- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
Scroll Down
Popular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Free CalculatorTopical Finasteride Calculator
- Free Interactive GuideInteractive Guide: What Causes Hair Loss?
- Free ResourceFree Guide: Standardized Scalp Massages
- Free Course7-Day Hair Loss Email Course
- Free DatabaseIngredients Database
- Free Interactive GuideInteractive Guide: Hair Loss Disorders
- Free DatabaseTreatment Guides
- Free Lab TestsProduct Lab Tests: Purity & Potency
- Free Video & Write-upEvidence Quality Masterclass
- Free Interactive GuideDermatology Appointment Guide
More
Articles100+ free articles.
-
Oral Minoxidil – Ultimate Guide
-
Introducing Ulo: The Future of Hair Loss Telemedicine
-
OS-01 Hair Review: Does It Live Up to the Hype?
-
Stretching The Truth: 3 Misrepresented Claims From Hair Loss Studies
-
Minoxidil Shedding – What to Expect & When it Stops
-
Does Minoxidil Cause Skin Aging?
-
Thermus Thermophilus Extract Does Not Increase Hair Density By 96.88%, Despite Dermatology Times’ Claims.
-
Does Retinoic Acid (Tretinoin) Improve Hair Growth From Minoxidil?
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
Before-Afters- Transformation Photos
Our library of before-after photos.
- Client Testimonials
Read the experiences of members
Before-Afters/ Client Testimonials- Popular Treatments
-
TreatmentsTopical Minoxidil
Evidence97%RegrowthViabilityOral Minoxidil
Evidence63%RegrowthViability-
Topical
-
Oral
-

Evidence Quality
97%
Regrowth Potential
Long-Term Viability
Written by Perfect Hair Health TeamMedically Reviewed by Rob EnglishFirst Published Oct 3, 2024Last Updated Oct 24, 2024Key Information
Free Resources
KEY INFORMATIONWhat Is Minoxidil?
Minoxidil is a drug that lowers blood pressure. In the 1980's, topical minoxidil was approved by the FDA to treat androgenic alopecia at 2% strengths for women and 5% strengths for men. Today, minoxidil is available in oral and topical formulations.
How Does Minoxidil Work?
Minoxidil is believed to promote hair growth by opening potassium ion channels, which then promotes blood flow and angiogenesis (the formation of new blood vessel networks). Minoxidil may also have anti-inflammatory effects. Its primary mechanism of action remains unclear.
What You Should Know
Topical minoxidil is largely ineffective at treating hair loss – with studies suggesting response rates of just 40-60%. However, response rates and regrowth rates can be greatly enhanced when minoxidil is paired microneedling and/or topical retinoic acid. Finally, low-dose minoxidil seems to producer higher response rates and a good safety and adherence profile – all without the same risk of sexual side effects as finasteride.
-
Evidence Quality
63%
Regrowth Potential
Long-Term Viability
Written by Perfect Hair Health TeamMedically Reviewed by Rob EnglishFirst Published Oct 3, 2024Last Updated Oct 24, 2024Key Information
Free Resources
KEY INFORMATIONWhat Is Minoxidil?
Minoxidil is a drug that lowers blood pressure. In the 1980's, topical minoxidil was approved by the FDA to treat androgenic alopecia at 2% strengths for women and 5% strengths for men. Today, minoxidil is available in oral and topical formulations.
How Does Minoxidil Work?
Minoxidil is believed to promote hair growth by opening potassium ion channels, which then promotes blood flow and angiogenesis (the formation of new blood vessel networks). Minoxidil may also have anti-inflammatory effects. Its primary mechanism of action remains unclear.
What You Should Know
Topical minoxidil is largely ineffective at treating hair loss – with studies suggesting response rates of just 40-60%. However, response rates and regrowth rates can be greatly enhanced when minoxidil is paired microneedling and/or topical retinoic acid. Finally, low-dose minoxidil seems to producer higher response rates and a good safety and adherence profile – all without the same risk of sexual side effects as finasteride.
FREE RESOURCESArticles
Explore the science behind hair loss and hair growth. Our in-depth articles cover topics ranging from natural remedies to pharmaceuticals to breakthroughs in hair loss science. Want to request an article topic? Contact us.
