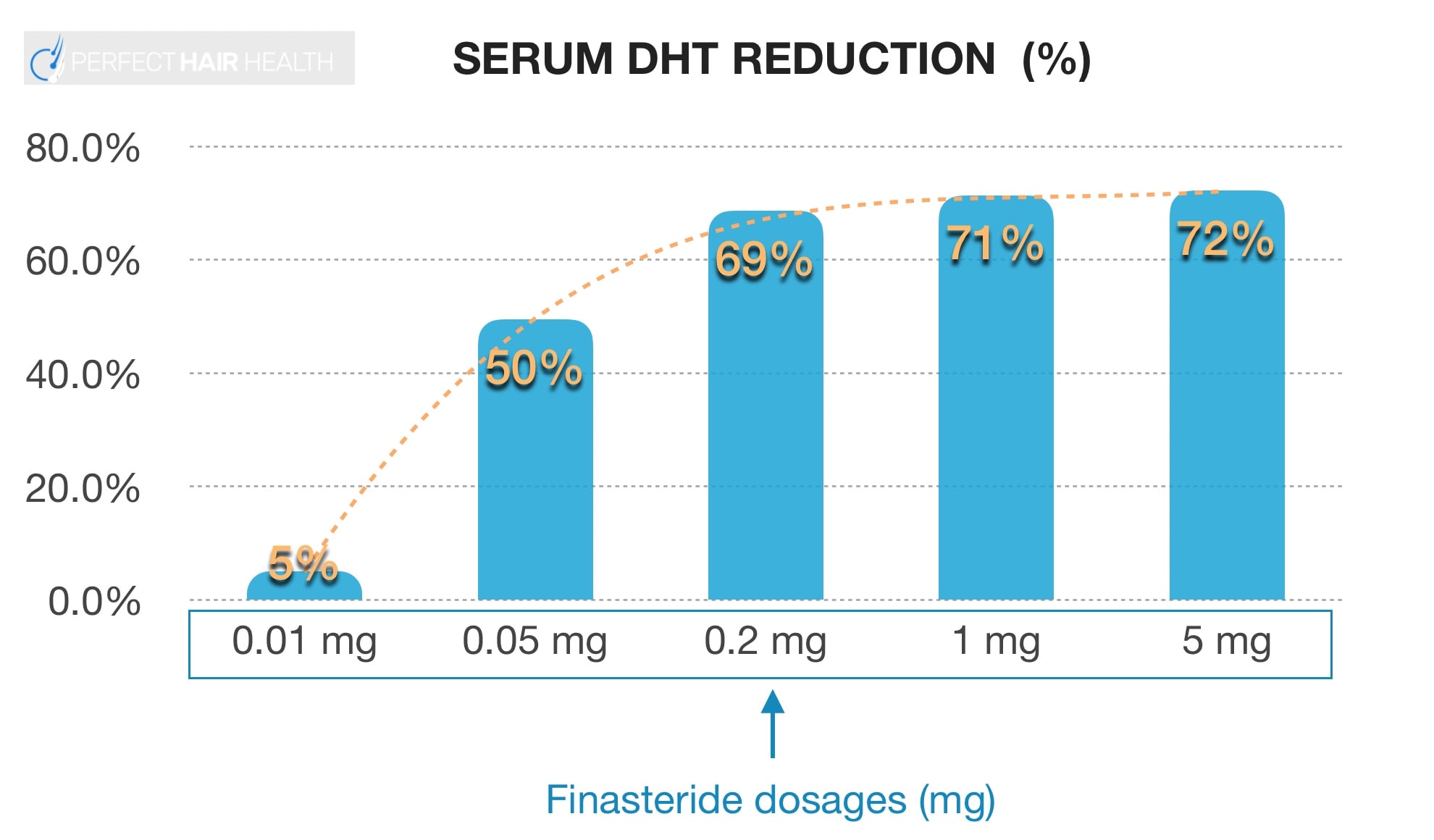
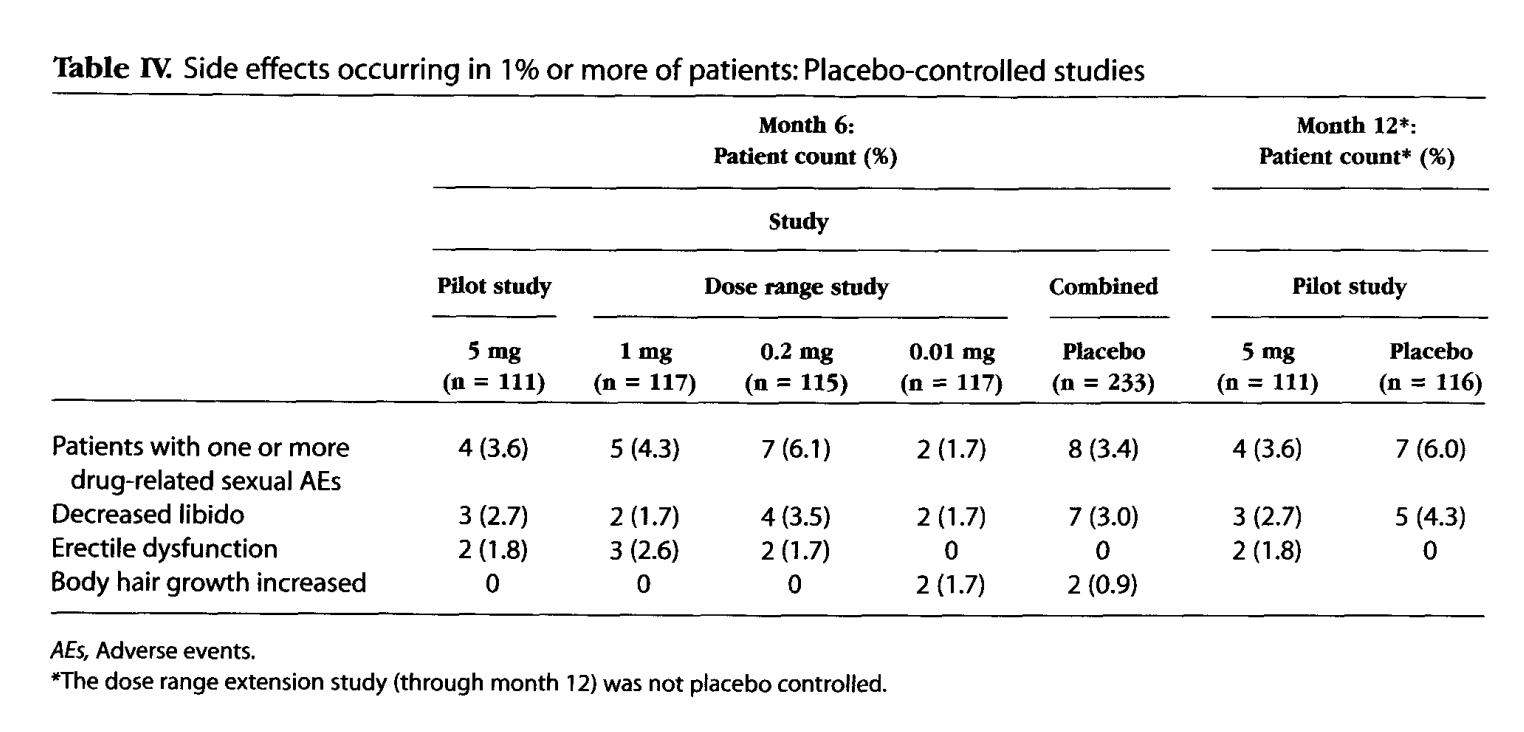
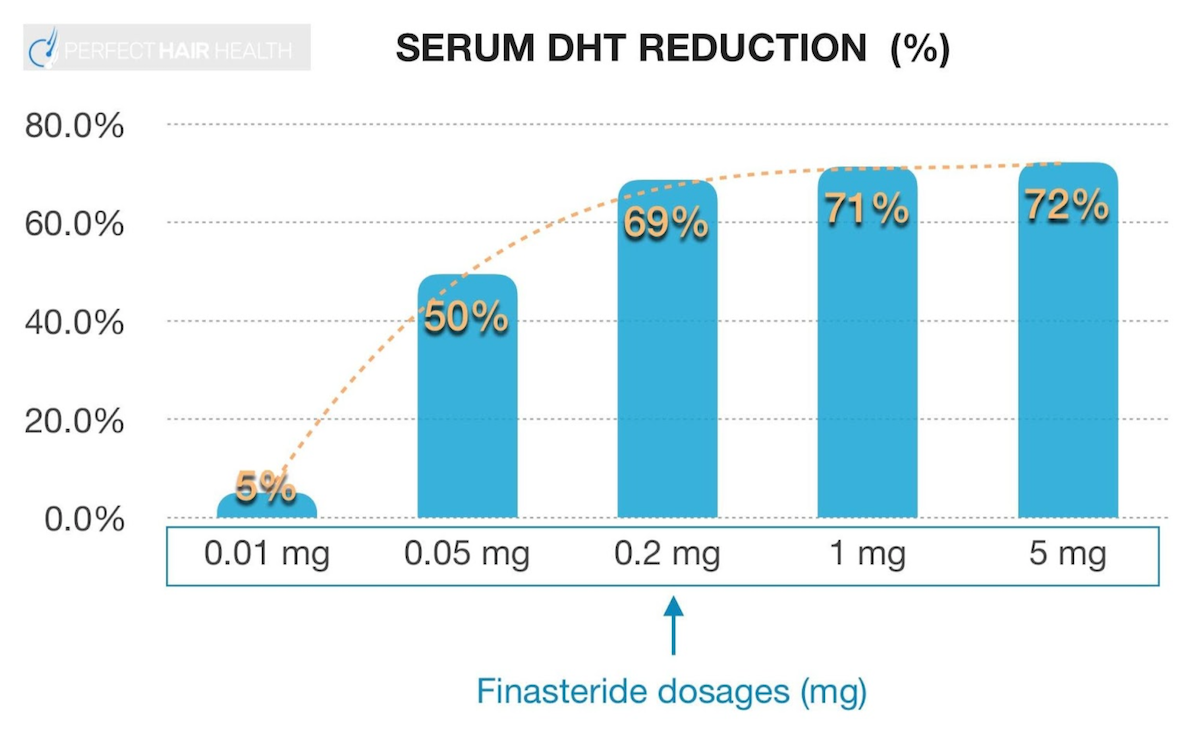
Scientifically speaking, finasteride’s mechanism of action is that it suppresses scalp DHT levels low enough to allow for hair cycle normalization and the partial reversal of hair follicle miniaturization. This typically occurs only at therapeutic levels of DHT reduction, which according to clinical studies for hair regrowth, seem to require lowering scalp DHT by 60-70%.
If someone quits finasteride and replaces the drug with other treatments, the preservation of any hair gains from finasteride will, for the most part, directly depend on the ability for those “replacement treatments” to suppress DHT levels to the same degree of finasteride.
For better or for worse, finasteride is one of the best tools we have to therapeutically and safely suppress scalp DHT levels enough to generate long-lasting hair growth – even despite its risk of side effects, which seem to affect 5-15% of users trying the drug.
Therefore, for anyone considering quitting finasteride, the most important question is to understand why. Then, we can create a roadmap or action plan based on that answer. For example:
- If quitting finasteride (as a male) to start to conceive: this can be done temporarily, and without a high risk of hair loss provided that you can conceive after month one of quitting but before month three of discontinuance.
- If quitting finasteride due to side effects: there’s a good chance that those side effects can be managed or eliminated with dose titration strategies, and/or the use of topical finasteride.
- If quitting finasteride because you want to try a natural approach to treating hair loss: we recommend first adding in a natural approach alongside finasteride use, rather than quitting finasteride abruptly.
- If quitting finasteride because you no longer want to use drugs to treat hair loss: we recommend watching this video to ensure your decision isn’t rooted in cognitive dissonance or misinformation.
If quitting finasteride for any other reason, please note that there are no studies exploring outcomes for men or women who withdraw from finasteride and replace the drug with other treatments.
Having said that, the totality of evidence strongly suggests that this is not necessarily a good gamble to make – as finasteride tends to suppress DHT levels in the scalp by a far larger margin (and for a far longer time period) than natural extracts such as saw palmetto. So, your expectation should be that hair loss, in all likelihood, will slowly resume.
Even still, we have seen success stories of people transitioning off finasteride and maintaining their hair gains. While this isn’t an approach we recommend unless absolutely necessary, here are the commonalities amongst people who’ve reported success with this:
- They multi-target their hair loss. In other words, they replace finasteride use with an array of supplements, topicals, and stimulation-based interventions that target their hair loss from multiple angles: DHT reduction, growth stimulation, angiogenesis, and more.
- They don’t immediately withdraw from finasteride. Instead, they add in all replacement interventions alongside finasteride use – and for at least 9-12 months. This allows for any potential synergies to occur between finasteride use and other therapies. Then, after achieving a new level of hair regrowth, they slowly wean away from finasteride via strategies such as topical finasteride and every-other-month oral dosing followed by titration – until after 3-5 months, they’re no longer using finasteride at all. Under the circumstances where users start noticing more hair fall, they hop back on finasteride until things stabilize. Under the circumstances whereby hair gains are maintained, they continue their drug withdrawal.
To reiterate, this is not something we actively recommend. But for those considering doing this, we recommend the above two strategies to minimize your downside risks.
Want Help With Your Hair Loss?
We offer one-on-one support to hair loss sufferers inside our membership community. This is where you can interact directly with hair loss researchers, access our library of product reviews, use our automated tools to build yourself a personalized regrowth plan, and protect yourself from the overwhelming negativity of most online hair loss forums.
If you’re interested in learning more, you can access our membership community right here.
Otherwise, we hope this article helps you make more informed decisions about your treatment choices.
References[+]
References ↑1, ↑4 https://pubmed.ncbi.nlm.nih.gov/9777765/ ↑2 https://pubmed.ncbi.nlm.nih.gov/11809594/ ↑3 https://www.oatext.com/Long-term-(10-year)-efficacy-of-finasteride-in-523-Japanese-men-with-androgenetic-alopecia.php ↑5 https://academic.oup.com/jcem/article/89/5/2179/2844345 ↑6 https://jaad.org/retrieve/pii/S0190962220319289 In this article, we’ll explore the science behind topical finasteride, if incidental exposure to the drug comes with a risk of harming pregnant women and/or children, and strategies you can employ starting today to minimize inadvertently exposing your household to secondary finasteride exposure – all while still preserving your hair gains from the drug.
Topical Finasteride: Benefits & Drawbacks
Finasteride is the world’s most effective FDA-approved treatment for androgenic alopecia in men. Having said that, the drug is not safe for use in children or in pregnant woman – mainly because it inhibits an enzyme that is critical for proper fetal and adolescent development.
Oral formulations of finasteride are ingested by the user, and thereby eliminate almost all possibilities of incidental drug exposure to partners or other household members of the drug user. The only exception to this is a small amount of detectable finasteride in semen, which can be absorbed by a partner during periods of unprotected intercourse – and in amounts that are considered far below danger levels (even while pregnant).[1]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2018472/pdf/11785276.pdf
In recent years, interest has exploded in an alternative delivery vehicle for finasteride: topical finasteride. This is because preliminary studies suggest topical finasteride can confer similar hair improvements versus the oral formulations, but also better localize the effects of the drug mainly to the scalp – thus lowering the risk of finasteride’s side effects.
Having said that, the switch to topical formulations comes alongside new risks: incidental drug exposure to partners and other members of the household. But are these risks quantifiable, and if so, how can we reduce them?
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

How Might Incidental Exposure To Finasteride Occur?
After applying topical finasteride, there is often a period of time – up to 30 minutes – whereby that finasteride solution has yet to fully dry onto the scalp. During this period, it’s much easier for topical finasteride to find its way onto other household surfaces or people – particularly if contact is made with the scalp.
During this window of time (when topical finasteride isn’t yet fully dried), here a few ways inadvertent exposure to topical finasteride can occur:
- Putting your head down on a pillowcase, thereby rubbing residual finasteride onto sheets that might be shared with your partner and/or children
- Resting your head on couch pillows and/or furniture surfaces
- Letting your partner and/or children play with your hair
In all of these scenarios, the amount of exposure to a partner or child will be relatively small. However, with repeated daily exposure throughout critical periods of development – such as a partner’s pregnancy or a child’s adolescence – each repeated contact comes alongside a cumulative increased risk of adverse events.
While the long-term effects of repeated, residual contact by spouses and/or children from topical finasteride have not been thoroughly investigated – and likely never will be (due to the difficulties of conducting such a study) – it goes without saying that it’s within our best interests not to expose our loved ones to unnecessary risks, particularly those that come with the potential for long-long adverse effects.
Topical Finasteride: How To Minimize Incidental Exposure To Loved Ones
Fortunately, when it comes to topical finasteride, there are great science-based management strategies that should allow you to keep using the medication while also minimizing – or even eliminating – your loved ones’ risks of incidental exposure. Here are a few that might take most of the risk off the table.
1. After applying topical finasteride, avoid physical contact for ~30 minutes
Depending on the carrier agents used for topical finasteride (alcohol, propylene glycol, etc.), most topicals should fully dry within a 30-minute window after application. At this point, most of the topical finasteride will remain trapped within the dried portion of the topical.
Once this window is reached, it’s far less likely that scalp contact with pillow cases, furniture, or even a partner’s hands will lead to appreciable leeching off the scalp. So, by making this very simple change, men and women can perhaps take most of the risk away regarding incidental finasteride exposure.
2. Wash pillow cases regularly, and try to dedicate a pillowcase just for the user of finasteride
Even after letting the topical dry, some topical finasteride (albeit significantly less) will leech onto the pillowcase or wherever else you might rest your head. While the amount will be substantially smaller than if you were to rest your hand on that pillowcase before the 30-minute time window for drying is completed, there’s still some topical finasteride that will end up in those sheets.
Under these circumstances, weekly washing of pillowcases is warranted. If that’s not of interest to you or your partner, you can instead dedicate one pillowcase to the person using topical finasteride that the other partner will not use.
If that’s not enough to create peace-of-mind, you can also consider wearing a loosely-fitting shower cap to bed. Some members of our membership community do this – particularly fathers with young boys who don’t want to leave any incidental exposure risks to chance.
3. Time your application windows for when you are out-of-the-house and/or unlikely to have skin contact with household members
Topical finasteride users can dramatically reduce the cumulative exposure risk to loved ones by timing their topical applications to periods where they are (mostly) outside of the home and/or unlikely to come into skin-to-skin contact with other household members. This can be done by either:
- Applying topical finasteride at least 30 minutes before bed, then washing it out each morning
- Applying topical finasteride prior to leaving for work, then washing it out after arriving home
If opting for either strategy, it’s critical to let topical finasteride site in the scalp skin for at least 6-12 hours. Otherwise, the diminishment in the drug’s contact time in the scalp may begin to hinder its efficacy. Here’s why.
How Long Should Topical Finasteride Stay on the Scalp Before Washing It Out?
When topicals are applied to the skin, there are multiple stages of absorption.
- Stage #1: the drug sits on the epidermis (the outermost layer of skin). Over several hours, some of the drug will absorb into the dermis, and some will evaporate.
- Stage #2: the drug absorbs percutaneously. This is when some of the drug moves from the epidermis into the dermis, where it can begin to affect hair follicles.
- Stage #3: the drug absorbs systemically. This is when some of the drug moves from the dermis into the bloodstream, where it can have systemic effects.
So, what’s the minimum amount of time topical finasteride must be left on the scalp to have an effect? First, one needs to know how much of the drug absorbs into the dermis over time.
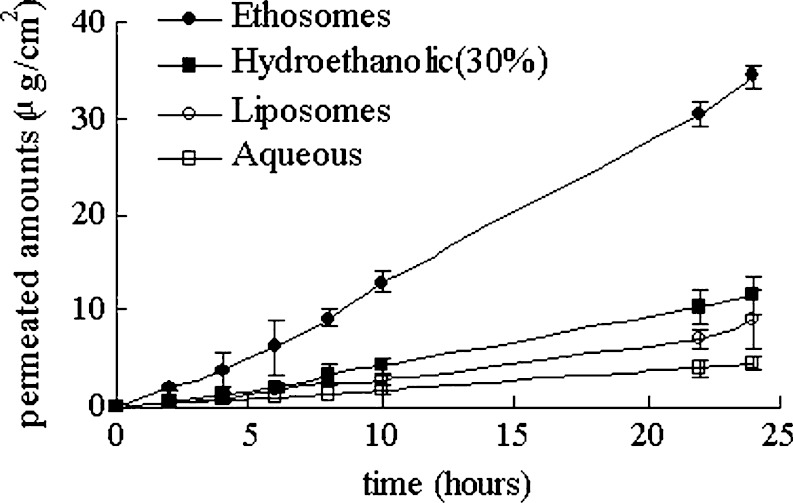
To answer this, there is an in vitro study measuring percutaneous absorption of topical finasteride across various formulations: ethosomes, ethanol, liposomes, and aqueous (water). [2]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2977015/
Here’s a chart showing the percent of topical finasteride that percutaneously absorbs (enters the dermis) over a 24-hour period:
Penetration profiles of finasteride permeating through human skin from different preparations (mean ± SD, n = 4)
According to these study results, if applying hydroethanolic finasteride to the scalp, then at the 10-hour mark, ~5 ug/cm2 will have been absorbed percutaneously. By hours 22-24, that absorption rises to ~8 ug/cm2. That means leaving the drug on the scalp for an additional 12-14 hours before washing it off only offers an additional 3 ug/cm2 of percutaneous absorption.
So, say that to minimize a partner’s exposure to finasteride means only keeping it on the scalp for 10 hours before washing it off. This begs the question: is the 5 ug/cm2 of absorbed finasteride enough to therapeutically lower scalp levels of dihydrotestosterone (DHT) and regrow hair?
Topical Finasteride: How Long Does It Need To Stay In The Scalp To Be Effective?
There aren’t any clinical studies attempting to answer this question. However, a look at surrogate data can help ballpark an answer.
First, a percentage of topical finasteride will absorb into the dermis, and a smaller percentage of topical finasteride absorbed into the dermis will later absorb into the bloodstream. This means after applying topical finasteride; people can use time-dependent DHT reductions in the bloodstream to “ballpark” how much DHT is likely also getting reduced in the scalp. This is, again, because there is more topical finasteride that percutaneously absorbs than systemically absorbs.
So, for lower dosages, the effects we see in the system can be used as signals for what’s happening, at a minimum, in the scalp skin.
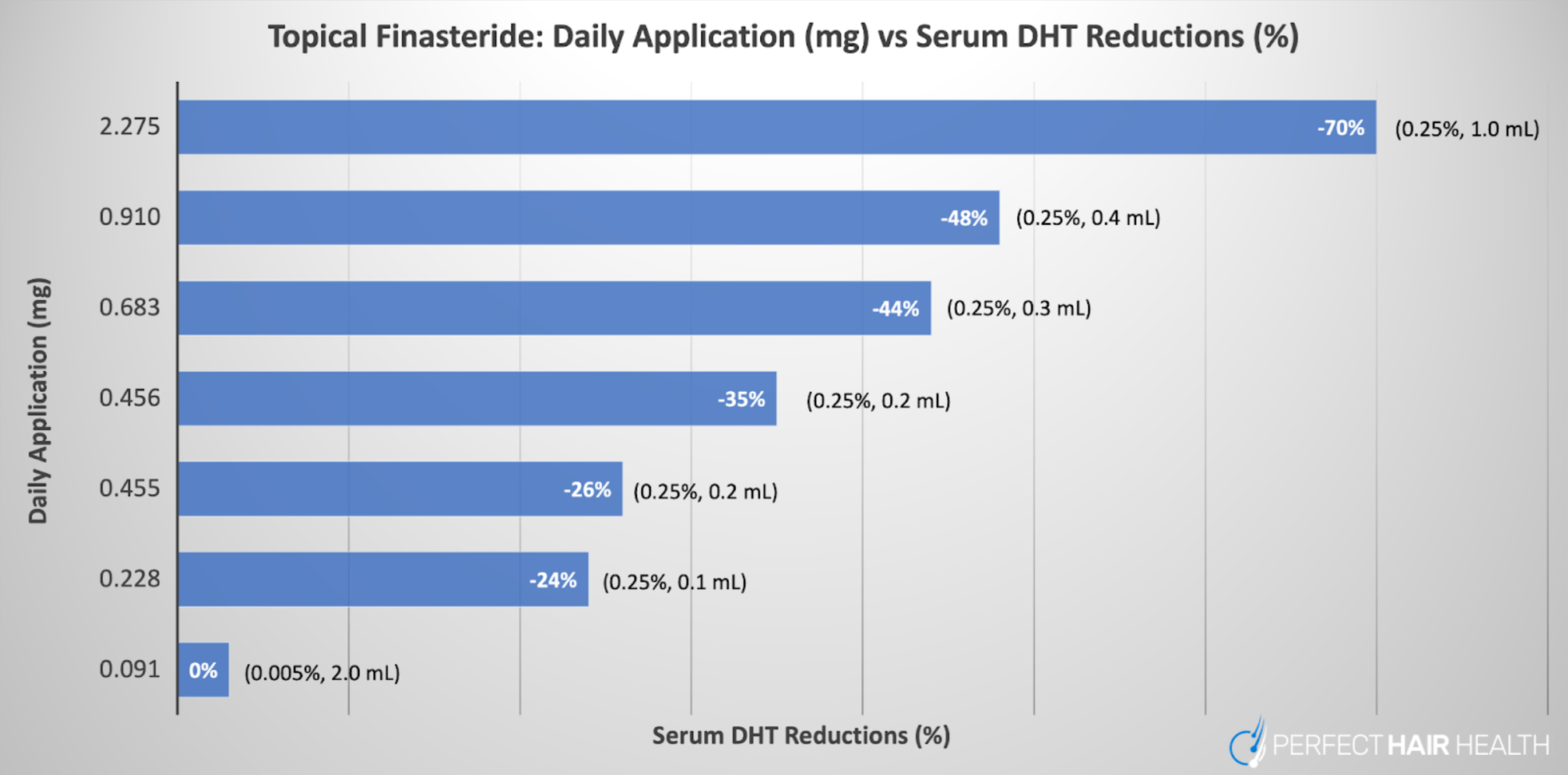
In that regard, see this figure from a 2014 study measuring the effects of one versus two applications of 1 mL of 0.25% topical finasteride on serum DHT levels. [3]https://pubmed.ncbi.nlm.nih.gov/25074865
Caserini, M., Radicioni, M., Leuratti, C., Annoni, O., & Palmieri, R. (2014). A novel finasteride 0.25% topical solution for androgenetic alopecia: pharmacokinetics and effects on plasma androgen levels in healthy male volunteers. International journal of clinical pharmacology and therapeutics, 52(10), 842–849.
Six hours after applying 1 mL or 2 mL applications of 0.25% topical finasteride (2.275-4.550 mg of finasteride), serum DHT reductions flatline. This means that for the 2 mL application group (the black circle with a dotted line), there was enough systemic absorption by the 6-hour mark to effectively lower serum DHT levels as much as they would normally lower with 1 mg of oral finasteride.
Keep in mind that finasteride has an upper limit for its effects on serum DHT reduction. After hitting ~70% reduction in serum DHT, more finasteride doesn’t reduce serum DHT. The same is true with scalp DHT reductions.
So, the above study shows that with topical finasteride applications of 2.275 mg or higher in a hydroxypropyl chitosan delivery vehicle, systemic reductions in DHT equal that of 1 mg of oral finasteride. And with topical finasteride, since serum DHT reductions are sort of like “canaries in the coal mine” for scalp DHT reduction, we can take an educated guess that 6-12 hours after applying topical finasteride. There’s likely enough percutaneous absorption to therapeutically lower scalp DHT levels for hair regrowth.
This is corroborated by a 1997 study suggesting that 2 mL daily of 0.005% topical finasteride (0.0912 mg of finasteride exposure) improved hair parameters for men with AGA and without affecting serum DHT levels – even after 16 months of treatment. [4]https://www.tandfonline.com/doi/abs/10.3109/09546639709160517
Taken together, all of the above evidence signals that, depending on the exposure level, 6-12 hours of exposure to topical finasteride should be enough to have a therapeutic effect on scalp DHT reductions (and hair growth).
Do these time windows apply to all topical finasteride formulations?
No. Obviously, the contact time required for topical finasteride to be effective depends on a number of factors:
- The finasteride dilution (i.e., 0.01% vs. 0.1% topical finasteride)
- The volume of topical applied (i.e., 1 mL vs. 2 mL)
- The topical’s carrier ingredients (i.e., hydroxypropyl chitosan vs. ethanol vs. propylene glycol vs. liposomes)
- The frequency of application (i.e., once-daily, twice-daily, every-other-day, etc.)
Nonetheless, a 6-12 hour contact window should allow for therapeutic efficacy of many big-brand topical finasteride formulations available to consumers currently. However, if you’d like to get specific about adjustments on an individual basis, we offer that level of support inside our membership community.
Final Thoughts
For the most part, occasional incidental exposure to topical finasteride should not cause problems for household members. With that said, there are certain groups at an elevated risk – particularly pregnant women and children – and in these groups, cumulative risk over a lifetime of incidental topical finasteride exposure has yet to be studied.
If this is a concern for you, men and women can minimize the risk of incidental drug exposure from topical finasteride by doing any (or all) of the following:
- Avoiding all physical contact with the scalp for at least 30 minutes after topical finasteride application (so that it fully dries)
- Dedicating a pillowcase to the topical finasteride user, and washing that pillowcase weekly
- Wearing a loosely-fitting shower cap to bed
- Timing topical finasteride applications to 6-12 hour windows where the user is out-of-the-house and/or unlikely to come into contact with household members
Using the evidence and strategies above, our hope is that topical finasteride users can minimize or even eliminate the risk of incidental exposure, all while preserving their hair gains.
References[+]
Fluridil: Scientific Deep-Dive
Fluridil, otherwise known as topilutamide (or by the brand name Eucapil) is a topical medication that has been tested as a treatment for both androgenetic hair loss and hirsutism (excess facial hair growth in women). In 2021, the patent for fluridil expired, however, there have been no generic fluridil treatments that have come to the market. Fluridil has been approved for cosmetic use in Europe but does not have FDA or EMA approval as a treatment for androgenetic alopecia. You can however buy this product on shopping websites, such as Amazon, for around $83 (at the time of writing). But is fluridil worth your money?
In this article, we will look at how Fluridil works, what the clinical evidence for it is, and whether it is safe to use.
Key Takeaways
-
- Drug. Fluridil is an anti-androgenic drug that is currently on the market for the treatment of androgenetic alopecia and hirsutism. It is known to reduce the gene expression of androgens. Due to its similar structure to other anti-androgens, it’s thought to also exert its effect by binding to androgen receptors. As it readily breaks down in aqueous solutions, some researchers believe that it is safer to use than other anti-androgens, and can be applied locally without the risk of side effects on the rest of the body.
- Clinical Data. There are only two studies that have been completed for fluridil: one on men and one on women.
- The first study was 9 months long and completed on 43 men with diagnosed androgenetic alopecia (AGA) aged between 20-56, in which 2mls of 2% fluridil was topically applied once nightly. Researchers found that in the first 3 months, there was a significant increase in the number of growing hairs, and a significant decrease in the number of non-growing hair, with no effects on testosterone levels or perceived sexual libido and function. Furthermore, fluridil, or its by-products, was not found to be present in the serum. Researchers also found, however, that the positive effects on the number of growing hairs/non-growing hairs did not last past the 3-month mark, and were instead maintained. A small safety study completed alongside this determined that either 2% or 4% fluridil was ok to use without adverse effects.
- The second study was 9 months long and only completed on 11 women, 2 of which had to drop out of the study due to adverse effects from the isopropanol that the fluridil was diluted in. The participants applied 2mls of 2% fluridil, once nightly. The researchers did not find any significant change in growing or non-growing hairs, however, they did measure an increase in hair thickness. Due to the small sample size, the lack of a placebo, and the fact that every participant had taken another anti-androgenic medication within 3 months of the beginning of the study, it’s not possible to conclude whether fluridil has any effect or not for women with AGA.
- Safety. Unlike oral anti-androgenic drugs, fluridil should only work at the point of application as it should break down once it comes into contact with the blood. Additionally, across the limited parameters of both the studies mentioned above, no serious adverse effects were reported, however as both of the studies were 9 months long, with small sample sizes, we have no real information about what the long-term effects of fluridil usage may be.
- Best Practices. Based on the limited clinical data, if you decide to use fluridil, you could apply 2ml of a 2% fluridil solution in isopropanol once, at night before bed on a dry scalp (it will degrade if your hair or scalp is wet). You might be a candidate for fluridil if you are male with AGA (as the data isn’t sufficient for females with AGA), are comfortable with using a product that has very limited efficacy or safety data, have potentially seen results using other anti-androgens (such as finasteride), and don’t mind limiting hair washing to once or twice a week. If you’re interested in trying fluridil, although it’s not approved by the FDA, you can buy it on shopping sites like Amazon, and it’s possible that you may see limited results, at least over the first 3 months of usage.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is Fluridil?
As mentioned above, fluridil is a topical treatment that has been used in studies to determine its efficacy and safety in hair loss and excessive hair growth in women (hirsutism).
Fluridil was synthesized alongside four other compounds in a study designed to discover a novel, topical anti-androgenic compound. [1]Seligson, A.L., Campion, B.K., Brown, J.W., Terry, R.C., Kucerova, R., Bienova, M., Hajduch, M., Sovak, M. (2003). Development of Fluridil, a Topical Suppressor of the Androgen Receptor in … Continue reading Androgens are linked to certain types of hair loss such as androgenetic alopecia.
The researchers were also searching for a compound that rapidly degraded (broken down) into non-harmful by-products in the blood so that it does not have effects at the systemic (whole-body) level (but rather limits its activity locally to the area of application). Out of the five total compounds synthesized, the researchers determined that fluridil best fit their criteria, which are described below:
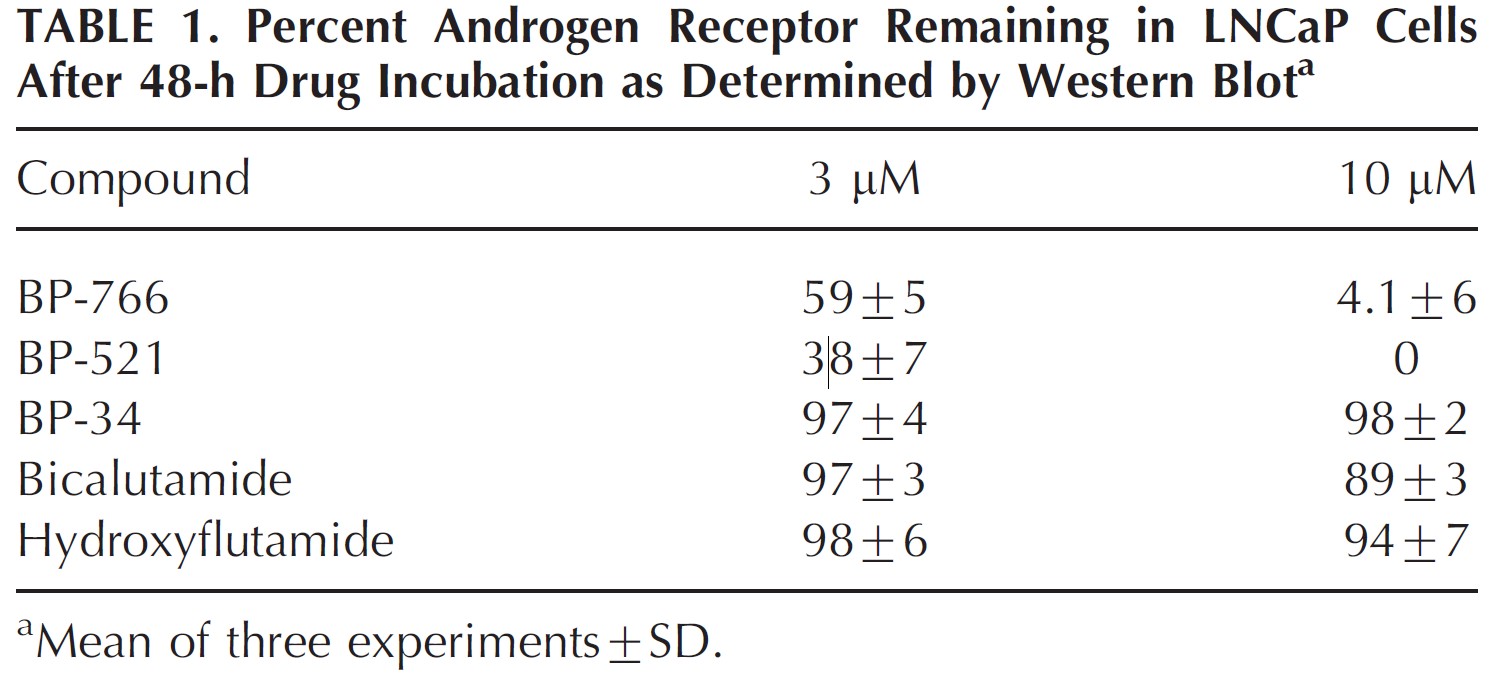
1. Down-regulation of androgen receptors
The growth of prostate cancer is often androgen receptor-dependent.[2]Fujita, K., Nonomura, N. (2019). Role of Androgen Receptor in Prostate Cancer: A Review. The World Journal of Men’s Health. 37(3), 288-295. Available at: https://doi.org/10.5534/wjmh.180040Therefore treating prostate cancer cells in a dish can be a useful way of seeing whether drugs have any anti-androgen receptor activity. In the human prostate cancer cell line LNCaP, fluridil reduced protein expression of androgen receptors by 40% at a concentration of 3μM, and by up to 95% at a 10μM concentration (Figure 1). Whilst this was not the most effective result, (BP-521 further reduced expression), it was the combination of this and results shown further down (Figure 2) that led the researchers to choose fluridil. Additionally, these compounds were compared to two other anti-androgen drugs (bicalutamide and hydroxyflutamide) and found that they did not decrease the expression of androgen receptors, indicating an additional mechanism of action of fluridil that other anti-androgen drugs may not have.
Figure 1: Reduction of protein expression of androgen receptors after 48 hours of drug incubation. BP-766 = fluridil. Adapted from: [3]Seligson, A.L., Campion, B.K., Brown, J.W., Terry, R.C., Kucerova, R., Bienova, M., Hajduch, M., Sovak, M. (2003). Development of Fluridil, a Topical Suppressor of the Androgen Receptor in … Continue reading
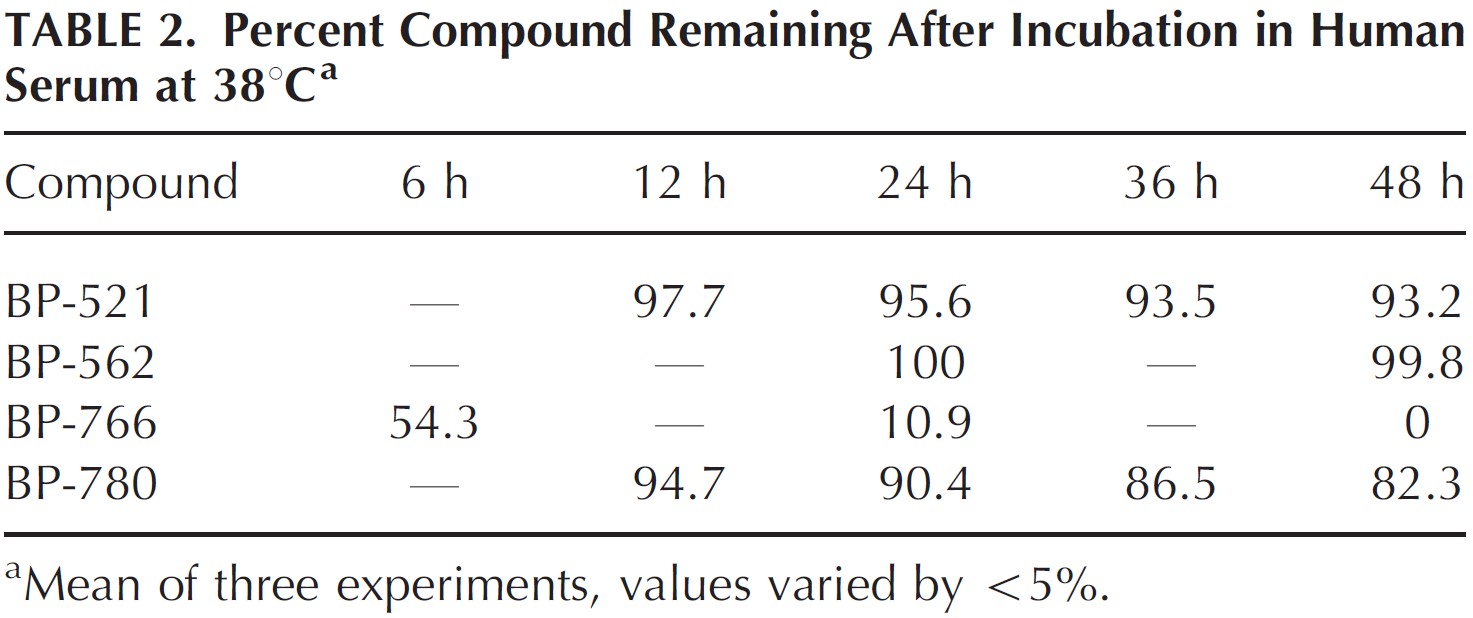
2. Degradation of the compound after incubation in human serum at 38°C
Fluridil was found to be the only compound that fully degraded in human serum by 48h of incubation (Figure 2). By contrast, BP-521, the compound that showed better down-regulation of androgen receptors barely showed any degradation, so did not match the criteria set by the researchers.
Fluridil degrades into BP-34 which – as the researchers show in Figure 1 – doesn’t have a large effect on the expression of androgen receptors. It also degrades into a perfluorocarboxylic acid (PFCA) called trifluoroacetic acid (TFA) which mammals are thought to be insensitive to. [4]Solomon, K., Velders, G., Wilson, S., MAdronich, S., Longstreth, J., Aucamp, P., Bornman, J. (2016). Sources, Fates, Toxicity and Risks of Trifluoroacetic Acid and its Salts: Relevance to Substances … Continue reading
The researchers state that the by-products are non-toxic and that they should be processed rapidly by the kidneys because they are ionic. Ionic substances are attracted to water molecules and undergo dissociation, where they disperse throughout the water, and can therefore be excreted in the urine.[5]Urine pH. (no date). University of Nottingham. Available at: https://www.nottingham.ac.uk/nmp/sonet/rlos/bioproc/kidneydrug/page_six.html (Accessed: 22 January 2022)
Figure 2: Percentage of compound remaining in human serum after incubation at 38°C. BP-766=fluridil. Adapted from:[6]Seligson, A.L., Campion, B.K., Brown, J.W., Terry, R.C., Kucerova, R., Bienova, M., Hajduch, M., Sovak, M. (2003). Development of Fluridil, a Topical Suppressor of the Androgen Receptor in … Continue reading
The researchers determined that based on their criteria, fluridil was the most promising in terms of its capacity to reduce androgen expression and due to its short half-life in aqueous solutions. This study however did not look at the efficacy of fluridil in the context of hair loss, and also did not provide data that established its safety in humans.
How does Fluridil work?
Androgenetic alopecia (AGA) is a form of hair loss with causes not yet fully understood, however, it is thought to be related to either excess androgens present, or an exaggerated response to androgens such as dihydrotestosterone (DHT). It affects both men and women and is characterized by progressive loss of hair over time in a particular pattern.[7]Ho, C.H., Sood, T., Zito, PM. (2022). Androgenetic Alopecia. StatPearls [Internet]. Treasure Island (FL). Available at: https://www.ncbi.nlm.nih.gov/books/NBK430924/. (Accessed: 22 January 2023)
Fluridil belongs to a class of drugs known as non-steroidal anti-androgens (NSAAs). NSAAs are chemicals that stop androgens (like testosterone and DHT) from binding to their receptors. This means that androgens then can’t exert their effects, as they need to bind to these receptors to initiate the signaling events that can lead to hair follicle miniaturization, amongst other things. NSAAs may also be called androgen receptor antagonists, or androgen receptor blockers. [8]Iverson, P., Melezinek, I., Schmidt, A. (2002). Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function. BJUI … Continue reading [9]Ustuner, E.T. (2013). Cause of Androgenic Alopecia: Crux of the Matter. Plastic and Reconstructive Surgery. Global Open. 1(7), e64. Available at: https://doi.org/10.1097/GOX.0000000000000005
Receptors are specialized proteins in cells that allow specific chemicals to bind to them. In response to the correct chemical binding to the receptor, the receptor can exert downstream effects that have an impact on biology (a process known as signal transduction).[10]Miller, E.J., Lappin, S.L. (2022). Physiology, Cellular Receptor. StatPearls [Internet]. Treasure Island (FL). Available at: https://www.ncbi.nlm.nih.gov/books/NBK554403/#_NBK554403_pubdet_ … Continue reading Other NSAAs include flutamide and bicalutamide.
It’s important to note that there have been no studies to determine if this is really how fluridil works. Researchers have stated that this is because of fluridil’s instability in aqueous environments (meaning it is difficult to store, handle, and therefore study). Researchers hypothesize that because its structure is similar to other NSAAs, it has a similar mechanism of action, in addition to its ability to reduce the expression of androgen receptors. [11]Seligson, A.L., Campion, B.K., Brown, J.W., Terry, R.C., Kucerova, R., Bienova, M., Hajduch, M., Sovak, M. (2003). Development of Fluridil, a Topical Suppressor of the Androgen Receptor in … Continue reading
So, how fluridil actually works has not been fully determined, but is there any information on if and how fluridil affects hair follicles?
How can Fluridil have an impact on hair follicles?
Other than what has been hypothesized above (fluridil may be an androgen receptor inhibitor), it is not possible to know for sure exactly how fluridil might work on the hair follicle. As mentioned, there have been no studies in cells or isolated hair follicles in a dish (which may be due to fluridil being unstable in aqueous environments). Cells and isolated hair follicles require physiological media solutions that contain all the nutrients needed to survive and grow, creating a barrier in experimentation with this drug/to experiment with this drug.
Furthermore, the only work completed on animals was in the initial paper in which the researchers completed skin irritant tests and absorption tests, where they found that fluridil was non-irritant at a concentration of 2% (the concentration at which they sell the product, although they don’t mention whether it’s weight/volume or volume/volume) and that there was no fluridil (or its by-products) detected in rabbit serum after a 1% solution was applied twice daily for 10 days. Samples were collected at 2, 5, 21, and 48 hours after treatment and then once every other day for the next 3 days. [12]Seligson, A.L., Campion, B.K., Brown, J.W., Terry, R.C., Kucerova, R., Bienova, M., Hajduch, M., Sovak, M. (2003). Development of Fluridil, a Topical Suppressor of the Androgen Receptor in … Continue reading
The most important thing however is whether, in humans, fluridil actually works and is safe to use. There have been two studies using fluridil in humans diagnosed with androgenetic alopecia. So let’s see if, regardless of knowing exactly how fluridil works, it is effective at treating hair loss.
Is Fluridil effective at treating hair loss?
There are currently only two studies that look at the efficacy and safety of fluridil in humans.
Study 1
The first study was a randomized, double-blind study to determine the efficacy and safety of a topical 2% fluridil solution on 43 men between 20-56 years of age with diagnosed AGA. [13]Sovak, M., Seligson, A.L., Kucerova, R., Bienova, M., Hajduch, M., Bucek, M. (2002).Fluridil, a Rationally Designed Topical Agent for Androgenetic Alopecia: First Clinical Experience. American … Continue reading Fluridil was dissolved in isopropanol to make the solution, because of its instability in water-based liquids. The participants were randomly assigned into two groups, 23 receiving the fluridil, and 20 receiving a placebo of just isopropanol. Participants were required to apply the fluridil or the placebo solution once nightly before bed, to avoid direct sun exposure and to only wash hair a maximum of twice a week using warm water.
After 3 months, the study then became open-label (all participants knew what they were receiving) and all participants began receiving the 2% fluridil solution with a further follow-up 6 months later (so the study was a total of 9 months long).
Data was collected through:
- Phototrichogram – an area of the hair is shaved (1.1cm2) and then photographed using a digital camera. Individual hairs/follicles are counted at baseline and at specific time points throughout.
- Calculating the ratio of growing (anagen) to non-growing (telogen) hairs.
- Global scalp imaging – photographs are taken of the entire scalp for subjective comparison.
- Blood collection – for measuring serum testosterone, measuring for the presence of serum fluridil and its by-products, and determining other relevant blood chemistry values.