By Sarah King, PhDJul 9, 2025Oral Minoxidil – Ultimate Guide
Oral minoxidil, once a blood pressure medication, is now gaining traction as a powerful off-label treatment for hair loss. But how does it compare to topical minoxidil, and is it safe? In this article, we explore the mechanisms behind oral minoxidil’s hair growth effects, its role in treating differ...By Perfect Hair Health TeamJul 8, 2025Introducing Ulo: The Future of Hair Loss Telemedicine
Ulo is a new telehealth brand focused exclusively on hair growth. With its commitments to evidence, personalization, & consumer safety, the company aims to provide best-in-class products that have not only been independently lab tested, but also offer a level of customization unrivaled by other ...By Ben Fletcher, PhDMay 19, 2025Does Minoxidil Cause Skin Aging?
Online discussions have raised alarms about a possible link between minoxidil and premature skin aging, especially among users reporting under-eye puffiness, dryness, and fine lines. Could a hair loss treatment really be affecting facial skin quality? This article takes a balanced look at the scienc...By Sarah King, PhDFeb 6, 2025Minoxidil Side Effects: Everything You Need To Know
Minoxidil is an FDA-approved treatment for androgenic alopecia, but its use can come with side effects – from mild scalp irritation to cardiovascular risks. This comprehensive guide assess common and rare side effects from topical minoxidil and oral minoxidil – along with mitigation strategies....By Perfect Hair Health TeamNov 21, 2024Genetic Tests: A Breakthrough for Personalized Hair Loss Treatments?
Genetic testing is trending in the hair loss industry. The premise? Our genes hold the secrets to better hair growth, and genetic tests can help hair loss sufferers unlock new levels of hair gains with customized treatments. It’s an enticing proposition, albeit one that holds little-to-no scie...By Sarah King, PhDAug 21, 2024PTGES2: Can This Gene Predict Regrowth from Minoxidil?
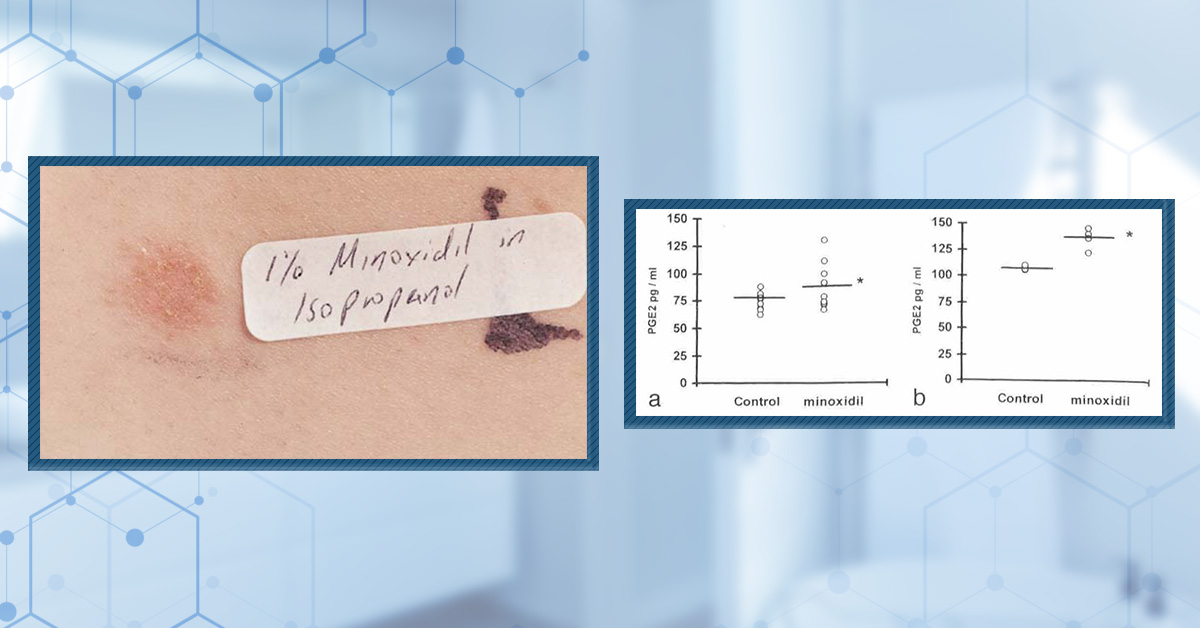
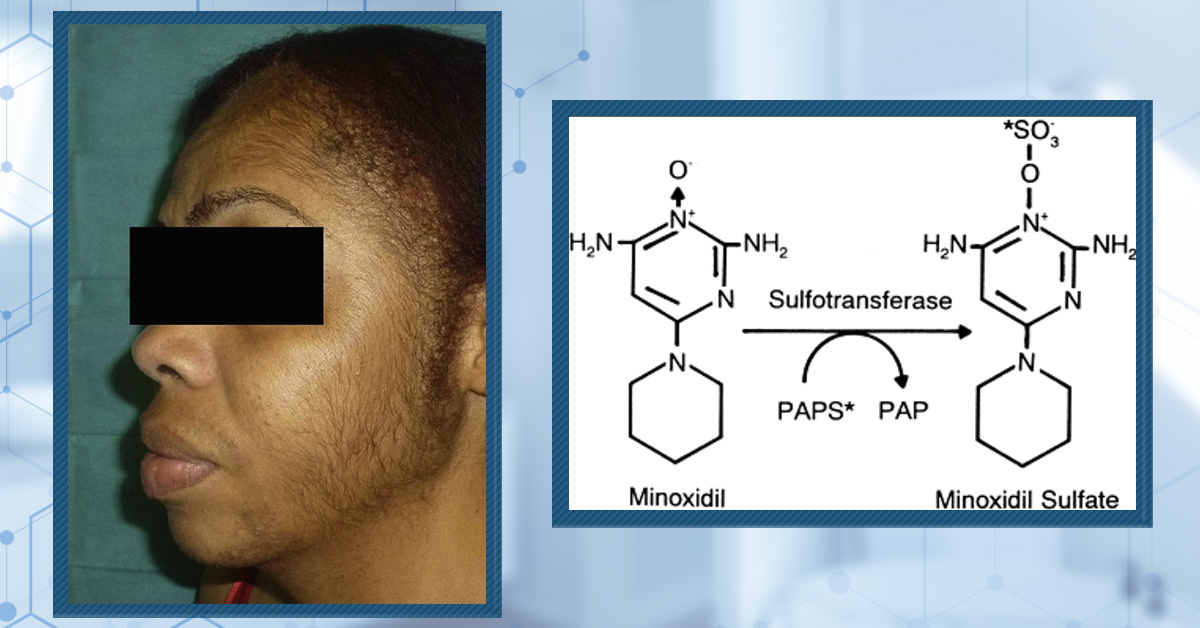
The PTGES2 gene encodes the enzyme prostaglandin E synthase 2, which is crucial for converting prostaglandin H2 to prostaglandin E2 (PGE2). This enzyme plays a significant role in various physiological processes, including inflammation and hair growth. Research has indicated that an SNP in the PTGES...By Sarah King, PhDJul 16, 2024SULT1A1: Can This Gene Predict Hair Regrowth From Minoxidil? | The Evidence
Can your genes predict minoxidil effectiveness? The SULT1A1 gene, which encodes sulfotransferase, might hold the key, at least according to gene testing companies. SULT1a1 codes for an enzyme that activates minoxidil, a common hair loss treatment. While some studies suggest certain SULT1A1 variants ...By Sarah King, PhDApr 11, 2024Is Hair Loss Treatment Lifelong? Here’s What The Data Show.
It can be daunting to think of hair loss treatments as a lifelong commitment. And for most cases of androgenic alopecia, this is true. However, starting treatment does not necessarily mean you must commit to a lifetime of treatment. Studies suggest that after stopping a hair loss treatment, hair los...By Perfect Hair Health TeamFeb 24, 2023Regrowth from Minoxidil: How Much Should I Expect?