- Self-perception questionnaire – for sexual function and libido
Results at 3 months
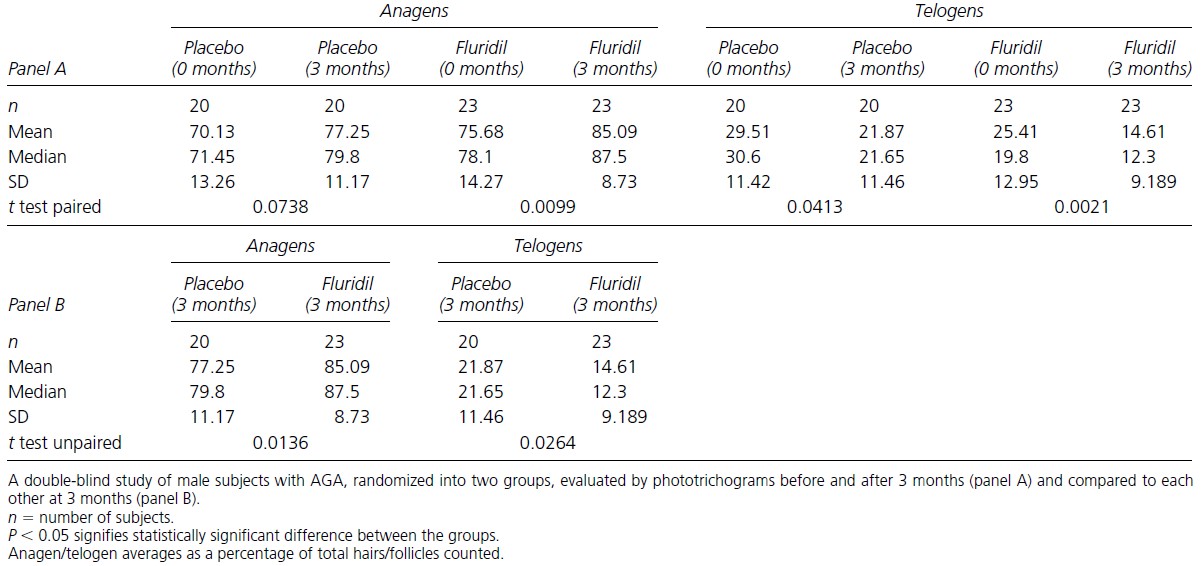
After 3 months, the number of growing to non-growing hairs was compared between the placebo and fluridil groups (Figure 3). The researchers found that the percentage of anagen hairs significantly increased from the baseline in the fluridil-treated group (75.68% at 0 months – 85.09% at 3 months) and the percentage of telogen hairs significantly decreased (25.41% at 0 months -14.61% at 3 months). The placebo group, however, also showed a significant decrease in the percentage of telogen hairs, however (29.51% at 0 months – 21.87 at 3 months) as well.
When comparing the fluridil-treated group to the placebo group after 3 months of treatment, the percentage of anagen hairs was higher in the fluridil (85.09% and 77.25% respectively). Furthermore, there were fewer telogen hairs in the fluridil-treated group than in the placebo group (14.61% and 21.87% respectively).
Figure 3: Effect of fluridil and placebo on the percentage of growing/non-growing hairs after 3 months. (a) Comparing baseline to 3 months of treatment, (b) Comparing fluridil treated to placebo after 3 months. Adapted from:[14]Sovak, M., Seligson, A.L., Kucerova, R., Bienova, M., Hajduch, M., Bucek, M. (2002).Fluridil, a Rationally Designed Topical Agent for Androgenetic Alopecia: First Clinical Experience. American … Continue reading
At this point, the researchers decided that the effects of fluridil on hair growth were significant enough to change all participants to the treated group. It would however have been useful for the researchers to have stated what percentage of participants did see a positive effect.
Results at 9 months
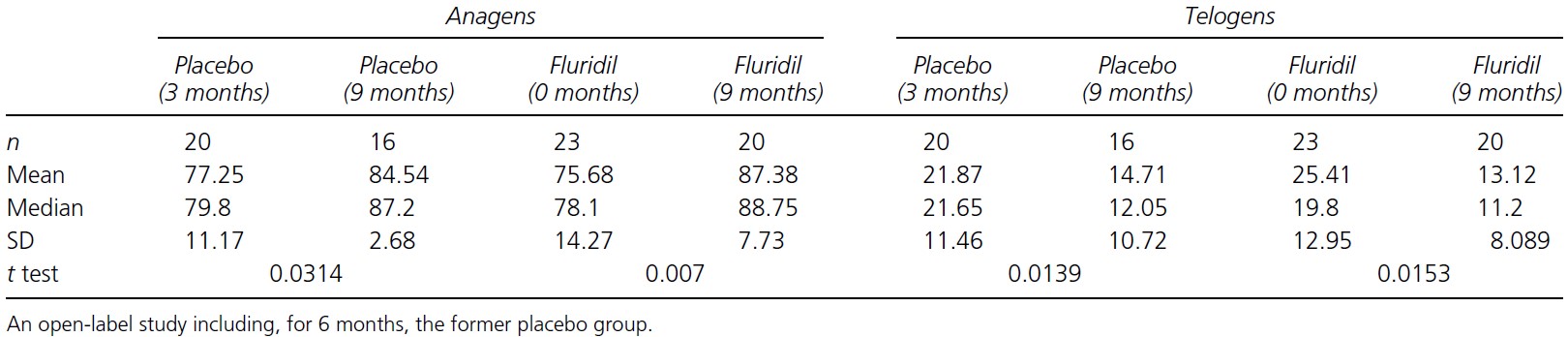
To keep us all on track, by the end of the 9 months, the fluridil-treated group will have been using fluridil for 9 months, and the placebo group will have used the placebo for 3 months and then fluridil for 6 months. We’ll call the placebo group the ‘former placebo’ group now.
After counting growing and non-growing hairs, the researchers found that all groups now experienced significant increases in anagen hairs, and significant reductions in telogen hairs (Figure 4).
Figure 4: Effect of fluridil on the percentage of growing/non-growing hairs after 9 months. Comparing measurements taken at 3 months and 9 months for the former placebo group. Comparing measurements at baseline and 9 months for the fluridil-treated group. Adapted from:[15]Sovak, M., Seligson, A.L., Kucerova, R., Bienova, M., Hajduch, M., Bucek, M. (2002).Fluridil, a Rationally Designed Topical Agent for Androgenetic Alopecia: First Clinical Experience. American … Continue reading
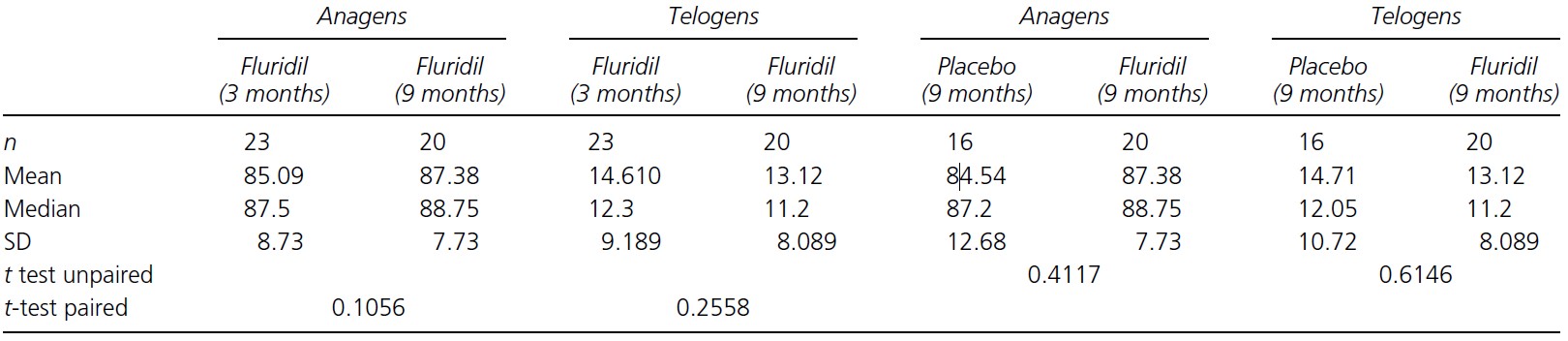
The researchers then compared the changes in growing and non-growing hairs after 3 months and 9 months for the fluridil-treated group and found that there were no significant differences, which indicates that there may be a limit to the effect that fluridil can have on hair growth, and that this limit might be achieved only within the first 3 months. Fluridil however did appear to maintain the number of growing/non-growing hairs after that.
Figure 5: Comparing growing/non-growing hair counts at 3 months and 9 months of treatment for the fluridil group. Comparing growing/non-growing hair counts at 9 months of treatment for the fluridil and former placebo groups. Adapted from: [16]Sovak, M., Seligson, A.L., Kucerova, R., Bienova, M., Hajduch, M., Bucek, M. (2002).Fluridil, a Rationally Designed Topical Agent for Androgenetic Alopecia: First Clinical Experience. American … Continue reading
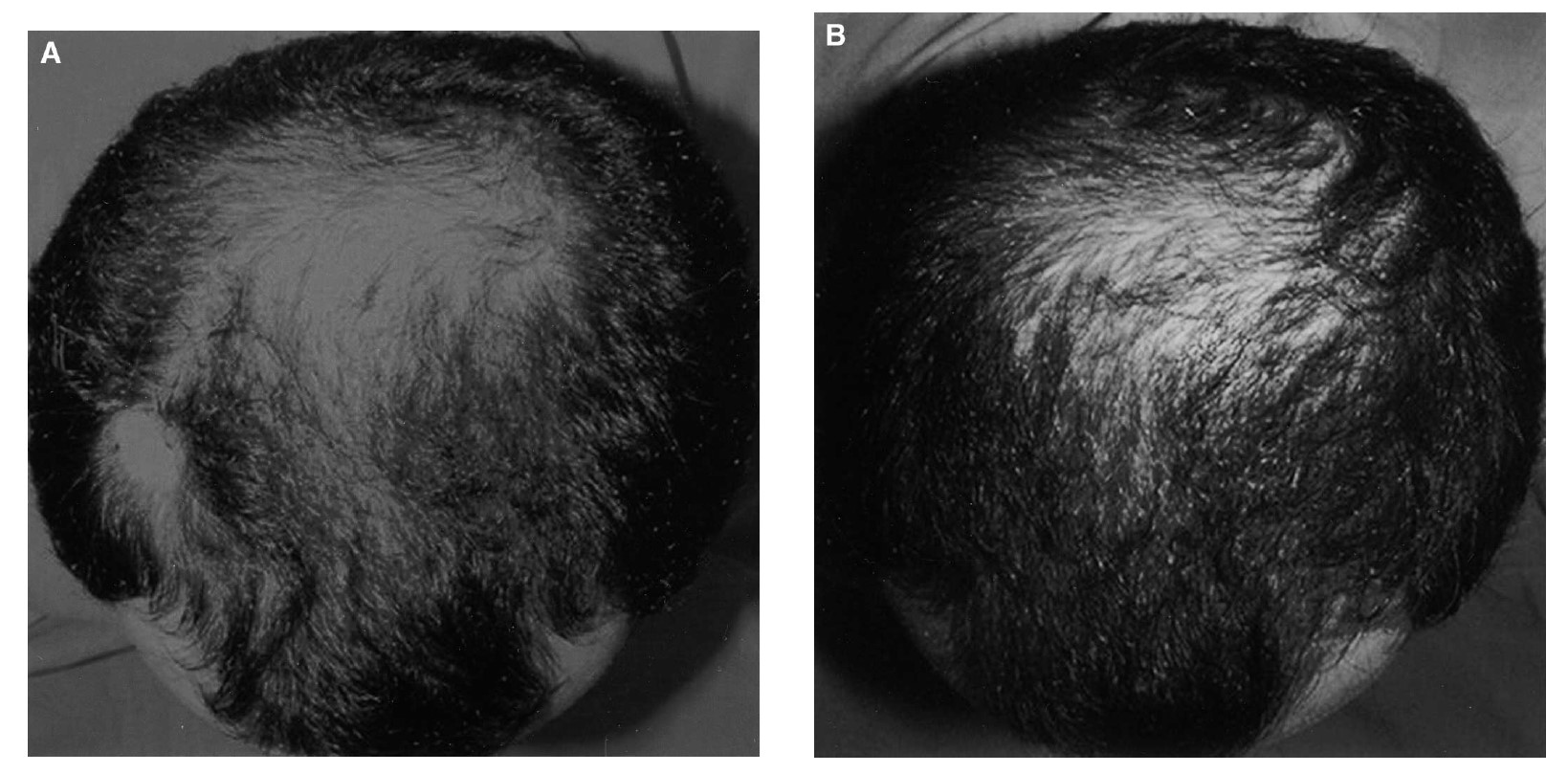
Let’s have a look at before-and-after images to see if this improvement shown in the data actually correlates to a visual improvement. Unfortunately, there is only one image shown (Figure 6), and we are left to wonder if this was the best case and if the reason that the others weren’t shown was that it was more difficult to see the improvements. Furthermore, there are no photos shown of anyone from the placebo group, so we cannot compare between groups.
Figure 6: Before-and afters (A-B) of a participant from the fluridil-treated group at A. Day 0 and B. 6-month time-points. Adapted from: [17]Sovak, M., Seligson, A.L., Kucerova, R., Bienova, M., Hajduch, M., Bucek, M. (2002).Fluridil, a Rationally Designed Topical Agent for Androgenetic Alopecia: First Clinical Experience. American … Continue reading
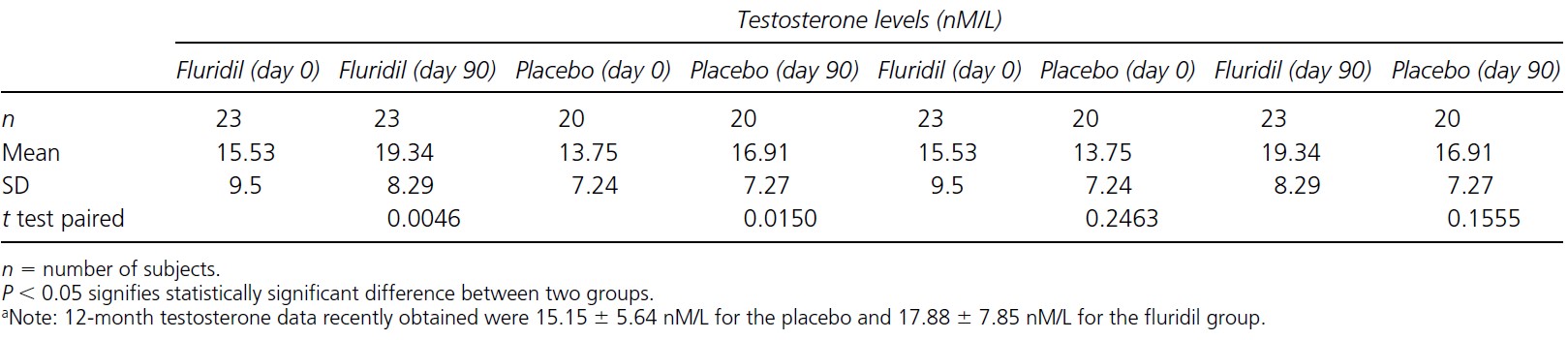
Other than measuring the number of growing/non-growing hairs, serum testosterone levels were also measured. Whilst variation between participants was observed, testosterone levels remained between the physiological range of 8-35 nm/L (Figure 7). Questionnaires also determined that participants did not experience any changes to libido or sexual performance either, however, it is not stated at what time points this data was collected. This is an indication that fluridil can only affect the hair follicle without leading to the systemic side effects that other anti-androgen drugs can cause. Additionally, the researchers did not detect fluridil or its by-product BP-34 in the serum of participants, further lending credence to this hypothesis.
Figure 7: Testosterone levels after treatment with fluridil (comparing baseline to the 90-day mark/comparing 90 days of fluridil to 90 days of the placebo group). Adapted from: [18]Sovak, M., Seligson, A.L., Kucerova, R., Bienova, M., Hajduch, M., Bucek, M. (2002).Fluridil, a Rationally Designed Topical Agent for Androgenetic Alopecia: First Clinical Experience. American … Continue reading
A separate study within the same paper was completed with 20 male participants between the ages of 18-60. Patches containing 2,4, or 6% fluridil in either isopropanol or Vaseline Intensive Care Lotion were applied once a day for 21 days (excluding weekends) to determine if fluridil caused any irritancy to the skin. Isopropanol was also given alone as a control. 2% and 4% fluridil were found to be non-irritant and non-sensitizing. 6% fluridil however caused a slight degree of macular erythema (a rash with flat discolored areas of skin and small raised bumps).
So, to summarize, the data indicates that fluridil treatment leads to more growing hairs and fewer non-growing hairs. This effect however plateaus after 3 months, with no improvement or deterioration occurring after. Fluridil doesn’t appear to affect testosterone levels (which other anti-androgen medications can), and, holding up to the claim of hydrolyzation neither fluridil nor its by-product BP-34 were found to be present in the serum of participants throughout the study. There is only one comparison photo however, and while it does look like there is an improvement, it’s not possible to know if this was just the very best case or whether other participants also experienced a similar level of improvement. Of course, the long-term effects of fluridil (beyond 9-months) are unknown.
Study 2
The second study completed by the same research group was an open study. An open study is a study in which both participants and researchers are aware of what they are using. It sought to determine the efficacy and safety of a 2% fluridil solution in isopropanol on 11 female participants, aged 22-45, with diagnosed AGA. [19]Kucerova, R., Bienova, M., Novotny, R., Fiuraskova, M., Hajduch, M., Sovak, M. (2006). Current Therapies of Female Androgenetic Alopecia and Use of Fluridil, a Novel Topical Antiandrogen, Scripta … Continue reading
Participants were required to massage 2 ml of the fluridil solution into their scalps once a day, in the evening. 2 women discontinued the study due to itching and reddening that developed at the site after treatment. It was determined with an allergy study that this was due to the isopropanol causing irritation, rather than a reaction to the fluridil itself.
Participants were advised to only apply the solution to a dry scalp and to limit hair washes to a maximum of 2 times a week.
In this study, all 11 participants were treated with fluridil, so there was no placebo or a no-treatment group. A placebo group is useful in clinical trials as it provides a group to compare throughout the study. The participants are also aware that they are receiving the actual treatment without a placebo, which may influence the participant’s perception of the effect of the treatment.
Several types of data were collected, including the following methods:
- Phototrichogram
- Global scalp imaging
- Hair Diameter measurement – an area of hair shaved and 3 weeks later ~50 new hairs collected and measured using a microscope.
- Changes in hair surface – five hairs from each patient were collected and prepared for scanning electron microscopy (SEM*).
- Evaluation by a physician (using a scoring system)
- Self-evaluation by participants (using a scoring system) to determine self-perception of hair growth and quality as well as effects on libido and sexual function.
- Blood tests – to measure serum testosterone, sex hormone binding globulin, other relevant blood chemistry, and serum fluridil or its by-products.
*(SEM is a special type of microscope that produces images of a sample by scanning the surface with electrons. These interact with the atoms that make up the sample, creating a much higher resolution image than might be obtained from a light-based camera). [20]Scanning Electron Microscopy. (no date). Nanoscience Instruments. Available at: https://www.nanoscience.com/techniques/scanning-electron-microscopy/ (Accessed: 22 January 2023)
Results
The authors of this study stated that they only included statistically significant data and what they considered to be “otherwise remarkable observations” in their results section.
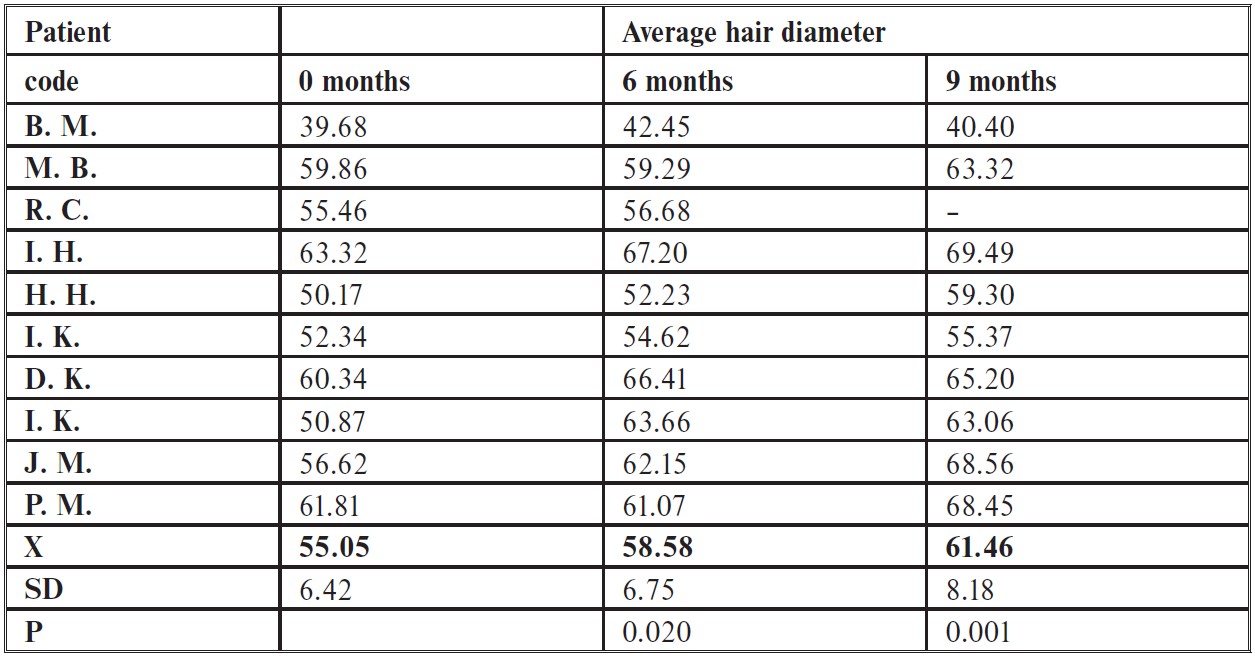
The researchers found that fluridil treatment did not significantly increase the number of growing hairs or decrease the number of non-growing hairs over the whole study period (9 months), however, there was a significant improvement in hair diameter when it was measured at the 6 months and 9-month marks compared to the baseline. Whilst there are no images included in this paper, it is mentioned that the SEM images showed no changes in the overall morphology of the hair and that after evaluating global scalp images (photos taken from the top of the head) hair appeared to be thicker.
Figure 8: Hair diameter measurements and baseline, 6 months, and 9 months. Adapted from: [21]Kucerova, R., Bienova, M., Novotny, R., Fiuraskova, M., Hajduch, M., Sovak, M. (2006). Current Therapies of Female Androgenetic Alopecia and Use of Fluridil, a Novel Topical Antiandrogen, Scripta … Continue reading
5 out of 11 participants reported that they perceived themselves to have reduced hair loss after 6 months of treatment. 1 out of 11 participants reported that they perceived their hair to have improved quality after 6 months, with another one reporting the same after 9 months. One person observed thickening of the hair (after 9 months), one reported new undergrowth (after 6 months) and one person reported accelerated hair growth (after 3 months). Undergrowth is the growth of short, fine hairs underneath longer hair.
So, not very convincing. We have measurements of hair diameter thickening but no data showing any increase in growing hairs or reduction in non-growing hairs. Moreover, the reported ‘positive’ data is almost entirely based on subjective patient self-reporting.
The safety data however does generally follow the same results as with the previous study on men, with no patients reporting adverse side effects.
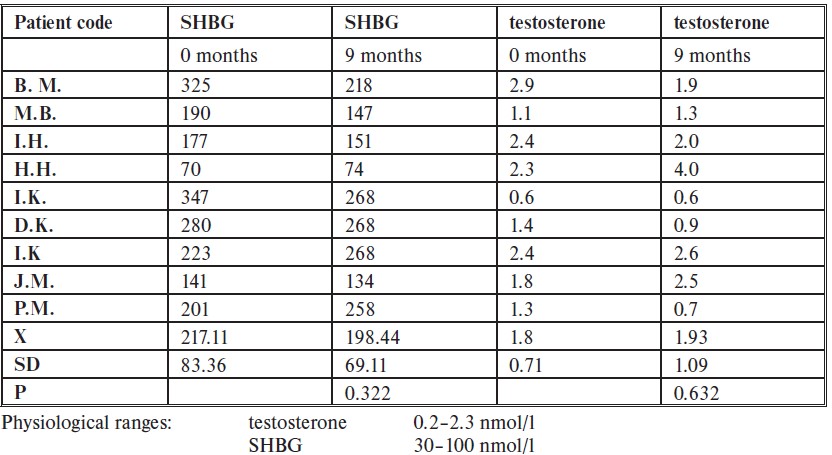
The blood chemistry data was within normal parameters throughout the study (measured at 3, 6, and 9 months) and there was no presence of fluridil or its by-products in the serum of any of the participants.
With regards to testosterone levels and sexual hormone binding globulin (SHBG), the researchers found no statistically significant differences between measurements taken at baseline and 9 months of treatment. There were however patients with higher than the physiological range of SHBG, which has been attributed to the fact that 8 out of 9 of the final patients were taking the combined oral contraceptive pill, which is known to increase SHBG. [22]Amiri, M., Tehrani, F.R., Nahidi, F., Kabir, A., Azizi, F. (2018). Comparing the Effects of Combined Oral Contraceptives Containing Progestins with Low Androgenic and Antiandrogenic Activities on the … Continue reading
Figure 9: SHBG and Testosterone levels at baseline and 9 months. Adapted from: [23]Kucerova, R., Bienova, M., Novotny, R., Fiuraskova, M., Hajduch, M., Sovak, M. (2006). Current Therapies of Female Androgenetic Alopecia and Use of Fluridil, a Novel Topical Antiandrogen, Scripta … Continue reading
So, why didn’t fluridil work in the same way for women as it did for men? Well, the researchers attribute this to the fact that the participants were taking cyproterone acetate (aka Diane 35) another anti-androgen, and (in some cases) contraceptive at least 3 months previous to the study. They determined that because they were taking Diane 35, it can be assumed that there was a sufficient anti-androgenic effect being exerted and so fluridil could not provide a further effect.
But this is just one of several other problems with this study, such as:
- Small participant number
- No placebo
- Participants had been taking medication that may interfere with the efficacy of fluridil
Overall, we cannot conclude that fluridil has any real beneficial effect for women with AGA.
Is Fluridil safe?
Within the limited parameters of the published studies, fluridil doesn’t appear to have any treatment-related side effects. Furthermore, unlike taking oral anti-androgenic medications, fluridil should work only at the point of application and not have effects anywhere else in the body, due to its ability to degrade when it comes into contact with water.
However, fluridil has not been approved by the FDA or the European Medicines Agency as an anti-androgenic medication and is only approved for use in Europe as a cosmetic. The long-term effects of using fluridil are completely unknown.
Is Fluridil for me?
You may want to try fluridil if you:
- Are male with AGA.
- Want to either maintain the current status of hair loss or see short-term improvement and then a plateau.
- Are comfortable with using a product that has no FDA or EMA approval.
- Have no issues using a product that has very little recent (or otherwise) efficacy or safety data.
- Are ok with reducing hair washing to around once or twice a week.
- Have perhaps seen positive results with other anti-androgens (such as finasteride)
Whilst the previously mentioned points (easily degradable and topical application) may prove appealing, we cannot currently recommend using fluridil until more data becomes available. If you want to take the risk, however, it is possible that you may see some limited benefits.
References[+]
References ↑1 Seligson, A.L., Campion, B.K., Brown, J.W., Terry, R.C., Kucerova, R., Bienova, M., Hajduch, M., Sovak, M. (2003). Development of Fluridil, a Topical Suppressor of the Androgen Receptor in Androgenetic Alopecia. Drug Development Research. 59, 292-306. Available at: https://doi.org.10.1002/ddr.10166 ↑2 Fujita, K., Nonomura, N. (2019). Role of Androgen Receptor in Prostate Cancer: A Review. The World Journal of Men’s Health. 37(3), 288-295. Available at: https://doi.org/10.5534/wjmh.180040 ↑3, ↑6, ↑11, ↑12 Seligson, A.L., Campion, B.K., Brown, J.W., Terry, R.C., Kucerova, R., Bienova, M., Hajduch, M., Sovak, M. (2003). Development of Fluridil, a Topical Suppressor of the Androgen Receptor in Androgenetic Alopecia. Drug Development Research. 59, 292-306. Available at: https://doi.org.10.1002/ddr.10166 ↑4 Solomon, K., Velders, G., Wilson, S., MAdronich, S., Longstreth, J., Aucamp, P., Bornman, J. (2016). Sources, Fates, Toxicity and Risks of Trifluoroacetic Acid and its Salts: Relevance to Substances Regulated Under the Montreal and Kyoto Protocols. Journal of Toxicology and Environmental Health. 43(15-16), 597-603. Available at: https://doi.org/10.1080/10937404.2016.1175981 ↑5 Urine pH. (no date). University of Nottingham. Available at: https://www.nottingham.ac.uk/nmp/sonet/rlos/bioproc/kidneydrug/page_six.html (Accessed: 22 January 2022) ↑7 Ho, C.H., Sood, T., Zito, PM. (2022). Androgenetic Alopecia. StatPearls [Internet]. Treasure Island (FL). Available at: https://www.ncbi.nlm.nih.gov/books/NBK430924/. (Accessed: 22 January 2023) ↑8 Iverson, P., Melezinek, I., Schmidt, A. (2002). Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function. BJUI International. 87(1), 47-56. Available at: https://doi.org/10.1046/j.1464-410x.2001.00988.x ↑9 Ustuner, E.T. (2013). Cause of Androgenic Alopecia: Crux of the Matter. Plastic and Reconstructive Surgery. Global Open. 1(7), e64. Available at: https://doi.org/10.1097/GOX.0000000000000005 ↑10 Miller, E.J., Lappin, S.L. (2022). Physiology, Cellular Receptor. StatPearls [Internet]. Treasure Island (FL). Available at: https://www.ncbi.nlm.nih.gov/books/NBK554403/#_NBK554403_pubdet_ (Accessed: 22 January 2023) ↑13, ↑14, ↑15, ↑16, ↑17, ↑18 Sovak, M., Seligson, A.L., Kucerova, R., Bienova, M., Hajduch, M., Bucek, M. (2002).Fluridil, a Rationally Designed Topical Agent for Androgenetic Alopecia: First Clinical Experience. American Society for Dermatologic Surgery. 28, 678-685. https://doi.org/10.1046/j.1524-4725.2002.02017.x ↑19 Kucerova, R., Bienova, M., Novotny, R., Fiuraskova, M., Hajduch, M., Sovak, M. (2006). Current Therapies of Female Androgenetic Alopecia and Use of Fluridil, a Novel Topical Antiandrogen, Scripta Medica (Brno). 79(1), 35-48 ↑20 Scanning Electron Microscopy. (no date). Nanoscience Instruments. Available at: https://www.nanoscience.com/techniques/scanning-electron-microscopy/ (Accessed: 22 January 2023) ↑21, ↑23 Kucerova, R., Bienova, M., Novotny, R., Fiuraskova, M., Hajduch, M., Sovak, M. (2006). Current Therapies of Female Androgenetic Alopecia and Use of Fluridil, a Novel Topical Antiandrogen, Scripta Medica (Brno). 79(1), 35-48 ↑22 Amiri, M., Tehrani, F.R., Nahidi, F., Kabir, A., Azizi, F. (2018). Comparing the Effects of Combined Oral Contraceptives Containing Progestins with Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis in Patients with Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis. JMIR Research Protocols, 7(4), e113. https://doi.org/10.2196/resprot.9024 Topical minoxidil is an FDA-approved treatment for male and female pattern hair loss, also known as androgenic alopecia (AGA).
Despite its popularity, not very many people continue using topical minoxidil for the long-run. In fact, one clinical study found that by the one-year mark, 95% of topical minoxidil users voluntarily quit applying the drug – with more than 2/3rds of them citing “low effect” as their rationale.[1]https://pubmed.ncbi.nlm.nih.gov/17917938/
So, what sort of hair regrowth can we expect from minoxidil? Why do so many people quit using the topical? And what can we do to maximize minoxidil’s hair growth-promoting effects, and in doing so, set ourselves up for sustainable hair regrowth years into the future?
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Is Minoxidil?
Topical minoxidil is the only medication approved by the FDA for the treatment of androgenic alopecia (AGA) in both males and females. Since its use as an anti-hypertensive drug in 1979, researchers have long-noted a nearly universal “adverse event” in oral minoxidil users: unexpected new hair growth along the limbs, chest, face, and scalp.[2]https://pubmed.ncbi.nlm.nih.gov/7030707/
This led to to the reformulation of minoxidil as a topical, and subsequent clinical trials to test its efficacy on treating AGA. In 1988 and 1992, 5% and 2% minoxidil became commercial available as an over-the-counter hair growth treatment for men and women, respectively.
How Does Minoxidil Work?
Researchers aren’t totally sure how minoxidil regrows hair.
Having said that, they suspect that minoxidil may work through at least one (or all) of the following mechanisms:
- Opening potassium ion channels – which increases blood, oxygen, and nutrient transport to balding regions (i.e., increased microcirculation)
- Modulation of prostaglandin analogues (i.e., decreased inflammation)
- Anti-androgenic activity in hair follicle sites (i.e., decreased dihydrotestosterone (DHT) – the hormone causally linked to baldness).
How Much Regrowth Should We Expect From Minoxidil?
Technically speaking, “hair regrowth” isn’t a term specific enough to be meaningful. Are we talking about changes to total hair counts? Changes to hair thicknesses? Increases to terminal hairs? Vellus hairs? Hair density changes? Over what time period: 1 month, 3 months, 5 years? What about the percentage of people who notice increased hair growth versus those who don’t?
Depending on how we define “hair regrowth”, our answers will vary wildly.
For these reasons, our team prefers to use more specific language surrounding hair regrowth. Here are the two metrics we tend to consider most important when evaluating the efficacy of a hair loss treatment option:
- Response Rate. This term can be defined through a question: “Of the people who try this intervention, what percent will see a slowing, stopping, or partial reversal of their hair growth versus a placebo group – and over a reasonable time period?”
- Regrowth Rate. This term’s definition varies depending on the quality of data on an intervention. But in general, it’s the change in an objective hair growth endpoint that closely mirrors the perception of “visual improvements” to hair. For instance, this might be the change in terminal hair counts, hair density (i.e., the ∆ in hair counts x the ∆ in hair thickness), or hair weight (i.e., the difference in the weight of hair shaved off before/after a study was conducted, controlling for hair growth timing).
What Is Minoxidil’s Response Rate?
Despite being an FDA-approved hair growth drug, topical minoxidil’s response rate is as low as 40-60%.[3]https://pubmed.ncbi.nlm.nih.gov/25112173/
This is because topical minoxidil is applied to the scalp as a pro-drug – meaning that it’s inactive. It needs to come into contact with a skin enzyme called sulfotransferase – which is produced by the SULT1A1 gene – in order to active in the skin, and then attach to hair follicles where it can elicit its hair growth-promoting effects.
Unfortunately, upwards of 60% of men and women do not have high enough levels of sulfotransferase in their skin to elicit a response to topical minoxidil.[4]https://pubmed.ncbi.nlm.nih.gov/24283387/
This means that for (potentially) a majority of people who try topical minoxidil, it won’t lead to any hair growth, because not enough of it will activate within the scalp to create an effect on hair growth.
Fortunately, there are ways to enhance minoxidil’s efficacy – and the activity levels of sulfotransferase in the scalp skin. We’ll get into these later in the article.
What Is Minoxidil’s Regrowth Rate?
This depends on a number of factors, including someone’s:
- Gender
- Severity of hair loss
- Genetic variance in the SULT1A1 gene
- The delivery method of minoxidil (oral vs. topical)
- The dosing amount and schedule
- If minoxidil is combined with interventions that might enhance its hair growth-promoting effects (more on this later).
Having said that, if we narrow our definition of Regrowth Rate to changes to “hair weight” occurring over a 1+ year usage period, and we narrow our patient population to healthy men and women who are facing androgenic alopecia, we can use clinical data to set ballpark expectations.
A well-designed study by Price et al. (1999) sought to determine the effect of 2% and 5% topical minoxidil on cumulative hair weight changes throughout 96 weeks of treatment. Compared to the placebo and untreated groups, hair weight changes from 2% and 5% topical minoxidil were 20% and 30% higher for 2% and 5% topical minoxidil users at the 52-week mark, respectively.[5]https://pubmed.ncbi.nlm.nih.gov/10534633/
Here’s a chart summarizing the details (Note: participants withdrew from treatment at the vertical line denoted at week 96):
Price VH, Menefee E, Strauss PC. Changes in hair weight and hair count in men with androgenetic alopecia, after application of 5% and 2% topical minoxidil, placebo, or no treatment. J Am Acad Dermatol. 1999 Nov;41(5 Pt 1):717-21. doi: 10.1016/s0190-9622(99)70006-x. PMID: 10534633.
So, despite that 40-60% of topical minoxidil users don’t respond to treatment, after averaging out all participants’ hair growth results, most studies on topical minoxidil show that overall hair growth results are statistically improved.
This is the big problem with topical minoxidil: its hair growth outcomes are bifurcated.
On the one hand, we have 40-60% of users seeing zero effect from the drug. On the other hand, we have 40-60% of users seeing big amounts of hair growth. These bifurcated results can average a 20-30% cumulative hair weight change at the one-year mark.
Key Takeaway: despite ~50% of people not responding to 2% or 5% topical minoxidil, most studies show statistically significant improvements to hair counts. This is because a subset of participants are often hyper-responders to minoxidil, which bring up the average hair counts for everyone.
Do Minoxidil’s Results Last Long-Term?
Unfortunately, hair regrowth from topical minoxidil is not necessarily as long-lasting as most would hope.
This is because clinical studies also show that, over time, the efficacy of topical minoxidil wanes – meaning that its hair growth-promoting effects diminish over a number of years, even despite keeping users above the placebo group. [6]https://pubmed.ncbi.nlm.nih.gov/12196747/[7]https://pubmed.ncbi.nlm.nih.gov/2180995/
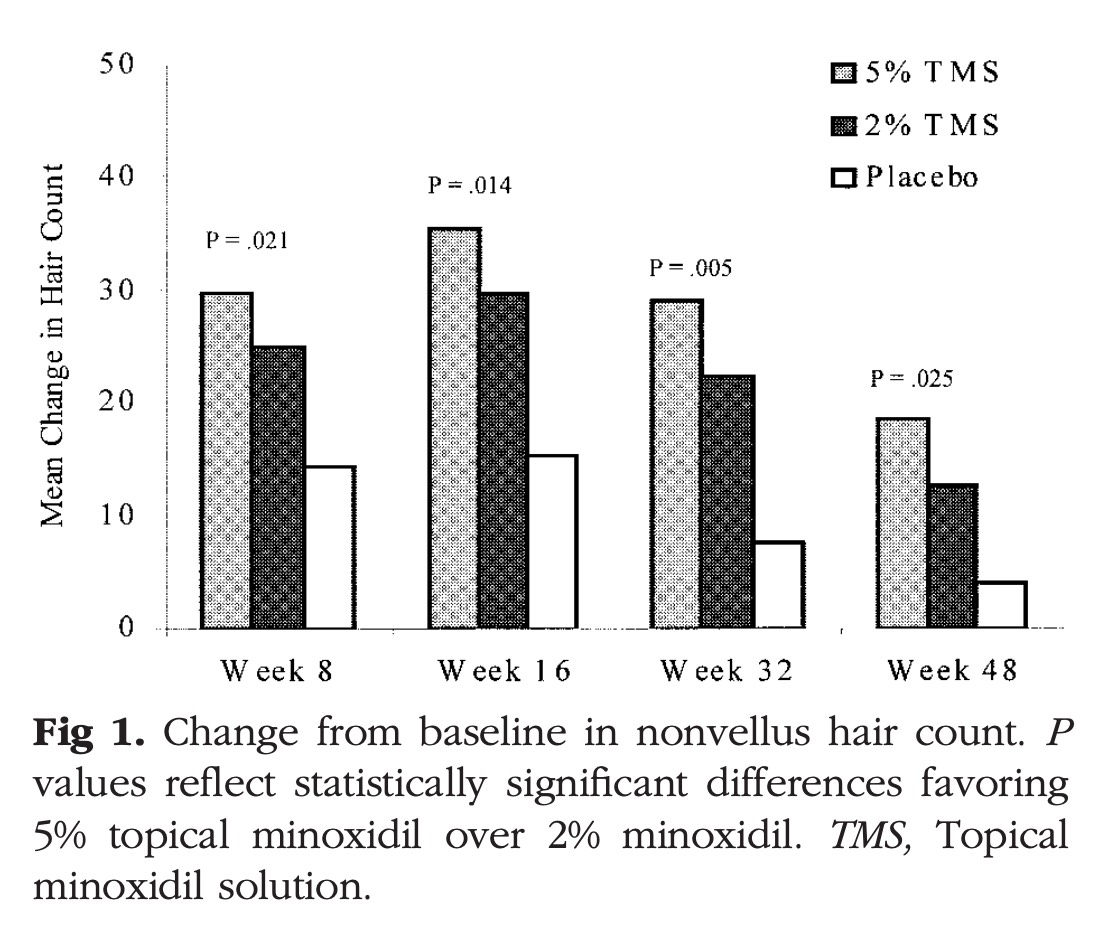
This was already evident in the above study, which showed a trend downward for cumulative changes to hair weights from weeks 52 to 96. And these results are consistent across other studies. Just see the diminishing regrowth results from this 48-week study on 2% and 5% topical minoxidil versus placebo:[8]https://pubmed.ncbi.nlm.nih.gov/12196747/
Olsen, E. A., Dunlap, F. E., Funicella, T., Koperski, J. A., Swinehart, J. M., Tschen, E. H., & Trancik, R. J. (2002). A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. Journal of the American Academy of Dermatology, 47(3), 377–385.
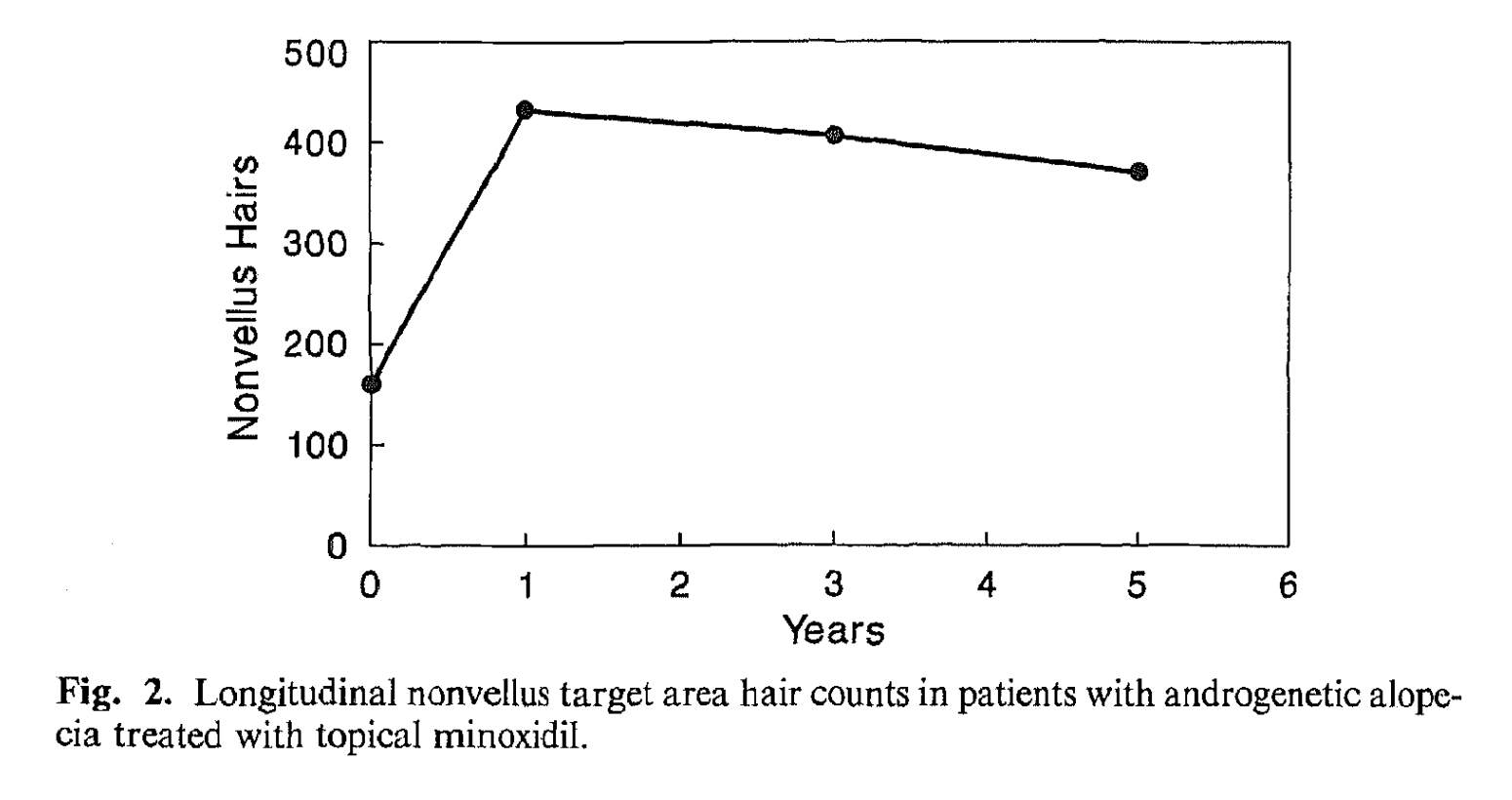
Moreover, here’s a five-year study tracking topical minoxidil’s efficacy, which seems to wane after year one:[9]https://pubmed.ncbi.nlm.nih.gov/2180995/
Olsen, E. A., Weiner, M. S., Amara, I. A., & DeLong, E. R. (1990). Five-year follow-up of men with androgenetic alopecia treated with topical minoxidil. Journal of the American Academy of Dermatology, 22(4), 643–646.
For more information on these topics, see this article: Minoxidil: How Long Do Results Last (Even After Quitting)?
Factors Affecting Topical Minoxidil’s Ability To Grow Hair
To summarize from the above, topical minoxidil has a response rate of just 40-60%. This is because a large number of users lack enough skin activity of an enzyme known as sulfotransferase – which is used to turn minoxidil into minoxidil sulfate, where the drug can then become active, attach to hair follicle sites, and have a positive impact on hair parameters.
But even with these poor response rates, 2% to 5% topical minoxidil still can improve hair weights by 20-30% over a 52-week period – and lead to modest hair count improvements – a portion of which will lead to cosmetically significant improvements to hair.
This is because the 40-60% of people who do respond to topical minoxidil tend to respond relatively robustly.
Factors affecting minoxidil’s response rates and regrowth rates are person-specific, and depend on (at least) the following:
- The person. Age, gender, hair loss severity, and genetic variations in the SULT1A1 gene
- The drug. Delivery methods (i.e., topical versus oral), along with dosing amounts and schedules (i.e., 5% twice-daily)
- Minoxidil enhancers. Whether minoxidil is used alongside therapies that enhance skin penetration and/or sulfotransferase activity (i.e., retinoic acid and/or microneedling)
This begs the question: if we’re worried we may not respond to minoxidil, how can we enhance the drug’s efficacy?
Fortunately, there are a number of ways to take someone from a non-responder to a great responder.
How Can Minoxidil Results Be Improved?
There are a handful of strategies to improve the effectiveness of minoxidil. If you’re looking for a deep-dive into the science, this article is a great resource.
Otherwise, here are the highlights:
- Increase the dilution of topical minoxidil to 15%. Clinical studies show that suspected non-responders to 2% and 5% minoxidil tend to see robust hair regrowth at higher dilutions ranging from 10% to 15% minoxidil.
- Add in minoxidil enhancers. Retinoic acid (i.e., tretinoin) and microneedling both help increase dermal penetration of minoxidil and active more sulfotransferase.
- Switch to oral minoxidil. Unlike topical minoxidil – which gets sulfated in the skin – oral minoxidil goes through processing in the liver whereby most people have an abundance of sulfotransferase to activate the drug. This leads to dramatically higher response rates – with daily doses of 2.5 mg and higher sometimes promoting 90% response rates in clinical trials.
Many people inside our membership community have used these strategies above to move from minoxidil non-responders to minoxidil hyper-responders. We hope they help you, too.
We hope these recommendations help take your hair growth results to a new level.
References[+]
References ↑1 https://pubmed.ncbi.nlm.nih.gov/17917938/ ↑2 https://pubmed.ncbi.nlm.nih.gov/7030707/ ↑3 https://pubmed.ncbi.nlm.nih.gov/25112173/ ↑4 https://pubmed.ncbi.nlm.nih.gov/24283387/ ↑5 https://pubmed.ncbi.nlm.nih.gov/10534633/ ↑6, ↑8 https://pubmed.ncbi.nlm.nih.gov/12196747/ ↑7, ↑9 https://pubmed.ncbi.nlm.nih.gov/2180995/ How Often Does Topical Finasteride Need To Be Applied?
Most clinicians recommend using topical finasteride at least once daily. However, its minimum viable frequency of application depends on factors such as daily drug exposure and contact time with the scalp.
For those who can keep topical finasteride on their scalps for 10-12 hours (or longer), once-daily applications of low-dose topical finasteride might suffice. For those who can only keep topical finasteride on their scalps for 4-6 hour periods, twice-daily applications may be more helpful – or higher-dose topical finasteride.
After maximum drug saturation has occurred in the scalp (typically after ~30 days of daily applications), it is possible to reduce the frequency of use from once daily to five times weekly – and perhaps even lower – while still seeing hair parameter improvements. However, doing so with low-dose finasteride may come with a reduction in efficacy.