How much regrowth can we expect from minoxidil? As with any hair loss treatment, it depends on a number of factors: genetic variance in the SULT1A1 gene, the delivery method of minoxidil (oral vs. topical), the dosing amount and schedule, and if minoxidil is combined with interventions that might en...By Perfect Hair Health TeamFeb 23, 2023How Does Minoxidil Work? 3 Hypotheses + Debates
Despite decades of study and FDA approval, researchers still aren’t sure exactly how minoxidil regrows hair. Over the last few years, investigators have explored a number of hypothetical mechanisms ranging from vasodilation to prostaglandin modulation to anti-androgenic effects. In this articl...By Perfect Hair Health TeamNov 24, 2022I Am Experiencing Side Effects From Topical Minoxidil. What Should I Do?
Topical minoxidil is one of the only FDA-approved drugs for androgenic alopecia. Unfortunately, topical minoxidil appears to induce skin irritation in 2-7% of users, with online users also reporting accelerated aging and/or a worsening of under-eye bags. A small percentage of users have also experie...By Perfect Hair Health TeamApr 16, 2022Hims vs Keeps vs Roman: Which Hair Growth Subscription Service Wins?
Hair growth subscription services are sprouting up everywhere online. Among them, three companies have emerged from the pack: Hims, Keeps, and Roman. Each company offers two FDA-approved hair loss treatments, as well as other add-on products (supplements, gummies, etc). In this post, the Perfect Hai...By Perfect Hair Health TeamMar 10, 2022How Long After Stopping Minoxidil Before We Lose Our Hair Gains?
Studies show that within 3 months of quitting minoxidil, any new hair growth is lost and, worryingly, our hair loss temporarily worsens before returning to baseline. But encouragingly, new studies are revealing potential ways to mitigate any shedding related to minoxidil withdrawals. In fact, a 2020...By Perfect Hair Health TeamMar 5, 2022Three Ways to Improve Minoxidil Results
Minoxidil is one of the most widely used hair loss products on the market. And yet, so much about this growth activating “pro-drug” remains unknown. Despite its FDA approval, results are not guaranteed. In fact, around 50% of hair loss sufferers are non-responders. Recent research sugges...By Perfect Hair Health TeamJan 3, 2017Why Most Hair Loss Topicals Fail To Regrow Hair
People often ask me if a new topical mentioned by a doctor, website, or hair loss forum will help regrow their hair. Here’s a running list from my emails just last week: Emu oil Argan oil Castor oil Coconut oil Onion juice Shea butter Egg yolk Rogaine In the last decade, if there’s any...FREE RESOURCESArticles
Explore the science behind hair loss and hair growth. Our in-depth articles cover topics ranging from natural remedies to pharmaceuticals to breakthroughs in hair loss science. Want to request an article topic? Contact us.
By Sarah King, PhDJul 9, 2025Oral Minoxidil – Ultimate Guide
Oral minoxidil, once a blood pressure medication, is now gaining traction as a powerful off-label treatment for hair loss. But how does it compare to topical minoxidil, and is it safe? In this article, we explore the mechanisms behind oral minoxidil’s hair growth effects, its role in treating differ...By Perfect Hair Health TeamJul 8, 2025Introducing Ulo: The Future of Hair Loss Telemedicine
Ulo is a new telehealth brand focused exclusively on hair growth. With its commitments to evidence, personalization, & consumer safety, the company aims to provide best-in-class products that have not only been independently lab tested, but also offer a level of customization unrivaled by other ...By Ben Fletcher, PhDMay 19, 2025Does Minoxidil Cause Skin Aging?
Online discussions have raised alarms about a possible link between minoxidil and premature skin aging, especially among users reporting under-eye puffiness, dryness, and fine lines. Could a hair loss treatment really be affecting facial skin quality? This article takes a balanced look at the scienc...By Sarah King, PhDFeb 6, 2025Minoxidil Side Effects: Everything You Need To Know
Minoxidil is an FDA-approved treatment for androgenic alopecia, but its use can come with side effects – from mild scalp irritation to cardiovascular risks. This comprehensive guide assess common and rare side effects from topical minoxidil and oral minoxidil – along with mitigation strategies....By Perfect Hair Health TeamNov 21, 2024Genetic Tests: A Breakthrough for Personalized Hair Loss Treatments?
Genetic testing is trending in the hair loss industry. The premise? Our genes hold the secrets to better hair growth, and genetic tests can help hair loss sufferers unlock new levels of hair gains with customized treatments. It’s an enticing proposition, albeit one that holds little-to-no scie...By Sarah King, PhDAug 21, 2024PTGES2: Can This Gene Predict Regrowth from Minoxidil?
The PTGES2 gene encodes the enzyme prostaglandin E synthase 2, which is crucial for converting prostaglandin H2 to prostaglandin E2 (PGE2). This enzyme plays a significant role in various physiological processes, including inflammation and hair growth. Research has indicated that an SNP in the PTGES...By Sarah King, PhDJul 16, 2024SULT1A1: Can This Gene Predict Hair Regrowth From Minoxidil? | The Evidence
Can your genes predict minoxidil effectiveness? The SULT1A1 gene, which encodes sulfotransferase, might hold the key, at least according to gene testing companies. SULT1a1 codes for an enzyme that activates minoxidil, a common hair loss treatment. While some studies suggest certain SULT1A1 variants ...By Sarah King, PhDApr 11, 2024Is Hair Loss Treatment Lifelong? Here’s What The Data Show.
It can be daunting to think of hair loss treatments as a lifelong commitment. And for most cases of androgenic alopecia, this is true. However, starting treatment does not necessarily mean you must commit to a lifetime of treatment. Studies suggest that after stopping a hair loss treatment, hair los...By Perfect Hair Health TeamFeb 24, 2023Regrowth from Minoxidil: How Much Should I Expect?
How much regrowth can we expect from minoxidil? As with any hair loss treatment, it depends on a number of factors: genetic variance in the SULT1A1 gene, the delivery method of minoxidil (oral vs. topical), the dosing amount and schedule, and if minoxidil is combined with interventions that might en...By Perfect Hair Health TeamFeb 23, 2023How Does Minoxidil Work? 3 Hypotheses + Debates
Despite decades of study and FDA approval, researchers still aren’t sure exactly how minoxidil regrows hair. Over the last few years, investigators have explored a number of hypothetical mechanisms ranging from vasodilation to prostaglandin modulation to anti-androgenic effects. In this articl...By Perfect Hair Health TeamApr 16, 2022Hims vs Keeps vs Roman: Which Hair Growth Subscription Service Wins?
Hair growth subscription services are sprouting up everywhere online. Among them, three companies have emerged from the pack: Hims, Keeps, and Roman. Each company offers two FDA-approved hair loss treatments, as well as other add-on products (supplements, gummies, etc). In this post, the Perfect Hai...By Perfect Hair Health TeamMar 10, 2022How Long After Stopping Minoxidil Before We Lose Our Hair Gains?
Studies show that within 3 months of quitting minoxidil, any new hair growth is lost and, worryingly, our hair loss temporarily worsens before returning to baseline. But encouragingly, new studies are revealing potential ways to mitigate any shedding related to minoxidil withdrawals. In fact, a 2020...By Perfect Hair Health TeamMar 5, 2022Three Ways to Improve Minoxidil Results
Minoxidil is one of the most widely used hair loss products on the market. And yet, so much about this growth activating “pro-drug” remains unknown. Despite its FDA approval, results are not guaranteed. In fact, around 50% of hair loss sufferers are non-responders. Recent research sugges...By Perfect Hair Health TeamJan 17, 2020Oral Minoxidil For Female Hair Loss: How To Avoid Hypertrichosis (Unwanted Body Hair Growth)
Oral minoxidil improves hair loss in women, but at the expense of unwanted body hair growth. Fortunately, there is a way to leverage oral minoxidil’s hair-promoting effects and without much body hair growth: combine it with spironolactone. This article reviews the evidence on oral minoxidil fo...By Perfect Hair Health TeamJan 6, 2020Oral Minoxidil: What’s The Best Dose (mg) For Men With Pattern Hair Loss?