More explanations can be found below.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Finasteride: How Much Is Enough To Regrow Hair?
Clinical studies have demonstrated a steep, dose-dependent, logarithmic response curve for finasteride’s effects on DHT levels. In other words, a little finasteride reduces almost as much DHT as a lot of finasteride. See this chart:
Clinical studies also show that topical formulations of topical finasteride as low as 0.005% x 1 mL, applied twice daily, can improve hair parameters over 16-month periods.[1]https://www.tandfonline.com/doi/abs/10.3109/09546639709160517
That’s a total daily exposure volume of just 0.1mg daily – or one-tenth that of what is prescribed orally on a daily basis to treat androgenic alopecia (AGA). Needless to say, people with localized hair loss (i.e., just at temples and/or crown) may be able to switch to topical finasteride, reduce their drug exposure, and still see impressive hair growth-promoting effects.
Can Topical Finasteride Be Used Every Other Day?
While usage frequencies lower than once daily haven’t been clinically studied, it’s likely that topical finasteride would still be effective with less frequent dosing schedules.
Why? Because finasteride has a tissue dissociation timing of 4-5 days. In other words, it takes multiple days (and sometimes weeks) for finasteride bound to skin tissue to finally leave that skin tissue and enter the bloodstream, where it is later metabolized and excreted.
Moreover, clinical studies on 1 mg daily of oral finasteride suggest that after one year of use, switching to a 30-days-on, 30-days-off dosing schedule is just as effective as continuing with a once-daily dosing schedule – despite not using the drug for a total of 6 months throughout the same year.[2]https://jaad.org/retrieve/pii/S0190962220319289
For these reasons, finasteride can still have a therapeutic effect on DHT reduction in the scalp skin, even up to ~30 days after quitting the drug.
This is even reflected in withdrawal studies of oral finasteride, which show that blood levels of DHT can still take multiple weeks to rebound to baseline levels prior to starting the drug.[3]https://academic.oup.com/jcem/article/89/5/2179/2844345
Richard V. Clark, David J. Hermann, Glenn R. Cunningham, Timothy H. Wilson, Betsy B. Morrill, Stuart Hobbs, Marked Suppression of Dihydrotestosterone in Men with Benign Prostatic Hyperplasia by Dutasteride, a Dual 5α-Reductase Inhibitor, The Journal of Clinical Endocrinology & Metabolism, Volume 89, Issue 5, 1 May 2004, Pages 2179–2184
The same pharmacokinetic relationships also apply to topical finasteride – provided that enough finasteride has saturated the scalp skin to match the levels of exposure in these oral finasteride withdrawal studies.
For a deeper dive into the pharmacokinetics supporting alternate doses and dosing schedules for finasteride, see these articles:
- How Often Should I Take Oral Finasteride?
- How Long Does Finasteride Stay In The Bloodstream?
- How Long Does Finasteride Remain In Scalp Tissues?
What About Scalp Contact Time?
In most cases, the longer a topical sits on the scalp skin, the better chance it has of absorbing into the skin, where it can positively impact hair follicles.
When it comes to topical finasteride, in vitro studies have measured skin absorption rates of the drug over a 24-hour period, and versus different topical formulations – such as finasteride paired with carrier ingredients such as ethosomes, alcohol, liposomes, or water.
The relationships change depending on the finasteride formulation. Just see this chart from the following study:[4]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2977015/
Penetration profiles of finasteride permeating through human skin from different preparations (mean ± SD, n = 4)
This chart suggests that absorption of topical finasteride is linear across time. In other words, the longer you leave in topical finasteride, the more of it will absorb into your scalp skin – with no diminishing returns over a 24-hour period.
Moreover, these results reveal that across the same time period, those using liposomal finasteride will absorb up to 30% less finasteride into the skin versus those using alcohol-based finasteride – and across the same time period.
This might explain why there are anecdotal reports of fewer side effects while on liposomal finasteride: less of it is getting into the scalp skin, and thereby less of it is leaching into the bloodstream and causing systemic effects. It causes fewer side effects, because it is perhaps less effective.
Additionally, liposomal finasteride users may need to let their topical sit for twice as long on the scalp to reach the same level of absorption as those using alcohol-based finasteride.
To illustrate this, look at the level of absorption for liposomal finasteride at 22 hours. It’s nearly the same as the level of absorption for hydroethanolic finasteride at 10 hours.
Finally, we also have (at least) three other variables at play that will affect finasteride absorption rates, and thereby the frequency at which we should apply topical finasteride on a daily or weekly basis:
- The total dilution of finasteride (i.e., 0.005%, 0.025%, 0.1%, etc.)
- The mL per application (i.e., 1 mL for those with localized hair loss, or 2 mL for those with diffuse hair loss)
- The application frequency (i.e., twice-daily, once-daily, once every-other-day, etc.)
For an example of how important these factors are, just see the results of this 2014 study exploring the effects of once- versus twice-daily dosing of topical finasteride on serum DHT levels:[5]https://pubmed.ncbi.nlm.nih.gov/25074865
Caserini, M., Radicioni, M., Leuratti, C., Annoni, O., & Palmieri, R. (2014). A novel finasteride 0.25% topical solution for androgenetic alopecia: pharmacokinetics and effects on plasma androgen levels in healthy male volunteers. International journal of clinical pharmacology and therapeutics, 52(10), 842–849.
As we can see from the following chart, a doubling of the daily dose had a dramatic effect on serum DHT reductions.
Which Factors Influence How Often We Can Use Topical Finasteride?
If it isn’t already obvious, it’s impossible to answer the question, “Can I use topical finasteride less than once-daily?” without more context.
Each of the variables we’ve mentioned is critically important, because minor differences in any variable can dramatically change your total weekly finasteride exposure, and thereby the actual effectiveness of the drug.
This is particularly important for those who are trying to build a topical finasteride application schedule that prevents inadvertent exposure to family members, or for those who are opting for topical finasteride to lower their risk of side effects.
So, here’s a recap of the five critical factors influencing how much topical finasteride will actually penetrate into the scalp skin:
- Topical Dilution (i.e., % finasteride). The higher the dilution, the less frequently you need to apply topical finasteride.
- Carrier Vehicles (i.e., liposomes, alcohol, etc.). Liposomal vehicles are significantly less effective versus alcohol.
- Application Dose (i.e., how many mL you apply each time). The higher the mL applied, the more drug exposure.
- Application Frequency (i.e., how often you apply). The more frequent the application, the more drug exposure.
- Scalp Contact Time (i.e., how many hours before washing out?). This is influenced by your % dilution and carrier vehicles.
Moreover, there’s a sixth factor that hasn’t yet gotten discussed: adjuvant treatments alongside topical finasteride.
If you’re combining topical finasteride with other ingredients or therapies that augment skin penetrability – i.e., retinoic acid, topical corticosteroids, or even microneedling – then you can expect more of the drug to penetrate the skin over the same time period.
That’s because these therapies wear down the stratum corneum (i.e. the outermost layer of skin), decrease the side of the epidermis, or create channels into the dermis for better drug penetration – all of which influence topical drug absorption.
What’s The Minimum Days Per Week I Can Apply Topical Finasteride?
To reiterate: the answer depends entirely on your topical dilution, carrier vehicles, application dose, how long you leave in that topical before washing it out, and your use of adjuvant therapies alongside topical finasteride.
Moreover, if someone isn’t experiencing side effects from finasteride, or if someone isn’t trying to limit other household members’ inadvertent exposure to the drug, then it doesn’t make much sense to adopt an alternate dosing schedule. It just introduces a level of complexity to your life that is, largely, unnecessary.
Nonetheless, if you are troubleshooting side effects, trying to limit a loved one’s inadvertent exposure to the drug, or simply traveling and wondering how long you can stop using topical finasteride before your hair starts falling out, you can lower your dosing frequency without necessarily hurting your hair gains.
The exact strategy will depend on why you’re doing this. For instance:
- If you’re troubleshooting side effects, you’ll likely want to lower your total weekly drug exposure. This is because total finasteride exposure is tied to side effect risks.
- If you don’t have any side effects, but you’re just trying to limit the amount of time you’re wearing topical finasteride around a partner, pregnant person, or family member – you may not want to lower your total weekly drug exposure. Instead, you may want to increase the dilution of your finasteride by a factor of 2x or more, but decrease the amount of time you wear in-the-house by washing it out more frequently, or only applying it on certain days of the week.
- If you don’t want to take topical finasteride with you on a vacation, chances are you can stop using it for 1-2 weeks (or more) without seeing much of a negative effect. After all, oral dosing studies showed that every-other-month daily doses were just as effective as every-month daily doses in the second year of use. Just make sure you reach scalp skin saturation points for finasteride before opting for this strategy – which you can likely achieve after ~30 days worth of applications.
How Much Topical Finasteride to Apply Daily
If you are opting for daily use of topical finasteride, regardless of the delivery vehicles, here are a few rules-of-thumb to consider:
- Leave for as long as possible on the scalp (If exposure is ≤ 0.1 mg daily and/or if applying less frequently than once daily). This includes a minimum of 10-12 hours, and preferably longer, before washing finasteride out of the scalp skin.
- Stick with 6-12 hour contact windows (if using twice daily)
We hope this article helps! If you’d like personal advice troubleshooting topical finasteride formulations, our research team is happy to support you inside our membership community.
References[+]
In this article, we’ll explore the history of minoxidil, how it became a hair loss drug, and the debate over its mechanisms of action for hair growth.
Despite decades of study, researchers still do not know how minoxidil promotes hair growth. But they do have some ideas, and these ideas have remained the subject of significant debate – even 70 years after the discovery of the drug.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Is Minoxidil?
Minoxidil is a drug that was originally developed in the 1950’s by Upjohn Company, which later became a part of Pfizer. In early experiments, minoxidil consistently improved vasodilation in animals, which led to human trials as a potential treatment for hypertension (i.e., high blood pressure).
In 1979, the FDA approved the use of oral minoxidil as a treatment for hypertension. But during its clinical trials and post-marketing studies, “nearly all” oral minoxidil users reported excessive hair growth as a side effect – and even the development of new hair along the face, chest, back, and scalp.[1]https://pubmed.ncbi.nlm.nih.gov/7030707/
This led to the reformulation of minoxidil as a topical, followed by clinical studies to evaluate topical minoxidil’s effectiveness in men and women facing androgenic alopecia (AGA) – one of the world’s most common hair loss disorders.
Throughout the 1980’s, a series of clinical studies consistently demonstrated that topical minoxidil was able to improve hair counts, increase hair thickness, and reduce hair shedding in male and female hair loss sufferers. And in 1988 and 1992, topical minoxidil at 5% and 2% formulations were approved by the FDA for male and female pattern hair loss, respectively.[2]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6691938/
How Does Minoxidil Work?
Despite decades of study, it’s still unclear exactly how minoxidil improves hair growth.
In animal studies, topical minoxidil has been shown to shorten the telogen (rest) phase of the hair cycle and stimulate the initiation of the anagen (active) stage of the hair cycle.[3]https://pubmed.ncbi.nlm.nih.gov/14996087/ These effects also consistently translate to humans using minoxidil (oral and topical) to treat AGA. But despite knowing what minoxidil does to most hair follicles, researchers still aren’t exactly sure of the mechanisms governing the hair growth improvements.
With that said, investigation groups do have some ideas what might be going on. In particular, there are (at least) three suspected ways minoxidil might regrow hair: its activity as a vasodilator, as well as its anti-inflammatory and anti-androgenic effects.
We’ll explore arguments for and against each hypothesis – all to elucidate why there’s still debate.
Hypothesis #1: Vasodilation (i.e, Increased Blood Flow)
The hypothesis: minoxidil improves blood, oxygen, and nutrient transport to balding hair follicles – which stimulates more robust hair growth.
Argument For
Minoxidil opens potassium ion channels, which improves circulation in microvascular networks. These potassium channels are located in a variety of places – including the muscles of peripheral arteries and within and nearby the hair follicles themselves.[4]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6691938/[5]https://faseb.onlinelibrary.wiley.com/doi/epdf/10.1096/fj.07-099424
The human scalp has a broad network of blood vessels, and is considered one of the most densely vascularized regions of the body. However, as AGA progresses, balding scalp regions undergo a loss of blood supply. For instance, clinical studies have shown 40% declines in transcutaneous oxygen levels in frontal balding regions versus non-balding controls.[6]https://pubmed.ncbi.nlm.nih.gov/8628793/ Similarly, another study found that subcutaneous blood flow is 2.6x lower in balding versus non-balding scalps.[7]https://www.jidonline.org/article/0022-202X(89)90189-9/pdf
Whether reduced blood supply is a cause or effect of the balding process is still debated – with research groups arguing both sides. However, current consensus is that if blood flow is causally linked to pattern hair loss, it is probably a secondary contributor to the balding process – rather than its root cause.
So, if minoxidil increases blood vessel diameters by opening potassium ion channels, more blood, oxygen, and nutrients might reach hair follicles and thereby lead to more robust hair growth.[8]https://pubmed.ncbi.nlm.nih.gov/22409453/
Studies using Doppler devices (a measurement tool for blood flow) showed that minoxidil appears to do this. Specifically, minoxidil improve microvascular vasodilation in skin tissues supporting hair follicles, and that these improvements coincide with hair growth.[9]https://pubmed.ncbi.nlm.nih.gov/10233226/
Other studies have found that minoxidil application grows new blood vessel openings surrounding the hair follicles themselves – a term known as fenestration.[10]https://pubmed.ncbi.nlm.nih.gov/10233226/ Fenestration is a process supporting angiogenesis, or the growth and formation of new blood vessel networks.
Therefore, mechanistic, animal, and clinical data all suggest that minoxidil might work by improving blood flow to balding regions – and that this might be the main mechanism by which minoxidil regrows hair.
Argument Against
There are three main counterarguments to the idea that minoxidil might regrow hair by improving blood flow to balding regions:
1. Reduced blood flow is likely a consequence of androgenic alopecia, rather than a cause.
While minoxidil might increase blood flow, reductions to blood flow are not considered to be the fundamental driver of AGA. Instead, the evidence most strongly supports that the overwhelming majority of reductions to blood flow that occurs during the progression of AGA is a consequence of hair cycle-mediated hair follicle miniaturization, rather than a cause of hair loss.Because of the conflation of cause-and-effect, improving circulation to thinning regions cannot be the main way in which minoxidil regrows hair – much like an increase in ice cream sales is not the cause of more shark attacks, despite both being correlated. Instead, there must be some other unidentified variable at play (in the case of ice cream sales and shark attacks, it’s “nice weather”).Therefore, minoxidil must be working to regrow hair through some other mechanism outside of increased blood flow.
2. If minoxidil works primarily by increasing blood supply, why don’t other vasodilating medications also regrow hair?
If increasing blood circulation were truly a plausible treatment target for androgenic alopecia, why don’t other antihypertensive medications regrow hair? Why is it only minoxidil?This is further evidence that minoxidil probably doesn’t work primarily through increasing blood supply to miniaturized hairs. There must be some other mechanism at play.
3. Minoxidil has other suspected mechanisms beyond circulation enhancements.
These mechanisms include, but are not limited to, prostaglandin modulation and anti-androgenic effects – the latter of which is far closer to the suspected root cause of androgenic alopecia: dihydrotestosterone (DHT), a hormone that is causally associated with the balding process.
Altogether, these three arguments form the basis by which some people reject the idea that minoxidil works primarily through increasing blood supply. But – as is the case with many topics in hair loss research – the science isn’t completely settled, because there also counterpoints to each of the above counterarguments.
Rebuttals
While the case against minoxidil working through vasodilation might appear strong, there are also compelling rebuttals to each of the counterpoints raised.
1. “Reduced blood flow is likely a consequence of androgenic alopecia, rather than a cause.”
This can be true, and simultaneously, it can also be true that targeting secondary contributors to AGA – like reductions to blood supply – can still promote hair growth.This has even been demonstrated in the context of human hair loss, whereby targeting to reduce factors such as inflammation in the infundibulum (which is believed to be partly caused by microorganisms) and/or inflammation near the dermal papillae (which is believed to be driven by the hormone DHT) in AGA patients can still improve hair growth outcomes – even without necessarily resolving the root cause(s) of that inflammation.Moreover, despite minoxidil being an FDA-approved to treat AGA, its effects on hair growth are relatively mild – particularly in the long-run – whereby hair density improvements from minoxidil start trending downward after the first year of use. The steepness of minoxidil’s downward slope is not matched by other treatments like finasteride, which directly lower scalp DHT levels and, in doing so, lead to longer-term hair gains – probably because of the drug’s ability to address factors closer to the “root cause” of AGA.
Therefore, minoxidil’s mild and long-run diminishing effects on hair growth actually support the idea that the drug targets an accelerator or secondary contributor to the balding process – rather than something closer to its root cause. There is enough alignment in mechanistic, animal, and clinical data on minoxidil to suggest that this might be increased blood supply via fenestration of vascular networks nearby hair follicles.
2. “If minoxidil works primarily by increasing blood supply, why don’t other vasodilating medications also regrow hair?”
Other anti-hypertensive medications do improve hair growth in humans. So at the outset, this counterargument makes no sense.Studies have shown that medications like diazoxide and pinacidil also increase blood flow by opening the same potassium ion channels as minoxidil, and also promote hair growth in humans.[11]https://faseb.onlinelibrary.wiley.com/doi/epdf/10.1096/fj.07-099424[12]https://www.karger.com/Article/Pdf/248368[13]https://journals.lww.com/cardiovascularpharm/abstract/1988/12002/clinical_pharmacology_of_pinacidil,_a_prototype.8.aspx[14]https://www.sciencedirect.com/science/article/pii/S0022202X9290089M
This is important, because it suggests that the mechanism of vasodilation – i.e., opening potassium ion channels – likely matters for hair growth. Because in mechanistic and animal studies, vasodilation stimulated by opening potassium ion channels seems to also enhance the vasculature surrounding the hair follicles and the fenestration of microvascular networks, whereas other vasodilating medications working through other mechanisms might not achieve the same effect.
This is because other anti-hypertensive medications do not all target potassium ion channels. Therefore, other anti-hypertensive medications will not always have the same magnitude of effect on vasodilation as minoxidil, nor will they always influence vasodilation in areas relevant to hair growth – like the microvascular regions of the scalp skin.
For an example, just see our article on peppermint oil for hair growth – in which we reviewed research showing that menthol (which is widely labeled as a “vasodilator”) happens to cause vasodilation in the vascular endothelium but vasoconstriction in vascular smooth muscle tissues.
This degree of specificity matters, but the nuance tends to get left behind by people blindly assuming that all vasodilation medications must improve hair growth in order for vasodilation to be a worthy mechanism of action by which minoxidil might work.
That’s not a reasonable assumption. Depending on the medication, dosing schedule, delivery method, and regions of application – anti-hypertensive compounds can have a range of blood flow-related effects across organ sites, arteries, veins, and microvascular networks – some of which are paradoxical.
3. “Minoxidil has other suspected mechanisms beyond circulation enhancements.”
This is true. It is also true that these mechanisms might also contribute to minoxidil’s hair growth-promoting effects. However, these mechanisms of action remain speculative, and they are supported by low-quality studies (and conflicting research) regarding their plausibility.Therefore, the existence of this speculation does not disprove the possibility that minoxidil might still work through vascular fenestration of AGA-affected hair follicles. All mechanisms can simultaneously contribute to hair growth; there need not be a “one versus the other” mentality.
Hypothesis #2: Prostaglandin Modulation
The hypothesis: minoxidil modifies prostaglandin activity, and in doing so, reduces inflammation in balding regions.
Argument For
Prostaglandins are fatty acid derivatives that come from our ingestion of omega 6 fatty acids. These lipid derivatives can have hormone-like effects on the body, and are often involved in inflammatory processes. Specifically, prostaglandins tend to increase in response to tissue damage or infection – with different prostaglandins playing roles in both inflammation generation and inflammation resolution.
In 2012, a renowned research team from the University of Pennsylvania demonstrated that prostaglandin D2 (PGD2) and prostaglandin J2 (PGJ2) were elevated in balding regions, and that in mouse models, prostaglandin D2 inhibited hair lengthening.[15]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3319975/[16]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3982925/
Moreover, research from more than a decade prior had demonstrated that minoxidil appears to enhance the activity of prostaglandins associated with the growth phase of the hair cycle, and perhaps dampen prostaglandins associated with hair loss.[17]https://pubmed.ncbi.nlm.nih.gov/9008235/
For these reasons, some researchers now believe that prostaglandin modifications are perhaps one of the ways in which minoxidil might regrow hair. In modifying prostaglandin activity, minoxidil might lower inflammation within certain hair follicle sites and, in doing so, improve hair growth outcomes.
Argument Against
When Garza et al.’s 2012 study on prostaglandin D2 was published, hair loss forums were enthralled with the possibility of developing and/or repurposing a new class of treatments for AGA: prostaglandin analogues. Excitingly, a drug developed to inhibit prostaglandin D2-mediated inflammation – setipiprant – was already undergoing clinical trials to treat asthma. As such, the drug developers repurposed the drug and began a clinical trial to see if it would also help fighting hair loss from AGA.
In 2021, the clinical trial evaluating setipiprant as a hair loss treatment was quietly published, and without a major press release. The results: the drug was well tolerated, but it did not work. Specifically, it produced no statistically significant effects on hair parameters versus the placebo group, whereas the study’s positive treatment-control group (who were taking oral finasteride) saw improvements to hair counts throughout the duration of the study.[18]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8526366/
Over the last two decades, other drugs with prostaglandin-modulating activities have also been tested to treat AGA – such as latanoprost and bimatoprost. While some clinical studies show a mild effect, these studies are poorly designed: they tend to have small sample sizes and poor methods (or no methods) of randomization for participants; they tend to include participants with other hair loss disorders in addition to AGA; and they tend to show relatively low response rates across participants, despite some endpoints achieving statistical significance.[19]https://my.perfecthairhealth.com/courses/latanoprost/ This makes it difficult to ascertain any true effects on prostaglandin modulation for AGA – if any.
Finally, follow-up studies conducted by Garza et al. (and other research groups) have actually found conflicting results regarding the presence of prostaglandins throughout the progression of AGA – with some studies showing elevated pro-inflammatory and anti-inflammatory prostaglandin levels only during specific stages of the hair cycle or specific stages of AGA’s progression.[20]https://pubmed.ncbi.nlm.nih.gov/33854354/
Altogether, these findings have significantly dampened excitement surrounding prostaglandin activity as an effective treatment target for AGA.
Rebuttals
Much like it is irresponsible to group together all anti-hypertensive medications as having the same effects on hair growth, we must also not make the same mistake by lumping together all prostaglandin analogues – setipiprant, latanoprost, bimatoprost, minoxidil, and more.
In other words, just because setipiprant failed its phase II clinical trials on AGA, and just because latanoprost appears to be inferior to minoxidil in terms of hair growth, this does not automatically mean that we can dismiss the possibility of prostaglandin modification as a potential treatment target for AGA, nor can we fully dismiss the idea that minoxidil does not work through prostaglandin modification.
Hypothesis #3: Androgen Receptor Antagonization
The hypothesis: minoxidil may reduce androgen activity in the scalp skin, and in doing so, regrow hair.
Argument For
An in vitro study published in 2014 suggested that minoxidil might make androgen receptor pathways less stable – thereby acting as a mild androgen receptor antagonist and/or anti-androgen (at least in cell culture studies).[21]https://pubmed.ncbi.nlm.nih.gov/24742982/
Overwhelming evidence implicates the hormone DHT as causally associated with the balding process. Drugs like finasteride lower DHT levels in the scalp, and in doing so, consistently improve AGA outcomes across dozens of studies spanning tens of thousands of participants.
If the results of this in vitro study hold true in vivo, this would suggest that minoxidil might help lower hormones in the scalp that are causally associated with the balding process. In doing so, minoxidil might actually target hormonal causes of hair loss – even though the drug isn’t believed to change hormonal profiles in the (serum) blood or elicit significant anti-androgenic effects elsewhere throughout the body.[22]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6691938/
Argument Against
This 2014 in vitro study conflicts with other studies exploring whether minoxidil has anti-androgenic effects.
For instance, a 1987 study and a 2017 study both found that minoxidil doesn’t appear to affect androgens – with the latter study suggesting that minoxidil may even enhance androgenic activity in the scalp.[23]https://pubmed.ncbi.nlm.nih.gov/3800423/[24]https://pubmed.ncbi.nlm.nih.gov/30064598/
Therefore, it can just as easily be argued that minoxidil enhances androgenic activity in the scalp skin, rather than inhibits it.
Rebuttals
To our knowledge, there aren’t any strong rebuttals to these counterpoints. With such little evidence existing on this subject – and with the existing studies finding conflicting results – the jury is still out on whether minoxidil has any anti-androgenic effects at all.