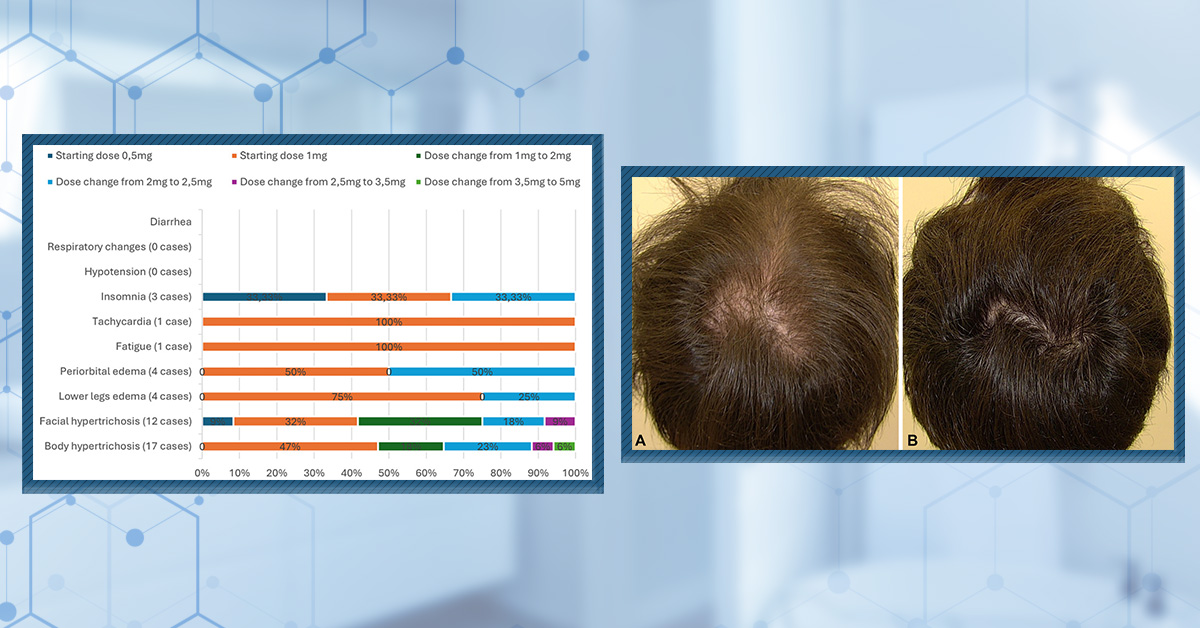
Oral minoxidil improves hair growth in men with androgenic alopecia (AGA), with dosages of 0.25mg, 2.5mg, and 5.0mg showing positive effects. But the higher the dose, the higher your risk of side effects: namely, body hair growth and lower limb edema (swelling). So, which dose is best for you? While...-
FREE RESOURCES
Research Tables
Want the latest research on Topical Minoxidil? Every quarter, our research team conducts a literature search on Topical Minoxidil to keep you up-to-date on new studies. See our search criteria & research tables below – including a summary of key findings from every single study.
Last updated: October 2024
Results
Search Criteria
Parameter
Inclusion Criteria
Exclusion Criteria
Patients Patients of any age with hair loss Patients with no hair loss disorder. Intervention Topical minoxidil as a standalone or adjunct therapy. A study that doesn’t contain topical minoxidil either as a standalone or adjunct therapy Comparator Placebo and/or other therapies Lack of control group (positive or negative) Outcomes Primary Endpoints of phototrichogram, investigator, and/or patient assessments. Any study not designed to adequately test for the standalone or additive effect of topical minoxidil Study Design Prospective, retrospective, and case series studies Literature reviews, non-human subjects, or ongoing clinical trials. Search Terms
Search Terms:
topical hair loss alopecia minoxidil-
Abbreviations:
-
FPHLFemale pattern hair loss
-
AGAAndrogenetic alopecia
-
AAAlopecia areata
-
MXMinoxidil
-
MTFTopical minoxidil foam
-
MXTTopical minoxidil
-
MNMicroneedling
-
PRPPlatelet-rich plasma
-
TAHCTarget area non-vellus hair count
-
AUAlopecia Universalis
-
ATAlopecia Totalis
-
AASISAlopecia Areata Symptom Impact Scale
-
SALTSeverity of Alopecia Scoring Tool
-
FGFFibroblast growth factor
-
SPTSpironolactone
-
RCTRandomized controlled trial
-
qPCRQuantitative polymerase chain reaction
-
TUADTotal unit area density
-
CIAChemotherapy-induced alopecia
Summarized Studies
Study Participants Design Treatment Results Key Takeaway Adverse Effects Evidence Quality Authors (year) Sex Hair Loss Type Design Dose Usage Duration Endpoints Hair Growth Assessments Summary Limitations Adverse Effects Jadad Score Liang et al. (2023) n=120 (F)
Group 1: 40
Group 2: 40
Group 3: 40FPHL
Prospective, single-center, parallel-group, evaluator-blinded, randomized trial Group 1: 5% MXT
Group 2: 5% MX + 80-100 mg SPT
Group 3: 5% topical MX + MNGroup 1: Once daily.