Final Thoughts
The way in which minoxidil grows hair is still up for debate.
To date, there are (at least) three leading hypotheses, all of which have their problems:
- Increased microcirculation to balding regions through vascular fenestration
- Prostaglandin modulation – specifically related to PGE2
- Anti-androgenic activity
What’s important to note is that there is not enough evidence to dismiss any of these suspected mechanisms. As such, all of them are still in the running, and all of them might contribute toward minoxidil hair growth-promoting effects.
With more research, we’ll hopefully have a final answer. And if we ever do, we’ll update this article with more information.
References[+]
References ↑1 https://pubmed.ncbi.nlm.nih.gov/7030707/ ↑2, ↑4, ↑22 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6691938/ ↑3 https://pubmed.ncbi.nlm.nih.gov/14996087/ ↑5, ↑11 https://faseb.onlinelibrary.wiley.com/doi/epdf/10.1096/fj.07-099424 ↑6 https://pubmed.ncbi.nlm.nih.gov/8628793/ ↑7 https://www.jidonline.org/article/0022-202X(89)90189-9/pdf ↑8 https://pubmed.ncbi.nlm.nih.gov/22409453/ ↑9, ↑10 https://pubmed.ncbi.nlm.nih.gov/10233226/ ↑12 https://www.karger.com/Article/Pdf/248368 ↑13 https://journals.lww.com/cardiovascularpharm/abstract/1988/12002/clinical_pharmacology_of_pinacidil,_a_prototype.8.aspx ↑14 https://www.sciencedirect.com/science/article/pii/S0022202X9290089M ↑15 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3319975/ ↑16 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3982925/ ↑17 https://pubmed.ncbi.nlm.nih.gov/9008235/ ↑18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8526366/ ↑19 https://my.perfecthairhealth.com/courses/latanoprost/ ↑20 https://pubmed.ncbi.nlm.nih.gov/33854354/ ↑21 https://pubmed.ncbi.nlm.nih.gov/24742982/ ↑23 https://pubmed.ncbi.nlm.nih.gov/3800423/ ↑24 https://pubmed.ncbi.nlm.nih.gov/30064598/ Oral finasteride is a drug that helps lower levels of dihydrotestosterone (DHT) – the hormone causally associated with androgenic alopecia (AGA). Since 1997, the FDA has approved oral finasteride at 1 mg daily doses to treat AGA.[1]https://www.ncbi.nlm.nih.gov/books/NBK513329/
Having said that, clinical studies also suggest that daily doses of finasteride as low as 0.2 mg can reduce nearly as much DHT as 1.0 mg daily, and lead to similar hair count improvements.[2]europepmc.org/article/med/15319158
For these reasons, many finasteride users have wondered why physicians routinely prescribe 1 mg pills when they can potentially reap the same hair gains with 0.2 mg, or 1/5th the total drug exposure.
In this article, we’ll explore the science behind finasteride’s dosing, and if alternate dosing schedules make sense.
Interested in Oral Finasteride?
Oral finasteride & minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What’s the Ideal Oral Finasteride Dosage For Hair Growth?
In pharmaceutical settings, ideal doses are determined based on the perfect intersection whereby a drug maximizes benefit while minimizing side effects. For finasteride, that would be the dose that maximizes DHT reduction (and thereby hair regrowth) while minimizing the risk of adverse events.
To determine what this dose is, investigators must conduct a range of dosing studies on finasteride for the treatment of AGA – and then measure hair parameter outcomes against any perceived side effects.
Luckily for us, these studies have already been conducted.
Finasteride’s dose-dependent effects on serum DHT
Finasteride is a drug that lowers levels of the hormone DHT – which is causally linked to the balding process in men and women with androgenic alopecia.
A 1999 study sought to determine the effects of finasteride on DHT levels in the blood and scalp, depending on the dose someone took: 0.01 mg, 0.2 mg, 0.05 mg, 1.0 mg, or 5.0 mg.[3]https://pubmed.ncbi.nlm.nih.gov/10495374/
The investigators found that finasteride had what’s known as a logarithmic, dose-dependent effect on DHT reduction. That’s just a fancy way of saying that a little finasteride had nearly the same effect on DHT as a lot of finasteride – and that with higher doses, the marginal reduction of DHT got smaller and smaller.
Serum DHT Reductions vs. Finasteride Dosages
For instance, the above chart shows that while 0.01 mg daily of finasteride barely reduces any DHT, 0.2 mg daily reduces almost as much as DHT as 5 mg daily – even though 5 mg of finasteride 25x higher than the 0.2 mg dose.
Thus, the investigators concluded:
“In this study, doses of finasteride as low as 0.2 mg per day maximally decreased both scalp skin and serum DHT levels. These data support the rationale used to conduct clinical trials in men with male pattern hair loss at doses of finasteride between 0.2 and 5 mg.”
Interestingly, finasteride’s phase III clinical trials (which granted the drug FDA approval) tested a dose of 1 mg daily – and with impressive results on hair count parameters and a relatively low rate of reported side effects versus placebo.[4]https://pubmed.ncbi.nlm.nih.gov/9777765/
But what about lower daily doses of finasteride? Might those also work to regrow hair – all while reducing drug exposure and perhaps side effects?
According to small clinical studies, yes – albeit with caveats.
Finasteride: dose-dependent effects on hair counts & side events
While the evidence is limited, there have been a handful of small clinical trials comparing different daily doses of finasteride on hair counts (and side effects) in men with androgenic alopecia.
One study tested daily doses of finasteride at 0.01 mg, 0.2 mg, 1.0 mg, and 5.0 mg versus placebo for 1-2 years. The researchers found that doses at or above 0.2 mg daily were effective at regrowing hair versus placebo, but that doses of 1.0 mg to 5.0 mg were directionally superior versus 0.2 mg doses.[5]https://pubmed.ncbi.nlm.nih.gov/10495375/
Just see this chart for a breakdown of the numbers:
Roberts JL, Fiedler V, Imperato-McGinley J, Whiting D, Olsen E, Shupack J, Stough D, DeVillez R, Rietschel R, Savin R, Bergfeld W, Swinehart J, Funicella T, Hordinsky M, Lowe N, Katz I, Lucky A, Drake L, Price VH, Weiss D, Whitmore E, Millikan L, Muller S, Gencheff C, et al. Clinical dose ranging studies with finasteride, a type 2 5alpha-reductase inhibitor, in men with male pattern hair loss. J Am Acad Dermatol. 1999 Oct;41(4):555-63. PMID: 10495375.
Moreover, here’s a chart visualizing the differences in hair counts across the full two years:
Roberts JL, Fiedler V, Imperato-McGinley J, Whiting D, Olsen E, Shupack J, Stough D, DeVillez R, Rietschel R, Savin R, Bergfeld W, Swinehart J, Funicella T, Hordinsky M, Lowe N, Katz I, Lucky A, Drake L, Price VH, Weiss D, Whitmore E, Millikan L, Muller S, Gencheff C, et al. Clinical dose ranging studies with finasteride, a type 2 5alpha-reductase inhibitor, in men with male pattern hair loss. J Am Acad Dermatol. 1999 Oct;41(4):555-63. PMID: 10495375.
So, what about adverse events? That same study concluded:
“The incidence of these side effects with finasteride therapy was generally comparable to that observed with treatment with placebo, and there was no evidence of dose dependency or increased incidence with longer therapy out to 12 months. In addition, these side effects ceased in some patients while they continued to receive finasteride.”
In other words, the authors of the study found that while 1mg daily doses of finasteride produced directionally better – but not statistically significantly better – hair count improvements, these improvements did not come at the expense of a higher rate of side effects.
Thus, the investigators concluded that 1mg daily of finasteride was probably the best dose for treating androgenic alopecia.
Having said that, other studies haven’t shared the exact same conclusions.
For instance, a 2004 study on 414 Japanese men found that 1.0 mg daily doses of finasteride produced “numerically superior” results versus 0.2 mg daily, but that 1.0 mg daily doses also came with a numerically superior risk of side effects.[6]https://www.researchgate.net/publication/8392775_Finasteride_in_the_treatment_of_Japanese_men_with_male_pattern_hair_loss
Similar to the other finasteride dosing study, none of the differences in hair count changes or side effect incidences were statistically significant. Nonetheless, the investigators felt the differences in results were still strong enough to note in the conclusions of their study.
Summary (so far)
Based on the totality of data currently available, this leads us to believe the following:
- DHT reduction. Finasteride daily doses of 0.2 mg, 1.0 mg, and 5.0 mg all reduce nearly the same amount of DHT in the body.
- Hair counts. Compared to 0.2 mg doses, 1.0 mg and 5.0 mg doses of finasteride result in directionally better hair counts over 1-2 years.
- Side effects. Compared to 0.2 mg doses, 1.0 mg and 5.0 mg may also come with a directionally higher risk (or magnitude) of side effects.
So, if we choose to lean into these directional (but not statistically significant) results and believe that lower doses of finasteride come with a lower risk of side effects, the next question becomes: “How infrequently can I use finasteride and still see hair gains?”
Can I Use Finasteride Less Than Once Daily?
The answer depends on a number of factors, including finasteride’s:
- Terminal half-life (i.e., how long it takes for 50% of the drug to become inactivated)
- Tissue dissociation timing (i.e., how long it takes for finasteride to leave skin tissues)
- Biological half-life (i.e., how long it takes for finasteride’s effect on DHT to get cut in half)
We’ve covered these topics in great detail inside the following articles. For more information, please read:
For now, here are the key takeaways from the literature:
- Finasteride has a terminal half-life of 5-7 hours.
- After multiple daily doses, finasteride reaches a tissue dissociation timing of 4-5 days.
- Due to both of the above, finasteride’s effects on DHT suppression can remain for up to 14-30 days after quitting the drug.
On that note, one dosing study on finasteride found that after a year of daily use, every-other-month dosing of 1 mg daily of finasteride was just as effect as once-daily dosing – despite users in the first group using the drug for a total of 6 versus 12 months throughout the same year.[7]https://jaad.org/retrieve/pii/S0190962220319289
Again, this is because finasteride’s effects don’t immediately dissipate upon cessation of the drug. They can last up to 14-30 days from the last dose – at least after reaching a certain saturation point in the body (which often requires a handful of days of use at 1 mg daily).
With all of this in mind, finasteride users who are interested in (1) achieving some hair gains, and (2) minimizing their drug exposure – all in hopes of lowering their risk of side effects – may be able to achieve this by reducing their dosing schedule of finasteride.
Alternate Dosing Schedules For Finasteride
To best conceptualize this, it’s easier to think of finasteride dosing in terms of weekly exposure levels, rather than daily. This is because finasteride’s effects on DHT can accumulate across doses, and because lower doses tend to have a similar impact on DHT as higher doses (up to a point).
For instance, those studies showing statistically equivalent efficacy of 0.2 mg versus 1.0 mg daily of finasteride represented dosing difference of 1.4 mg versus 7.0 mg weekly of finasteride.
So, how can we take into account finasteride’s biological half-life to build an alternate dosing schedule that might help support hair growth, albeit with a lower overall drug exposure?
We can likely do so by trying a finasteride dosing schedule of 0.5 mg, 3x weekly.
For most people, that would involve taking 0.5 mg of finasteride every Monday, Wednesday, and Friday. That’s ~1.5 mg weekly of exposure, which is roughly the same as 0.2 mg daily (or 1.4 mg weekly).
In that regard, you can achieve this by simply getting a standard prescription of finasteride for 1.0 mg daily. Companies like Hims, Keeps, and Roman (no affiliation!) often offer these bundled in 90-day supply.
Then, you can cancel that subscription product, buy a pill cutter, and just cut the pills in half.
You can take one-half pill every Monday, Wednesday, and Friday – which equates to 1.5 pills weekly.
If you received a 90-day supply of 1.0 mg daily of finasteride from any of these companies, this alternate dosing schedule should last you a total of 60 weeks – which is more than a year.
With this alternate dosing schedule, you also reduce your total costs of finasteride treatment to just a few dollars per month. So for those who are financially constrained, it’s potentially a wonderful option.
Whether or not these lower doses actually worsen hair count outcomes or lower side effect risks is still up for debate. Nonetheless, this reduced dosing schedule should – at a minimum – lower your overall drug exposure. For this reason, this alternate dosing schedule is also included as part of our guide on troubleshooting finasteride-related side effects.
We hope this article helps. If you’re looking for personal support on hair growth journey, you can receive personalized support and work with our team of researchers directly inside our membership community.
References[+]
References ↑1 https://www.ncbi.nlm.nih.gov/books/NBK513329/ ↑2 europepmc.org/article/med/15319158 ↑3 https://pubmed.ncbi.nlm.nih.gov/10495374/ ↑4 https://pubmed.ncbi.nlm.nih.gov/9777765/ ↑5 https://pubmed.ncbi.nlm.nih.gov/10495375/ ↑6 https://www.researchgate.net/publication/8392775_Finasteride_in_the_treatment_of_Japanese_men_with_male_pattern_hair_loss ↑7 https://jaad.org/retrieve/pii/S0190962220319289 After quitting finasteride, many users wonder how long they have until:
- The drug leaves the bloodstream
- Hormone levels to return to baseline
- When hair loss will resume
The answers vary slightly from person-to-person, but all relate to how finasteride behaves in the body: its distribution, saturation, tissue binding capacity, metabolism, and excretion. These terms are all related to the pharmacokinetics.
In this article, we’ll dive into the pharmacokinetics of finasteride to answer how long finasteride stays active in the scalp skin. In doing so, we’ll also reveal an alternate dosing strategy that some finasteride users employ to maintain hair gains, but potentially lower their risk or magnitude of side effects.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Is Finasteride?
Finasteride is an FDA-approved drug for androgenic alopecia (AGA) – one of the world’s most common hair loss disorders in adults.
Finasteride works by blocking the formation of an enzyme called 5α-reductase, which transforms free testosterone into dihydrotestosterone (DHT). An abundance of evidence shows that DHT is causally associated with hair growth cycle disruptions, hair thinning, and hair loss from AGA. Clinical studies also show that finasteride can therapeutically lower DHT and, in doing so, improve AGA outcomes in 80-90% of the men who use it.[1]https://pubmed.ncbi.nlm.nih.gov/9777765/
For these reasons, many consider finasteride to be the gold-standard treatment for AGA.
Unfortunately, as with all drugs, finasteride is also causally linked to side effects in a portion of men and women trying the drug. It’s also contraindicated in women who are planning to become pregnant, already pregnant, and/or breastfeeding – with debate over whether men should stop finasteride prior to conceiving.
For these reasons, some finasteride users choose to stop using the drug for a variety of reasons: (1) troubleshoot side effects, (2) conceive without finasteride detectable in the semen, or (3) just take a break due to travel.
What Happens When Someone Quits Finasteride?
Clinical studies on finasteride also show that once the drug is paused, hair loss eventually presumes and converges back to where a user would’ve been had they never started the drug in the first place.
Just see this chart from a two-year clinical study on men using 1 mg daily of finasteride.[2]https://pubmed.ncbi.nlm.nih.gov/9777765/ In the group labeled Fin → Pbo, users were given finasteride for the first year, and then unknowingly switched into the placebo group from year one to year two. As we can see, hair counts improve up until year one, then decline below baseline by the end of year two:
Kaufman KD, Olsen EA, Whiting D, Savin R, DeVillez R, Bergfeld W, Price VH, Van Neste D, Roberts JL, Hordinsky M, Shapiro J, Binkowitz B, Gormley GJ. Finasteride in the treatment of men with androgenetic alopecia. Finasteride Male Pattern Hair Loss Study Group. J Am Acad Dermatol. 1998 Oct;39(4 Pt 1):578-89. doi: 10.1016/s0190-9622(98)70007-6. PMID: 9777765.
For these reasons, the manufacturers of finasteride often warn users that after quitting the drug, hair loss will resume, and within 3-12 months, any hair gains maintained by the drug will be lost.
But just how long after quitting finasteride will it take for hair loss to resume? The question depends entirely on finasteride’s biological half-life in scalp skin tissues. More specifically, it depends on how long finasteride can continue suppressing DHT levels in the scalp, even after a user has stopped taking it.
Finasteride: Effects On Scalp DHT
To reiterate, DHT is the hormone causally linked to hair loss from AGA. Finasteride can therapeutically lower DHT levels by ~70% throughout the body. At this level of suppression, AGA often stabilizes and some hair regrowth can be achieved.[3]https://pubmed.ncbi.nlm.nih.gov/10495374/
However, when it comes to scalp hair regrowth, DHT reduction is not as important throughout the body as it is in the scalp.
After all, several studies from the 1980’s and 1990’s suggest that up to 80% of the DHT found in balding scalps is manufactured at the site of the hair follicle – more specifically, the outer root sheath, dermal papillae cell cluster, and even the mesodermal sheath.[4]https://www.ncbi.nlm.nih.gov/books/NBK557634/[5]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459338/[6]https://dm5migu4zj3pb.cloudfront.net/manuscripts/113000/113003/JCI87113003.pdf
Therefore, when many people ask, “How long does finasteride stay in the bloodstream?”, they’re mostly asking the wrong question. Instead, they should be asking, “How long does finasteride continue to impact scalp DHT levels – even after quitting the drug?”
The answer to that question depends on finasteride’s:
- Terminal half-life. In other words, how long will it take for 50% of the finasteride ingested to get metabolized and sent to the digestive tract for excretion?
- Tissue dissociation. In other words, how long does it take for active finasteride to “unbind” to those tissues and re-enter circulation and/or get sent to the digestive tract for excretion?
- Biological half-life. In other words, given finasteride’s terminal half-life and tissue dissociation timing, how long will it take for 50% of the drug to stop having its biological impact (i.e., lowering DHT levels)?
The answers will help provide a more nuanced perspective on just how long finasteride stays active in the scalp, and how long someone has before hair loss might presume.
Finasteride Pharmacokinetics
According to pharmacokinetic studies, here’s some key information about finasteride:[7]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3481923/
- Terminal half-life: 5-7 hours, with slightly longer half-lives in older populations
- Tissue dissociation: 4-5 days, meaning that finasteride can remain attached and/or bound to organs for longer than its half-life – which potentiates the drug having a longer-lasting effect than its terminal half-life might suggest
- Biological half-life: 14-30 days, mainly due to its tissue dissociation timings after reaching peak drug distribution and saturation throughout the body (which can happen after only a handful of 1 mg daily ingestions of the drug)
How Long Does Finasteride Impact Scalp DHT Levels?
For most people, finasteride appears to still appreciably lower scalp DHT levels for up to 30 days after quitting the medication.
This was best illustrated in a clinical study measuring blood DHT levels before, during, and after use of finasteride and dutasteride versus a placebo group.[8]https://academic.oup.com/jcem/article/89/5/2179/2844345
Richard V. Clark, David J. Hermann, Glenn R. Cunningham, Timothy H. Wilson, Betsy B. Morrill, Stuart Hobbs, Marked Suppression of Dihydrotestosterone in Men with Benign Prostatic Hyperplasia by Dutasteride, a Dual 5α-Reductase Inhibitor, The Journal of Clinical Endocrinology & Metabolism, Volume 89, Issue 5, 1 May 2004, Pages 2179–2184
Again, the answer is due to how finasteride is stored in organs like the skin. Studies suggest that once finasteride binds to cells within the skin, it has a tissue dissociation timing of 4-5 days.[9]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3481923/
In other words, it can take 4-5 days before the finasteride that has bound to skin cells dissociates from those tissues and reenters the bloodstream for metabolism and excretion.
Interestingly, once finasteride users understand these pharmacokinetics, they can actually use them to their advantage in order to (1) temporarily quit finasteride (if needed), while also (2) preserving hair gains from the drug.
Taking Advantage Of Finasteride’s Tissue Dissociation Timings
Given the relatively long biological half-life of finasteride, many users have wondered, “Can I temporarily quit the drug for any reason, and without sacrificing any of my hair gains?”
So far, clinical studies seem to suggest it’s possible – at least within short-enough cessation periods.
One clinical study on men showed that after one year of taking finasteride, men who switched to a 30-day on, 30-day off dosing schedule for year two achieved comparable hair regrowth to those who continued taking finasteride daily.[10]https://jaad.org/retrieve/pii/S0190962220319289
In other words, these men were able to cut their drug exposure by 50% throughout year two – and take a total of 6 months off the drug – without sacrificing any hair gains versus those taking the drug daily throughout that same year.
This is, again, due to finasteride’s biological half-life – which relates to its terminal half-life and tissue dissociation timings.
Anecdotally, many members of our community have found that taking a 2- to 3-week break from finasteride to troubleshoot side effects, or to fully disconnect during family vacations, does not seem to adversely impact their hair gains. So, at least within our community, we have a number of people to corroborate this clinical evidence with real-world experience.
Beyond a full month of quitting, it’s very likely that scalp levels of DHT fully return to baseline and that hair loss resumes. So, keep this in mind before deciding to experiment with different finasteride dosing schedules.
References[+]
References ↑1, ↑2 https://pubmed.ncbi.nlm.nih.gov/9777765/ ↑3 https://pubmed.ncbi.nlm.nih.gov/10495374/ ↑4 https://www.ncbi.nlm.nih.gov/books/NBK557634/ ↑5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459338/ ↑6 https://dm5migu4zj3pb.cloudfront.net/manuscripts/113000/113003/JCI87113003.pdf ↑7, ↑9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3481923/ ↑8 https://academic.oup.com/jcem/article/89/5/2179/2844345 ↑10 https://jaad.org/retrieve/pii/S0190962220319289 Oral finasteride is a gold-standard treatment option for men wanting a low-effort approach to hair maintenance. The drug is FDA-approved for androgenic alopecia (AGA) – with two-year studies showing that 1 mg daily of finasteride might slow, stop, or partially reverse AGA progression in 80-90% of men using the drug.[1]https://pubmed.ncbi.nlm.nih.gov/9777765/
But what happens when someone decides to stop using finasteride? How long does the drug remain in the system? After withdrawal, how long does the drug continue to impact hormones like dihydrotestosterone (DHT)?
In this article, we’ll explore the scientific papers that have attempted to answer these questions, and provide step-by-step instructions for what to expect should you decide – for any reason – to withdraw from finasteride.
Interested in Oral Finasteride?
Oral finasteride & minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Why Might Someone Stop Using Finasteride?
There are three main reasons someone might withdraw from finasteride use:
- Experiencing side effects. In this case, withdrawing can help troubleshoot if those side effects are related to the drug or perhaps something else in their life.
- Trying to conceive. Under these circumstances, a user may not want to risk having the drug interfere with their ability to do so or the health of the baby. (Note: while men have the option to temporarily withdraw from finasteride during windows of conception, the drug is contraindicated in women who are pregnant, planning to become pregnant, or breastfeeding.)
- Not seeing enough benefit. Unfortunately, finasteride doesn’t work for everyone, which may lead to drug withdrawal for those not seeing desired results.
In cases of side effects and conception, withdrawal might be temporary.
For instance, men experiencing sexual dysfunction might withdraw from finasteride to gauge if it’s the drug causing the side effect, or perhaps something else in their life (like poor dietary, lifestyle, and/or environmental habits). Men who want to conceive might temporarily withdraw from finasteride to ensure that none of their semen is influenced by finasteride during the period of conception, after which they can then hop back on the drug.
However, for those who are having trouble tolerating finasteride – or for those who aren’t getting any results from the drug – finasteride withdrawal might be more permanent. In these cases, users might find better success by switching to dutasteride, adding in adjuvant therapies like microneedling and/or minoxidil, or exploring if their hair loss is actually androgenic or perhaps caused by other factors – like hypothyroidism.
Under these circumstance, how long does finasteride stay in the bloodstream after we stop taking it? How long until the effects of the drug reverse?
After Quitting, How Long Does Finasteride Stay in the Bloodstream?
The answer depends on (1) how long it takes for the body to metabolize finasteride, and (2) whether you’ve taken enough finasteride to reach steady-state saturation levels throughout the body.
The term most often used to describe drug metabolism is terminal half life. That’s the amount of time it takes for the body to metabolize 50% of a drug dose.
According to pharmacokinetic studies, finasteride has a terminal half-life in the bloodstream of 5-7 hours. This means that it takes 5-7 hours before half of the drug is metabolized from the circulatory system and sent for excretion – where finasteride is primarily excreted through bile and urine.[2]https://pubmed.ncbi.nlm.nih.gov/8846625/
So, if you took 1 mg of finasteride one time, your body would probably metabolize, inactivate, and excrete all of that finasteride within a 2-3 days.
However, taking 1 mg one time isn’t how most people use finasteride. So, what about real-world usage cases – where someone takes 1 mg of finasteride daily for weeks, months, or years?
If this person stops, how long would it take for the drug to clear the system and for the drug’s effects to go away?
With repeated doses, finasteride reaches a saturation point throughout the body. This is where the drug travels throughout the bloodstream, gets distributed throughout other organs and tissues, and after that distribution reaches its peak, blood levels of finasteride reach a steady-state.
In other words, there’s an equilibrium reached for the amount of new finasteride coming into the body, and the amount of finasteride getting metabolized and excreted by the body. And we can measure this equilibrium by measuring steady-state plasma levels (i.e., blood levels) of finasteride as someone takes repeat doses.
For most people, steady-state plasma levels of finasteride are reached within just a few days.[3]https://pubmed.ncbi.nlm.nih.gov/24012200/ And once that occurs, the “equation” for finasteride’s full elimination changes.
Why? Because now finasteride’s excretion isn’t just dependent on its terminal half-life – or how long it takes for 50% of that finasteride to get metabolized from the blood. Now, the equation must also take into account how long it will take for all finasteride that has been stored in other tissues and organs – like the skin and prostate – to dissociate from those sites, re-enter the blood stream, and get metabolized.
According to pharmacokinetic studies, finasteride has a tissue dissociation timing of 4-5 days.[4]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3481923/ Because of this, finasteride’s full excretion from the body (and bloodstream) can actually take a bit longer than a few days.
In fact, withdrawal studies on finasteride have demonstrated that despite its terminal half-life of 5-7 hours, it still takes ~30 days for blood levels of dihydrotestosterone (i.e., DHT) to return back to baseline after someone quits the drug.[5]https://academic.oup.com/jcem/article/89/5/2179/2844345 Just see this chart comparing drug withdrawal from finasteride and dutasteride versus placebo – and the number of weeks it takes for the finasteride group to return to baseline levels of serum DHT.
Richard V. Clark, David J. Hermann, Glenn R. Cunningham, Timothy H. Wilson, Betsy B. Morrill, Stuart Hobbs, Marked Suppression of Dihydrotestosterone in Men with Benign Prostatic Hyperplasia by Dutasteride, a Dual 5α-Reductase Inhibitor, The Journal of Clinical Endocrinology & Metabolism, Volume 89, Issue 5, 1 May 2004, Pages 2179–2184
Moreover, after quitting, former finasteride users will typically lose any hair gains from the drug within 3-12 months.
So, to summarize:
- Finasteride’s terminal half-life is 5-7 hours. This is the amount of time it takes for 50% of a drug’s dose to be metabolized and sent for excretion.
- Finasteride’s biological half-life is 14-30 days. This is the amount of time it takes for the biological effects of a drug to fully reverse. In the case of finasteride, this is a return to baseline levels of DHT. This takes longer than a drug’s terminal half-life, because the equation for biological half-life involves not only a drug’s terminal half-life, but also the drug’s saturation levels and its tissue dissociation timings.
How To Take Advantage Of Finasteride’s Terminal & Biological Half-Lives
Because of the mismatch between finasteride’s terminal half-life and biological half-life, users of finasteride who withdraw from the drug don’t immediately lose their hair. Instead, it usually takes ~3 months for hair loss following finasteride withdrawal to presume.
In fact, one clinical study found that after one year of finasteride use, men who switched to 30 days-on, 30 days-off finasteride use were no worse off than men who continued taking the drug every day.[6]https://www.jaad.org/article/S0190-9622(20)31928-9/fulltext
This is, again, because of the difference in finasteride’s terminal and biological half-lives. And with this knowledge, finasteride users who intend to temporarily withdraw from the drug can leverage these differences to their advantage.
For example, say a male would like to conceive with their partner, but they don’t want finasteride to potential impact their semen parameters during the window of conception. This user can:
- Withdraw from finasteride. After 30 days, the drug should be fully out of the system and all biological effects should return to baseline.
- Conceive with their partner. Technically speaking, they have a 1-2 month window after that 30-day washout period whereby hair gains from finasteride should remain preserved.
- Hop back on finasteride. After conception is complete, this male can restart finasteride prior to hair loss reinitiating – so long as they were able to conceive during that 1-2 month window following their finasteride washout period.
The same approach can be taken with troubleshooting side effects, or deciding to leave finasteride at-home while traveling short-term, or any other reason you might want to temporarily hop off the drug.
Those experiencing side effects can potentially minimize them by switching to a topical formula. Just be aware that topical finasteride can enter the bloodstream, too, depending on the percent active ingredient, the amount applied, and the length of time the solution is left on the scalp.
References[+]
References ↑1 https://pubmed.ncbi.nlm.nih.gov/9777765/ ↑2 https://pubmed.ncbi.nlm.nih.gov/8846625/ ↑3 https://pubmed.ncbi.nlm.nih.gov/24012200/ ↑4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3481923/ ↑5 https://academic.oup.com/jcem/article/89/5/2179/2844345 ↑6 https://www.jaad.org/article/S0190-9622(20)31928-9/fulltext Post-Finasteride Syndrome is a term used to describe a constellation of symptoms reported by former finasteride users who quit using the drug, but who still report drug-related side effects more than 3 months after discontinuing.
Amongst dermatologists, endocrinologists, and hair loss researchers, the existence and prevalence of Post-Finasteride Syndrome (PFS) is a hotly debated topic. On the one hand, some urologists like Dr. Abdulmaged Traish are adamant that PFS is real, and that the original clinical trials that earned finasteride FDA approval were neither adequately designed nor robust enough to capture how many finasteride users might be affected.[1]https://pubmed.ncbi.nlm.nih.gov/32033719/
On the other hand, some world-renowned hair loss researchers like Dr. Ralph Trueb claim that PFS is a self-induced delusional disorder bordering on mass formation psychosis – and support those claims by pointing to (1) the absence of evidence of PFS from the original finasteride studies, (2) the influence of media reporting on PFS and subsequent spikes in people claiming to have the condition, and (3) a strong proclivity toward those claiming to have PFS also having diagnosed mental health disorders – particularly histrionic personality disorder.[2]https://www.karger.com/Article/Fulltext/497362
So, what’s the truth about PFS? Is it real or imagined? If PFS is real, what’s the estimated risk for people trying finasteride? And is there anything that can be done to lower the risk of PFS?
In this article, we’ll explore the evidence on both sides of the PFS argument, explain why the existence of PFS is difficult to study, and reveal why debate over PFS is likely here to stay. Finally, we’ll contextualize the estimated prevalence of PFS by comparing its risk ratio to other voluntary risks taken in each day of life – like the risk of death from driving a motor vehicle – all so that potential finasteride users can make more informed decisions about their hair loss treatments.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Is Post-Finasteride Syndrome (PFS)?
Post-Finasteride Syndrome (PFS) is an alleged condition from the use of finasteride, whereby side effects incurred from the drug do not go away 3+ months after quitting. The implication of PFS is that, for a very small number of finasteride users, side effects might be long-lasting, and perhaps permanent.
Alleged PFS symptoms vary from person-to-person, but in general, may involve persistent and unresolved:
- Sexual dysfunction
- Genital numbness
- Reduced libido and/or weak erections
- Persistent brain fog
- Depressive-like symptoms
Some people claiming to experience PFS-related side effects have described their onset within hours of taking a single finasteride pill. Others say it took months before anything started going wrong. Others say they were symptom-free while using finasteride, and that they only started experiencing side effects after withdrawing from the drug.
Given the heterogeneity in both PFS symptoms and their timings of onset, researchers (and sufferers) have struggled to understand why this alleged condition seems to impact so many people in such wildly different ways.
Nonetheless, those who believe PFS is real also suspect that its development is causally linked to the enzyme that finasteride inhibits, as well as the potential for that enzyme inhibition to have unintended, downstream, long-lasting effects on the body.
Finasteride & Side Effects: A History Of Debate
Finasteride is a drug that inhibits the type II 5-alpha reductase enzyme. By inhibiting this enzyme, finasteride lowers levels of dihydrotestosterone (DHT) – a hormone causally associated with androgenic alopecia (AGA) and benign prostatic hyperplasia.
At daily doses of 0.2 mg to 5.0 mg daily, oral finasteride can therapeutically lower DHT levels by 70% – with two-year studies showing that 80-90% of men using the drug see a slowing, stopping, or partial reversal in AGA.[3]https://www.sciencedirect.com/science/article/pii/S0022202X15529357 In fact, dozens of studies totaling more than 10,000 participants suggest that oral finasteride routinely improves hair growth outcomes versus placebo – with 5- and 10-year studies suggesting hair maintenance above baseline for a majority of its users.[4]https://www.oatext.com/Long-term-(10-year)-efficacy-of-finasteride-in-523-Japanese-men-with-androgenetic-alopecia.php
For these reasons (and the quality of evidence supporting the medication), finasteride has received FDA-approval for AGA and is widely considered the gold-standard medical intervention for this condition.
But as is the case with all medications, there’s always a risk of side effects. For finasteride, these side effects tend to present in the form of lowered libido, sexual dysfunction, gynecomastia, and/or brain fog.
While the original clinical trials that granted finasteride FDA-approval estimated side effect risks to be less than 5% versus placebo, follow-up studies have put that risk as high as 40%.[5]https://www.sciencedirect.com/science/article/pii/S0022202X15529357[6]http://www.drproctor.com/propecia/propecia.pdf Depending on the online resource you read (i.e., a natural website versus a telehealth website), you may have noticed that websites will cite either end of the extreme, depending on the products they’re trying to sell. Natural websites tend to cite higher numbers to fearmonger over side effects and encourage people to buy their natural supplements and topicals; telehealth websites tend to avoid discussions about higher estimations because it might interfere with prescription drug sales.
The reality is that most follow-up studies citing higher rates of finasteride-related side effects tend to be of lower quality – with smaller sample sizes, biases in research methodologies, and a strong influence of the nocebo effect – whereby in some studies, physicians actually told patients to “watch out” for side effects while prescribing the drug, which introduces a psychogenic influence whereby patients become nearly 5 times as likely to report those side effects.[7]https://www.nature.com/articles/ncpuro1012
At the same time, other researchers have pointed out that finasteride’s original clinical trials also contain their own biases. For instance, those studies were funded by Merck – the very drug company that stood to gain from the approval of its patented hair loss-fighting medication – and that this might’ve influenced the ways in which side effects were both catalogued and tabulated by investigators – all to downplay their true prevalence and/or magnitude.
While these criticisms may read as conspiratorial and unfounded, the reality is that Merck doesn’t have the best reputation as a drug company. Former employees-turned-whistleblowers alleging clinical trial obfuscation in vaccine trials, and lawsuits settled after drugs taken to market by Merck later inadvertently killed lots of people.[8]https://www.fiercepharma.com/vaccines/whistleblowers-accuse-merck-of-withholding-info-on-mumps-vaccine[9]https://www.nature.com/articles/450324b Because of this history, criticisms of this nature will remain on-the-table for Merck, regardless of their validity.
Based on our experience working with hair loss sufferers (and our read of the data), we estimate that between 5% to 15% of finasteride users experience some degree of side effects – and that the majority of these side effects are mild and improvable – at least with the right titration and/or drug delivery strategies. If you’re interested in learning more, see our article on strategies to reduce side effects from finasteride, and if blood tests can help predict finateride-linked side effects.
Nonetheless, it is true that a small subset of finasteride users do experience side effects, and that many of those side effects are sexual or cognitive in nature. What is debated, however, is whether those finasteride-induced side effects reverse entirely for 100% of people after quitting the medication.
According to finasteride’s phase II and phase III clinical trials, all participants who stopped using finasteride due to side effects saw a complete resolution of those side effects, and within three months. Yet in the last 15 years, some former finasteride users have claimed otherwise.
So what might explain this discrepancy? And if this phenomenon is real, how might we explain its pathology?
Post-Finasteride Syndrome: What Might Cause It?
To date, there have been dozens of hypotheses surrounding how PFS might develop. All of them relate to the way finasteride works, and what might go wrong when the enzyme the drug targets is inhibited for appreciable periods of time.
Below are three theories that have received significant attention over the last few years, along with their counterarguments.
Please consider this a very brief overview of these arguments. The goal of this article is not to indoctrinate ourselves within the fine details of these hypotheses, but instead, to overview both sides of the argument, explain why this debate won’t be settled anytime soon, express our current perspectives given the data, and reveal strategies to navigate any known-unknown risks linked to finasteride.
Persistent biological changes (i.e., androgen receptor upregulation and/or downregulation)
- Argument: In vitro and animal studies suggest that when anti-androgen drugs – like spironolactone, finasteride, or flutamide – are administered, male hormones (like testosterone or dihydrotestosterone) decrease, and in response, androgen receptors increase.[10]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3116931/[11]https://pubmed.ncbi.nlm.nih.gov/21557276/ In some animal models, withdrawal from anti-androgen drugs does not lead to a rebalancing of androgen receptor expression. In other words, these receptors remain upregulated. This suggests long-lasting biological changes from finasteride use might be possible in a small subset of users, and that androgen receptor upregulation (or reflexivity) might be part of the equation for those suffering from PFS.[12]https://pubmed.ncbi.nlm.nih.gov/34247957/
- Counterargument: Human data on finasteride use and androgen receptor upregulation often conflicts with findings from in vitro and animal models.[13]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4137476/ Moreover, animal models whereby androgen receptors remained upregulated following finasteride withdrawal (1) used supraphysiological doses of finasteride, and (2) paired that drug with other anti-androgens. This doesn’t reflect normal human usage cases, and co-administration of the drugs obfuscates the ability to discern which drug is actually responsible for the phenomenon. Finally, studies on finasteride show that serum and tissue DHT levels return to normal following ~30 days of treatment withdrawal. This suggests that if finasteride is leading to any androgen receptor reflexivity or permanent upregulation, then for whatever reason, hormonal levels post-finasteride withdrawal still return to baseline.[14]https://www.ncbi.nlm.nih.gov/books/NBK513329/ Finally, studies exploring the potential for upregulation of androgen receptors in penile tissues of those claiming PFS do not use adequate controls – such as men affected by erectile dysfunction who never used the drug. Therefore, it is impossible to parcel out how many of these cases are drug-related versus just related to impotence – which affects a high number of American adults.
Persistent changes to gut microflora
- Argument: Observational studies on PFS sufferers show alterations to gut microflora versus healthy controls.[15]https://pubmed.ncbi.nlm.nih.gov/32951160/ These gut alterations in microflora might influence hormonal and immunological markers elsewhere throughout the body – particularly the skin tissues and brain. After all, studies show bidirectional feedback loops between gut microflora and serum / organ hormonal profiles, which are causally linked to disorders related to libido and mood.[16]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6962501/
- Counterargument: While this is hypothetically plausible, the one study measuring gut microflora composition on post-finasteride syndrome participants suffers from major methodological flaws – one of the biggest being a negative-control group. For instance, depression also influences gut microflora, but depressed patients were not included as a negative control in this study. How can we discern the differences between these depressed patients and any long-lasting microflora changes due to withdrawn finasteride use? Due to the limitations of this study, it’s impossible to further this hypothesis with the available data.
Persistent histological changes (i.e., tissue fibrosis and scarring)
- Argument: Subsets of PFS sufferers have reported tissue-level changes appearing since their first use of finasteride. These histological changes include, but are not limited to, penile microvascular changes and fibrosis.[17]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7354335/ There is mechanistic evidence suggesting that low DHT levels in prostatic tissues might elevate inflammatory markers that could resolve, over time, into fibrosis if left unchecked.[18]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3997870/ Therefore, perhaps PFS is caused by medically lowering DHT levels, which in a subset of patients, might increase inflammation that leads to scarring in key organ sites. When the medication is withdrawn, DHT levels return to normal, but the fibrosis / scarring that formed during the hormone’s depression remains.
- Counterargument: While this hypothesis warrants further investigation, the studies supporting this viewpoint are of very low quality due to small sample sizes and no control groups. It is important to note that upwards of 40% of American adults suffer from erectile dysfunction – with increasing prevalence per decade of life and a subset of those individuals also displaying with penile fibrosis.[19]https://www.amjmed.com/article/S0002-9343(06)00689-9/fulltext[20]https://pubmed.ncbi.nlm.nih.gov/8254833/ Without a control group, these studies make it impossible to parcel out who might believe they’re experiencing long-standing side effects from finasteride, but who are just coincidentally reaching the age at which impotence risk increases, and by coincidence of usage and the very fact that finasteride can cause sexual side effects, these participants are misplacing blame on the drug for a phenomenon that would’ve otherwise happened to them had they never used the drug anyway. Furthermore, there is no high-quality evidence of long-lasting histological changes in finasteride users after withdrawing from the drug. All indications are that hormonal profiles return to normal, and that even while on the drug, muscle morphology and subcutaneous fat stores do not change relative to controls because testosterone and other hormones can still govern these processes in replacement to lowered DHT.
Summarizing The Case Against PFS
There are rebuttals to these counterarguments, and counter-rebuttals to those rebuttals. But given these arguments and counterarguments, we’ve likely seen enough to recognize their overarching patterns:
- Yes, there’s some mechanistic and clinical evidence to support the anecdotes of symptoms befitting PFS. But…
- That evidence is of very low quality, so will remain forever scrutinized (and with good reason)
For instance, some mechanistic studies conflict with human studies, and due to small sample sizes, imperfect methodologies, and inadequate control groups, the PFS clinical studies currently available will remain open to criticism.
Moreover, because the original 1-, 2-, and 5-year studies on finasteride did not report (in their published material) any incidences of side effects not resolving after a participant withdrew from treatment, it’s incredibly difficult to parcel out finasteride’s influence on persistent erectile dysfunction versus the background risk of erectile dysfunction in adult men – which some studies suggest is 40% or higher.
Finally, PFS reports increase and decrease in congruence with media coverage on the topic, along with lawsuits against Merck for men who claim to be experiencing PFS-like effects.[21]https://www.karger.com/Article/Fulltext/497362 For what it’s worth, studies show that finasteride users have a strong tendency toward the nocebo effect – whereby simply telling a patient about the drug’s side effects leads to those patients reporting those side effects at a much higher rate than had they never been told anything. This was demonstrated in a randomized, controlled clinical study whereby a group of men who were prescribed finasteride and told it might lower their libido were nearly 500% more likely to report sexual side effects in follow-up appointments versus those who hadn’t been told that information.[22]https://www.nature.com/articles/ncpuro1012
All of this makes it scientifically challenging to parcel out a true prevalence of PFS, or even catalogue the condition as real versus imaged.
5 Barriers In The Way Of Proving PFS’ Existence
Take into consideration the following realities:
- The strong nocebo influence of finasteride
- The influence of media on PFS reporting
- The high background rates of erectile dysfunction and/or impotence in adults
- The fact that many PFS sufferers have mental health disorders – like histrionic personality disorder
- The very low quality studies exploring PFS
Given these circumstances, it might feel reasonable to dismiss PFS as a hoax condition propagated by opportunistic, delusional men looking to cash in by filing frivolous lawsuits against a pharmaceutical giant.
In fact, this is essentially the sentiment on most public hair loss forums – BaldTruthTalk, HairLossTalk and Tressless – whose users routinely mock and insult people alleging PFS, and in doing so, dissuade discussion about the topic.
If you hold this sentiment, it’s not unreasonable – particularly given the studies, arguments, and counterarguments we just outlined.
Yes, there’s reason to doubt the existence of PFS. Yes, there’s reason to question the sanity of many alleged PFS sufferers.
But that’s not the whole story.
One of the biggest counterarguments for PFS – one routinely repeated online – is actually inaccurate. Most people wouldn’t know it, mainly because of the sheer number of people blindly regurgitating it on hair loss forums.
It’s the assertion that there’s no evidence that finasteride can cause histological changes that persist after quitting the drug.
This is 100% false.
There is evidence of persistence histological changes post-finasteride withdrawal. In fact, these changes are well-studied and widely acknowledged by physicians across both aisles of the PFS debate.
The phenomenon is called finasteride-induced gynecomastia. And in a subset of cases, it doesn’t resolve after quitting the drug.
Persistent Gynecomastia: The Strongest Evidence Supporting Post-Finasteride Syndrome
Gynecomastia is the growth of male breast tissue. In men, studies causally link the development of gynecomastia to elevations in estrogen and/or prolactin.
Men who use finasteride tend to see their levels of estradiol (an estrogen) increase by 10-20%. This is a normal consequence of 5-alpha reductase inhibition, because with less available DHT formation, more free testosterone will convert into total testosterone and estradiol.
For those who have a genetic predisposition to gynecomastia, or for those whose diets, lifestyles, and environments have already elevated their estrogen and/or prolactin beyond baseline, any additional increases in estrogen from finasteride might be enough to push these men toward the development of unwanted growth of breast tissue.
This is a well-studied side effect of finasteride (and 5-alpha reductase inhibitors). It tends to affect between 0.25% to 5% of finasteride users – with a varying magnitudes of effect and prevalence depending a study’s participants (i.e., healthy young men or overweight men with benign prostatic hyperplasia).[23]https://pubmed.ncbi.nlm.nih.gov/23067029/
To be clear: there is no debate over finasteride-induced gynecomastia, or the mechanisms governing its development.
So, let’s circle back to one of the biggest counterarguments levied by people who do not believe in the plausibility of PFS.
If gynecomastia occurs in a small subset of finasteride users, then once someone stops taking finasteride, that gynecomastia should go away. Right?
Wrong.
Clinical studies show that in 80% of cases, finasteride-induced gynecomastia resolves if given enough time away from the drug.[24]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2929552/[25]https://jamanetwork.com/journals/jamadermatology/article-abstract/478759 Having said that, 20% of cases may see incomplete or no resolution – even up to six years after quitting the medication.[26]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2929552/
Under those circumstances, the only option for removal is surgery.
Persistent gynecomastia is perhaps the best example of a long-lasting histological change caused by finasteride that does not always resolve after the drug is discontinued.
The histological change is the unwanted growth of adipose and/or glandular tissue in the male breast.
This phenomenon is well-defined, well-observed, and widely-recognized amongst researchers on both sides of the PFS debate. And while the original finasteride studies did not capture this risk, post-marketing studies did.
This is because those original finasteride studies – despite having more than 1,200 participants in the finasteride group – still weren’t large enough to account for a side effect rare enough to impact only one-fifth of 0.25% of healthy finasteride users (i.e., 1 in every 2,000 people).[27]https://www.sciencedirect.com/science/article/abs/pii/S0190962298700076
With that in mind, let’s revisit the possibility and plausibility of PFS. If there are cases of finasteride-induced gynecomastia that persist even after finasteride is discontinued, does this signal that finasteride might also have a potential to histologically influence other organ sites in similar matters?
Yes.
And while these types of adverse events (if they do exist) are probably incredibly rare – much like persistent gynecomastia induced by finasteride – their existence is now plausible, because we’ve seen a similar phenomenon documented in male breast tissue.
Why The PFS Debate Is Here To Stay
In the exercise above, we revealed how an incredibly rare adverse event from finasteride – treatment-induced gynecomastia that persists even after quitting the drug – is now a recognized side effect that was not captured in the original clinical studies on finasteride. Instead, it was a side effect observed in post-marketing studies – mainly because of how few people it affects: perhaps just 1 in every 2,000 finasteride users.
Given the heated scientific debate over PFS versus the well-established acknowledgment of finasteride-induced gynecomastia, it’s probably safe to assume that if PFS is real, the number of finasteride users affected is substantially less than 1 in 2,000.
Otherwise, PFS would’ve probably been noted in finasteride’s original phase II and phase III clinical trials.
So, let’s assume (for the sake of argument) that the estimated prevalence of PFS is 1 in 5,000 finasteride users. Let’s also assume that around 40% of American adult men already have some degree of impotence – which has previously been established by several studies.
What sort of study do we need to design to prove or disprove the existence of PFS?
We would need a study that was randomized, double-blinded, placebo-controlled, and prospectively designed – as these kinds of studies are generally the only types that can infer causality.
One group of people would receive finasteride; the other group would receive a sugar pill. The study would need to run multiple years – to control for the heterogeneity in timings of onset for PFS. And it would also need a multiple-year withdrawal period to track outcomes for side effect resolution.
So, how many participants would we need to gain enough statistical power to get a definitive answer?
This is where things get incredibly difficult to parcel out.
If we estimate a “true” PFS incidence of 1 in 5,000 finasteride users (i.e., 0.02%), we must recruit enough men in this study to statistically differentiate that effect from the background risk of erectile dysfunction in 40% of adult men.
With randomization, erectile dysfunction should be equally present in both finasteride users and non-users, and at a background rate of 40%. So, we’ll need a large enough sample size to discern statistical significance between impotence reports with differences of 40% (in the placebo group) versus 40.02% (erectile dysfunction + PFS post drug withdrawal).
Then we’ll need to also find ways to account for risks of the nocebo effect and mental health disorders influencing side effect reporting – as some participants will ultimately discover that they’re using finasteride and begin researching the drug on their own. There are statistical tools that can help us account for all of the above to determine a needed sample size for significance.[28]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017493/
So, accounting for all of the above, how many participants do we need to recruit to determine – once and for all – if PFS is real?