Group 2: Once daily.
Group 3: MXT once daily, alongside MN every 2 weeks.24 weeks Dermascope evaluation, ultrasound biomicroscopy (UBM), physician's global assessment, and patient assessment. Group 1:showed improvement at week 24 in hair density and shaft diameter. The effective rate was 55.27% at week 24.
Group 2:
The effective rate was 86.49% at week 24.
Group 3: The effective rate was 95% at week 24.
The degree of improvement of hair density at week 24 in Group 1 was less than in the latter two.The combined therapies showed advantages in efficacy over 5% MXT alone. Group 3 showed significant improvement in most endpoints, including hair density, hair shaft, diameter, epidermal thickness, dermis thickness, follicle diameter, hair shedding score, and QoL score Small sample size, exclusion of severe FPHL patients, and potential bias from unblinded treatments among the 3 groups. Group 1: Facial hypertrichosis (n=4), trichomadesis aggravating (n=4), scalp pruritus (n=8), increased scurf (n=7), headache (n=1), palpitation (n=1), postural hypotension (n=1), urticaria (n=1).
Group 2: facial hypertrichosis (n=5), trichomadesis aggravating (n=4), scalp pruritus (n=8), increased scurf (n=6), edema (n=1), headache (n=1), palpitation (n=3), hyperkalemia (n=1), menstrual disorder (n=15), urticaria (n=1)4Hassan et al. (2022) n=60 (F) Group 1: 15 Group 2: 15 Group 3: 15
+ 15 controls for vitamin D comparison.FPHL
Comparative study. Group 1: 5% MTF and oral vitamin D3 (5000 IU/day). Group 2: 5% MTF only.
Group 3: Oral vitamin D3 (5000 IU/day)Group 1: 6 puffs twice daily of MTF and 5000 IU/day. Group 2: 6 puffs of MTF twice daily. Group 3: 5000 IU/day. 12 weeks Clinical evaluation (Ludwig scale) and dermoscopy. Group 1: reduction in thin hairs to 10.47 ± 6.94 from 23.33 ± 7.94. Improvement in Ludwig classification: 6.7% in stage 0, 80% in stage I, and 13.3% in stage 2.
Group 2: reduction of thin hairs to 16.67 ± 9.23 from 23.33 ± 8.8. Improvement in Ludwig classification: 13.3% in stage 0, 53.3% in stage I, 33.3% in stage II.
Group 3: reduction of thin hairs to 24.33 ± 10.67 from 28.33 ± 9.39. Improvement in Ludwig classification: 6.7% in stage 0, 53.3% in stage I, and 40% in stage II.Vitamin D treatment alone had no notable effect on hair growth compared to MX or combination therapy. A combination of MX and vitamin D appeared to improve hair growth outcomes the most. Small sample size. Not reported. 0Bao et al. (2022) N=71 (M)
Group 1: 23
Group 2: 23
Group 3: 25AGA
RCT Group 1: 5% MXT
Group 2: Electrodynamic MN treatment
Group 3: Combination of MXT and MN treatment.Group 1: twice daily
Group 2: every 3 weeks (8 treatments total) treatment
Group 3: once daily MXT + every 3 weeks (8 total treatments).24 weeks followed by a 6-month follow-up period. Non-vellus hair density and diameter, hair growth evaluation, qPCR microarray, protein expression. Hair density: All 3 groups showed significantly increased non-vellus hair density (p= <0.05):
Group 1 – 28.01 ± 7.42, Group 2 – 32.09 ± 4.51, and Group 3 – 56.45 ± 7.82.