1,000,000+ participants.
That’s right. We need more than a million study participants. That’s how much work it will take to parcel out a 0.02% increased risk of finasteride-induced erectile dysfunction persisting post-drug withdrawal from the 40% background risk of already having erectile dysfunction or having it develop for unrelated reasons during the time someone is using the medication.
That sort of study would require billions of dollars to fund, and even if it were funded, we wouldn’t have an answer until years after the study began – probably 5-10 years after its initiation.
Keep in mind that finasteride’s patent expired years ago. With these financial barriers and with no incentive for funding from large pharmaceutical companies, the likelihood of this study happening is as close to 0% as it gets.
For these reasons, debate over PFS is destined to rage on. The studies to prove or disprove its existence are too difficult to conduct.
Reconsidering The PFS Debate
With all of the evidence in mind, here are our current perspectives on PFS:
- PFS is likely real, but also probably affects fewer than 1 out of every 5,000 to 10,000 finasteride users.
- If PFS is real, its prevalence is likely overstated online due to negativity bias in public anonymous hair loss forums.
- While many people claiming PFS might instead be suffering from a psychological disorder, we’ve spoken to people alleging PFS who (1) are otherwise healthy, (2) have no psychiatric disorders, (3) have successful careers, (4) have good relationships with friends and romantic partners, (5) have never filed a lawsuit against Merck, (6) have received a PFS diagnosis by a doctor – sometimes with corroborating histological data, and (7) just want their life to go back to normal. For these reasons, PFS reports from credible individuals need to be separated from the hysteria, rather than dismissed by way of lumping in with the hysteria.
- Anyone considering finasteride should be made aware of the debate surrounding post-finasteride syndrome.
- At the same time, with a small estimated prevalence of PFS, those with AGA should consider the risk-benefit analysis of finasteride – especially in the context of what other behavioral risks people engage in on a daily basis.
PFS: Contextualizing Its Risk Vs. Other “Voluntary” Behavioral Risks
If you’re considering finasteride, but have decided against trying it because of concerns of PFS, we 100% understand.
With that said, let’s contextualize what a 1 in 5,000 (or lower) estimated risk of PFS actually looks like in the context of other risks you might take in your everyday life.
Throughout a lifetime, 1 out of every 102 Americans will die in a motor vehicle accident.[29]https://injuryfacts.nsc.org/ However, this does not stop the overwhelming majority of Americans from operating motor vehicles. While accidents are tragic and sometimes unavoidable, there are also safe-driving behaviors that might lower that risk, and in doing so, allow you all the benefits of driving.
We believe the same is true for finasteride and hair loss.
Consider the heavy psychological and emotional impact that hair loss can have (especially on younger people). Also consider the overwhelming clinical evidence on finasteride – a drug that can stop the progression of AGA in the majority of men, and for 10+ years. Now consider the debate over PFS and its loosely estimated prevalence of 1 out of every 5,000 to 10,000 finasteride users.
The decision to try or not try finasteride is entirely your own to make, along with the medical guidance of a physician. Depending on your needs, preferences, and goals – all of us will weight the above evidence and the opportunity costs of finasteride (i.e., more lost hair) differently. But if PFS is a top concern for you, we believe – much like safe driving – that there are ways to still benefit from the drug while also further lowering that ~1 in 5,000-10,000 risk.
If PFS Is Real, Can We Reduce Our Risks Of Developing It?
Currently, there are no risk factors (aside from psychiatric disorders) that might help to predict someone’s risk of PFS. But in our opinion, any strategy that might reduce side effects from finasteride may also reduce the risk of developing PFS.
By opting for lower-dose oral finasteride formulations, or by using certain topical finasteride formulations, finasteride users can not only reduce their total drug exposure over a lifetime, but also better localize the effects of the medication to the scalp.
Under both circumstances, we suspect there to be a significant risk reduction in both finasteride-linked side effects as well as PFS.
We hope this article helps, and if you’d like personal support on your hair loss journey, you can always partner with our team inside our membership community.
References[+]
References ↑1 https://pubmed.ncbi.nlm.nih.gov/32033719/ ↑2, ↑21 https://www.karger.com/Article/Fulltext/497362 ↑3, ↑5 https://www.sciencedirect.com/science/article/pii/S0022202X15529357 ↑4 https://www.oatext.com/Long-term-(10-year)-efficacy-of-finasteride-in-523-Japanese-men-with-androgenetic-alopecia.php ↑6 http://www.drproctor.com/propecia/propecia.pdf ↑7, ↑22 https://www.nature.com/articles/ncpuro1012 ↑8 https://www.fiercepharma.com/vaccines/whistleblowers-accuse-merck-of-withholding-info-on-mumps-vaccine ↑9 https://www.nature.com/articles/450324b ↑10 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3116931/ ↑11 https://pubmed.ncbi.nlm.nih.gov/21557276/ ↑12 https://pubmed.ncbi.nlm.nih.gov/34247957/ ↑13 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4137476/ ↑14 https://www.ncbi.nlm.nih.gov/books/NBK513329/ ↑15 https://pubmed.ncbi.nlm.nih.gov/32951160/ ↑16 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6962501/ ↑17 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7354335/ ↑18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3997870/ ↑19 https://www.amjmed.com/article/S0002-9343(06)00689-9/fulltext ↑20 https://pubmed.ncbi.nlm.nih.gov/8254833/ ↑23 https://pubmed.ncbi.nlm.nih.gov/23067029/ ↑24, ↑26 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2929552/ ↑25 https://jamanetwork.com/journals/jamadermatology/article-abstract/478759 ↑27 https://www.sciencedirect.com/science/article/abs/pii/S0190962298700076 ↑28 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017493/ ↑29 https://injuryfacts.nsc.org/ In terms of hair regrowth, the “best” dose for medication is typically the one that maximizes improvements and minimizes the risk of adverse events.
In the case of finasteride, 1mg daily has the most clinical support befitting a “best” dose given the risk-benefit ratio of hair improvements. However, there’s also evidence that finasteride doses as low as 0.2 mg daily may produce similar degrees of hair regrowth and reduce the risk of side effects.
Interested in Oral Finasteride?
Oral finasteride & minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Finasteride Doses: Is 1 mg The Only Dose That Works?
Is 1 mg the best dose of finasteride for hair loss? After all, oral finasteride is prescribed at 1 mg daily for androgenic alopecia and 5 mg daily for benign prostate hyperplasia. For most people, these dosages are tolerable and produce a relatively excellent safety profile. But for those interested in cutting down on a lifetime of finasteride consumption, there may be ways to reduce drug exposure by 80% without sacrificing much (or any) hair gains.
Clinical studies have demonstrated a steep, dose-dependent, logarithmic response curve for finasteride’s effects on DHT levels. That just means that a little bit of finasteride reduces almost as much DHT as a lot of finasteride. See this chart:
Serum DHT Reduction Percentage vs. Finasteride Dosages
As such, 0.2 mg daily reduces DHT levels by nearly the same as 5 mg. This is why, in some countries, it’s common to prescribe 0.2 mg of finasteride for androgenic alopecia rather than the full 1 mg dose.
Does Clinical Data Support a 0.2mg Daily Dose of Finasteride?
Yes. According to a review on finasteride:[1]https://escholarship.org/content/qt24k8q743/qt24k8q743.pdf
“In a 48-week randomized, double-blind study of finasteride treatment of androgenetic alopecia, the efficacy of 1mg and 0.2mg finasteride were compared in 414 men. The incidence of decreased libido was 2.9%, 1.5%, and 2.2% for finasteride 1mg, 0.2mg, and placebo, respectively [31]. Most of these cases resolved during the course of therapy, and there were no discontinuations of the study related to the adverse drug effects [31].”
That specific study also mentioned that:[2]europepmc.org/article/med/15319158
“All efficacy endpoints showed significant improvement with finasteride therapy by 12 weeks (p < 0.05 versus placebo). At 48 weeks, 58%, 54%, and 6% of men in the finasteride 1 mg, finasteride 0.2 mg, and placebo groups, respectively, had improved based on assessments of global photographs. All efficacy endpoints were numerically superior for the 1 mg dose over the 0.2 mg dose at 48 weeks.“
The authors did not find that the hair regrowth from 0.2 mg daily of finasteride was statistically significantly different (i.e., better or worse) than 1.0 mg daily of finasteride. So, it’s unclear whether these results regarding slightly lower efficacy (and risks of side effects) for the 0.2 mg versus 1.0 mg doses of finasteride are statistically or clinically significant.
Another 12-month study compared finasteride doses of 1 mg, 0.2 mg, and 0.01 mg daily versus placebo.[3]https://pubmed.ncbi.nlm.nih.gov/10495375/
Roberts JL, Fiedler V, Imperato-McGinley J, Whiting D, Olsen E, Shupack J, Stough D, DeVillez R, Rietschel R, Savin R, Bergfeld W, Swinehart J, Funicella T, Hordinsky M, Lowe N, Katz I, Lucky A, Drake L, Price VH, Weiss D, Whitmore E, Millikan L, Muller S, Gencheff C, et al. Clinical dose ranging studies with finasteride, a type 2 5alpha-reductase inhibitor, in men with male pattern hair loss. J Am Acad Dermatol. 1999 Oct;41(4):555-63. PMID: 10495375.
Interestingly this study found directionally stronger hair count improvements for finasteride at 1-5 mg versus 0.2 mg. The researchers also noted that, unlike the other aformentioned study, adverse events were directionally higher in the 0.2 mg group – albeit not statistically different across groups.
Roberts JL, Fiedler V, Imperato-McGinley J, Whiting D, Olsen E, Shupack J, Stough D, DeVillez R, Rietschel R, Savin R, Bergfeld W, Swinehart J, Funicella T, Hordinsky M, Lowe N, Katz I, Lucky A, Drake L, Price VH, Weiss D, Whitmore E, Millikan L, Muller S, Gencheff C, et al. Clinical dose ranging studies with finasteride, a type 2 5alpha-reductase inhibitor, in men with male pattern hair loss. J Am Acad Dermatol. 1999 Oct;41(4):555-63. PMID: 10495375.
For these reasons, the investigators concluded that 1 mg daily of finasteride is the optimal dose for androgenic alopecia (AGA).
Which Dose Of Finasteride Should I Try?
When it comes to efficacy vs. safety considerations, the evidence on dose titration of finasteride is mixed. On the one hand, some studies show directionally lower risks of side effects on 0.2 mg versus 1.0 mg daily of finasteride – albeit at the expense of slightly lower hair counts. On the other hand, other studies show no statistical risk in adverse events at 0.2 mg versus 1.0 daily of finasteride – and thus recommend the 1.0 mg dose.
What doesn’t get measured in these studies is the magnitude of each side effect. In other words, “How bad is this side effect? And does it get better on a 10-point scale when I titrate down my finasteride dose?”
In our experience working with hair loss sufferers, we routinely see a lowered magnitude of side effects when individuals go from 1.0 mg to 0.2 mg daily of finasteride. While this may come at the expense of a little more hair growth, this might be appropriate for people who are experiencing finasteride-induced side effects or who just want to take as much risk off the table, while still getting some benefit from the drug.
For others with more moderate side effects, it’s likely that topical finasteride is more appropriate.
How Can We Achieve A Dose Of 0.2 mg Daily?
To achieve a finasteride dose of 0.2 mg daily, consider the following:
- Get a prescription for 1mg of finasteride daily, then use a pill cutter to quarter the pills (so that each daily dose is now 0.25mg versus 1.0mg). This will effectively net patients the same drug exposure as 0.2mg daily.
- Get a prescription for 1mg of finasteride daily, cut the pills in half (so you have 0.5mg per daily dose), and then take one half-pill each Monday, Wednesday, and Friday. This will net patients 1.5 mg of weekly exposure, whereas 0.2mg daily would net 1.4mg weekly – so they’re more or less the same.
We hope this information helps.
References[+]
Oral finasteride, a type II 5-alpha reductase inhibitor, is one of the most effective treatments available for androgenic alopecia (AGA). However, concerns over the drug’s potential side effects prevent many men from ever considering the medication.
In the last several years, nearly a dozen studies have shown that certain formulation topical finasteride may confer the same hair growth-promoting benefits as oral finasteride, but with less systemic drug exposure. For those worried about side effects, topical finasteride is often a stepping stone toward an effective treatment protocol for hair regrowth.
In this article, we’ll uncover how to make topical finasteride using crushed pills – which is perhaps the least expensive alternative to DIY topical finasteride. We’ll also explain why doing so might be short-sighted, and that there is likely a better way to reduce costs for topical finasteride, but also control for the quality of the product: diluting topical finasteride that is already purchased.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Why Make Topical Finasteride at Home?
Most people consider making DIY topical finasteride for two reasons:
- Cost savings. Compounding pharmacies often charge $50-$100 per month for topical finasteride, thus pricing out a lot of men and women who would otherwise be interested in trying it. However, oral finasteride prescriptions are often 2-5 times cheaper on a monthly basis. This has led many to wonder, “Why don’t I save money by crushing my finasteride pills into a solution and apply that topical directly on my head?” While there are cost-savings behind this logic, the actual step-by-step process is a little more involved (more on this later).
- Control over dilutions. Most big-brand formulations of topical finasteride use dilution percentages that actually expose users to more finasteride each day than if they were to use the drug orally. For instance, Hims sells a 0.3% topical finasteride solution, of which many customers will apply 1 mL daily or more to cover all balding regions. That actually equates to 3 mg of finasteride exposure daily, which is 3 times the amount of drug prescribed daily for oral consumption (i.e., 1 mg). Under these circumstances, if just 0.2 mg of that topical drug escapes the scalp skin and enters the bloodstream, most users will experience the same systemic hormonal modifications as if they were to instead just use the oral medication.
To elaborate on that second point, just see this chart below, which shows just how little finasteride needs to be consumed to affect serum levels of dihydrotestosterone (DHT).
With that in mind, see this other cart, which shows topical finasteride’s effects on serum DHT – a proxy to estimate systemic drug exposure – while controlling for the daily exposure (in mg) of finasteride applied to the scalp. The higher the daily dose, the higher the systemic reductions to DHT.
A graph representing the daily dose exposure of topical finasteride (y-axis) versus the amount of serum DHT reductions in participants (x-axis). Across all studies referenced in the graph, topical finasteride led to hair parameter improvements.
For these reasons, many topical finasteride users prefer to have the ability to titrate their daily dosages of the topical. They can do this by:
- Using less of the topical finasteride solution. The shortcoming: with less solution, you may not be able to apply the topical to all balding regions.
- Using topical finasteride fewer days per week. The shortcoming: this throws off the rhythm of a daily routine, and at a certain threshold, reduces efficacy.
- Making their own topical finasteride. The shortcoming: it takes additional work, and it’s not always clear if you did it right.
Moreover, a lot of people presume that making their own topical finasteride is as simple as crushing their own prescription of finasteride pills into water, then applying that directly to the scalp. It isn’t.
Nonetheless, most people opt for option #3: making their own topical finasteride. And most people prefer to do this by crushing pills. While we strongly recommend getting properly formulated topical finasteride prescribed to you and made by a compounding pharmacy, for those who don’t heed this advice and instead go with the pill-crushing approach, here are some educational resources (and a free calculator) that might help you.
Making Topical Finasteride By Crushing Pills: Step-By-Step Instructions
Before proceeding, it’s important to recall what your goals are for opting to try topical finasteride. In 99% of cases, it’s going to be to minimize the risk of adverse events while maximizing the chances of growing new hair. If that is your goal, consider the following.
1. Settle on a daily dose of finasteride exposure
Serum DHT reductions act as proxies for estimate systemic absorption from topical finasteride, and thereby the risk of side effects. On that note, the only clinically studied formulation of topical finasteride that (1) demonstrated effectiveness in men and women, and (2) led to no changes in serum DHT, is one that exposed participants to ~0.1 mg daily of topical finasteride. That’s 1/10th the amount of the standard oral dose prescribed for androgenic alopecia.
This dose of topical finasteride is typically applied daily in the following formulas:
- 0.01% at 1 mL daily – good for those with localized hair loss
- 0.005% at 2 mL daily – good for those with diffuse hair loss (more topical to spread across the scalp)
So, for those who want to be as cautious as possible, this is probably the dose that is most appropriate to start for topical finasteride. Higher doses also work, and also still likely confer a reduction in side effect risk, but at the expense of guaranteed DHT reductions elsewhere in the body. With the 0.1 mg low-dose formula, this risk (according to the clinical literature) is a lot lower.
2. Consider your carrier ingredients
Carrier ingredients help carry a topical’s active ingredient into deeper layers of the skin, where it can have its desired effects. In the case of topical finasteride, carrier ingredients help bring finasteride through the stratum corneum and into the mesodermal sheath, outer root sheath, and dermal papillae cell clusters of hair follicles – where the drug can get to work inhibiting type II 5-alpha reductase and lowering scalp levels of DHT.
When it comes to topical finasteride, some carrier ingredients work better than others at enhancing skin penetration. For an example, see this chart:[1]https://ncbi.nlm.nih.gov/pmc/articles/PMC2977015/
Penetration profiles of finasteride permeating through human skin from different preparations (mean ± SD, n = 4)
There are a few key takeaways from this chart:
- Topical finasteride’s penetration into the skin is linear across 4 common carrier agents. That means the longer you leave in the topical without washing your hair, the more of it will absorb into the skin.
- This enhanced skin penetration will also come at the expense of higher systemic absorption of the drug. For these reasons, we recommend serum DHT testing regularly with topical finasteride. Our membership has resources on how to do this, and we can team members and researchers who will personally support you through this entire process if you need it.
- Don’t just mix your finasteride pills with water. As we can see from the chart, water is a terrible carrier ingredient for topical finasteride.
In our topical finasteride calculator (it’s free), we recommend a series of low-cost carrier ingredients for you, as well as links to the actual products. Please note: we do not receive commissions on any of those product recommendations, as doing so would undermine the objectives of this site: to be as unbiased as possible in our scientific analyses (and advice) to hair loss sufferers.
3. Before crushing your finasteride pills, remove any pill coatings
Depending on where your finasteride pills were manufactured, there’s a strong likelihood that the pills come with a protective coating that prevents incidental drug exposure from anyone who might’ve handled the drug without the intention of ingesting it. This is generally to prevent pregnant women from coming into incidental contact with the drug.
As such, if you’re going to use your prescribed finasteride pills to make topical finasteride, it’s critical to remove this protective coating from each pill in order to allow those pills a better chance at dissolving into the topical solution. You can do this by scraping the pills with a small knife or nail clipper, and then peeling off all of the coating with your finger tips.
4. Use our topical finasteride calculator to dial in your DIY, homemade topical finasteride formulation
The math involved in making topical finasteride isn’t likely solving an equation for quantum physics. At the same time, it’s also not as straightforward as many people would like. After all, you have to account for the following:
- Hair loss patterning (localized vs. diffuse) – as this determines if you’ll need 1 mL or 2 mL of liquid daily to cover all balding regions
- Dilution amounts – which, together with the mL of daily application, will determine your daily total finasteride exposure
- Adjustments for pill sizes (in mg). After all, oral finasteride pills are available in 1 mg and 5 mg daily doses, so you’ll need to account for this prior to crushing anything
To take the guesswork out of this process, we decided to do all of the math for you. Then we hired developers to integrate these math equations into an interactive survey that factors in all of the above, then spits out step-by-step instructions for how to make topical finasteride by crushing pills.
You can access the topical finasteride calculator right here. It’s 100% free.
To reiterate, this calculator is not medical advice and is for educational purposes only. We still strongly recommend that you just get your topical finasteride properly formulated by a compounding pharmacy. Nonetheless, the calculator is there for those who decide to ignore this advice and instead take the cost-savings route toward topical hair loss treatments.
Final Thoughts
We produce content like this to benefit hair loss sufferers worldwide – regardless of their financial circumstances. With more access to free information, more men and women can seek effective hair loss treatments faster, and thereby improve their outcomes long-term.
With that said, these free resources represent just a tiny fraction of what’s available inside our membership community. If you’re looking for personal support on your hair growth journey, interactions with hair loss researchers, one-on-one video calls, and a customized hair growth protocol built around your needs, preferences, goals, and the evidence – our membership is the place where we offer these services.
It’s also the way in which we monetize this site, which is why we’ve never accepted any hair loss product advertisements or commissions – which otherwise comes with the risk of biasing our own research lens and interpretation of data. For evidence of how big this problem is, just take a look all of the other sites, forums, and YouTube personalities catering their content toward the sale of physical products to which they’re financially tied – which only serves those creators and, simultaneously, overwhelms the ecosystem of information accessible to consumers with biased advice.
Not a member of the Perfect Hair Health Membership Community? Join today to create a customized regrowth roadmap and gain access to hundreds of resources, including treatment guides, product reviews, expert interviews, forums, and more.
IngredientsPharmaceuticalsNatural RemediesCompany ReviewsBy Sarah King, PhDJan 17, 2025New Study: Does Finasteride Cause Birth Defects?
A recent study has raised concerns about paternal finasteride use and cryptorchidism (undescended testicles) in offspring, but does the data actually support a causal link? The study, based on FAERS reports, shows a statistical association—but not proof of risk. Issues like reporting bias, lack of a...By Sarah King, PhDJan 14, 2025Can Intermittent Fasting Cause Hair Loss? A Look Into A New Study
Intermittent fasting has gained popularity for its potential health benefits, but recent research highlights its possible impact on hair health. Studies on mice and humans suggest that fasting-induced metabolic shifts can slow hair growth and weaken hair shafts by depleting activated hair follicle s...By Ben Fletcher, PhDJan 13, 2025Burdock Root For Hair Loss? A Look Into The Evidence
Burdock root, derived from the plant Arctium lappa, has long been used in traditional medicine for its purported anti-inflammatory, antimicrobial, and antioxidant properties. In recent years, it has been included in natural hair loss treatments, with claims that it promotes hair growth. Some studies...By Sarah King, PhDDec 11, 2024Which Vitamin Deficiences Can Cause Hair Loss?
Hair loss is a complex issue influenced by various factors, including vitamin deficiencies. We explored the impact (or lack thereof) of deficiencies in five vitamins – Vitamin D, Biotin, Vitamin B12, Vitamin E, and Vitamin A – on hair health and whether supplementation can aid hair regrowth. While d...By Perfect Hair Health TeamNov 21, 2024Genetic Tests: A Breakthrough for Personalized Hair Loss Treatments?
Genetic testing is trending in the hair loss industry. The premise? Our genes hold the secrets to better hair growth, and genetic tests can help hair loss sufferers unlock new levels of hair gains with customized treatments. It’s an enticing proposition, albeit one that holds little-to-no scie...By Sarah King, PhDNov 8, 2024Do Chinese Herbs Help Regrow Hair? A Look At Traditional Remedies
Hair loss treatments have expanded beyond pharmaceuticals to include Traditional Chinese Medicine (TCM) herbs, which some enthusiasts claim help support hair growth. We reviewed the scientific evidence behind four well-known herbs: Polygonum multiflorum (Fo-Ti), Panax ginseng, Lycium chinense (Goji ...By Sarah King, PhDOct 11, 2024Cannabidiol (CBD) Increases Hair Counts By 246%? Not So Fast.
Cannabidiol (CBD), a non-psychoactive compound from Cannabis sativa, is being explored for hair regrowth due to its anti-inflammatory, antioxidant, and circulation-boosting properties. Small studies on CBD topicals for androgenic alopecia (AGA) show hair count increases between 55% and 246% over six...By Sarah King, PhDSep 27, 2024Creatine: Does It Worsen Hair Loss? It Depends On The Hair Loss Type. – 2025 Update
Creatine, a substance that supports energy production in the muscles and brain, is commonly used as a supplement to boost athletic performance. However, its potential link to hair loss has raised concerns, particularly due to its effect on dihydrotestosterone (DHT), a hormone associated with androge...By Sarah King, PhDSep 18, 2024Can Progesterone Improve Hair Regrowth?
Progesterone is a hormone that plays a vital role in female reproductive health. Deficiencies in progesterone have been linked to hair thinning, particularly in conditions like female pattern hair loss (FPHL) and postpartum telogen effluvium (PPTE). While natural progesterone seems to have 5-alpha-r...By Ben Fletcher, PhDSep 10, 2024CRABP2: Can This Gene Predict Regrowth From Retinoids?
The CRABP2 gene, which plays a role in retinoic acid metabolism, has been linked to hair health. Retinoic acid, a derivative of vitamin A, is known to influence hair growth, and some studies suggest CRABP2 may also be involved. However, the evidence connecting CRABP2 variants to hair loss and treatm... - Mission Statement
 Scroll Down
Scroll Down