Hair diameter: Group 1 and group 3 showed significant improvements (p=<0.01).
Group 1: 18.70 ± 6.17 µm, Group 2: 10.41 ± 4.83 µm, and Group 3 – 22.46 ± 3.87 µm.Combination treatment of MXT and MN showed the most improvement in non-vellus hair density and hair diameter Small sample size, participants in the combination group received scalp massages. 12 people had adverse reactions.
Group 1: seborrheic dermatitis (n=1), scalp itching (n=1), eczema (n=1).
Group 2: increased dandruff (n=2), scalp infection (n=1), enlarged lymph nodes in the neck (n=1).
Group 3: seborrheic dermatitis (n=1), increased dandruff (n=1), enlarged lymph nodes (n=3).3Singh et al. (2019). n=80. (M)
Group 1: 20
Group 2: 20
Group 3: 20
Group 4: 20AGA
RCT, double-blind, placebo-controlled. Group 1: 5% MXT.
Group 2: 5% MXT + intradermal injection of PRP.
Group 3: topical placebo and intradermal placebo injection.
Group 4: topical placebo and intradermal injection of PRP.Group 1: twice daily.
Group 2: twice daily topical + once monthly intradermal injection.
Group 3: twice daily topical + once monthly intradermal injection.
Group 4: twice daily topical + once monthly intradermal injection12 weeks followed by 2 months of follow-up. Change in total, terminal, vellus, and non-vellus hair density, change in degree of hair pigmentation, patient self-assessment of hair loss using the visual analog scale, and assessment of hair loss by investigators using the 7-point Sinclair scale. Global photographic assessment (GPA) of hair density and thickness. Hair Density: By the final follow-up,
Group 1: 123.95 ± 35.41
Group 2: 150.45 ± 28.27
Group 3: 89 ± 37.39
Group 4: 143.2 ± 33.35
Patient satisfaction: Found to be highest in group 2, followed by Group 4 and Group 1, whereas none were satisfied in group 4.PRP with MXT was found to be more effective than PRP or topical MXT alone in treating male-type baldness. Lack of long-term follow-up, no hair counts or thickness measurements, and the use of patient self-assessment as a subjective measure By the final follow-up:
Group 1: scalp pruritus (n=3), increased facial hair (n=1), hyperpigmentation (n=1).
Group 2: increased facial hair (n=1).
Group 3: no adverse effects.
Group 4: no adverse effects.3Blume-Peytavi et al (2019). N=220 (M)
Group 1: 110
Group 2: 44
Group 3: 44
Group 4: 22AGA
Phase II multicenter, double-blind, randomized, placebo-controlled, split scalp study. Group 1: 5% MXT (DCO120) + comparator.
Group 2: 5% MXT (DCO120) + comparator vehicle.
Group 3: DCO120 vehicle + comparator.
Group 4: DCO120 vehicle + comparator vehicle.Products are applied twice daily morning and evening. 16 weeks Trichoscan, cumulative hair thickness, safety, and tolerability. Non-vellus TAHC:
At 16 weeks, both DCO120 and the comparator showed an increase in non-vellus TAHC. Change from baseline = +22 hairs/cm2 and +20.5 hairs/cm2 respectively.
Hair thickness: Significantly increased following both DCO120 and comparator treatments compared to the vehicles.
Heart rate, systolic blood pressure, and diastolic blood pressure remained stable over the treatment period.The study demonstrated that the new topical minoxidil was non-inferior to the comparator in stimulating hair growth over 16 weeks. The treatment was generally well-tolerated, with mild or moderate treatment-related adverse events. Products were only applied to small areas of the scalp, and the study was not large enough to detect less common adverse events 3 subjects discontinued the study because of AEs related to the study treatment:
Group 1 – contact dermatitis (n=1), erythema (n=1).
Group 2 – contact dermatitis (n=1).
When present, erythema, pruritus, and burning sensation at application sites were generally mild and did not worsen during the study.4Bergfeld et al (2016). n=404 (F)
Group 1: 202
Group 2: 202FPHL
Phase III, multicenter, parallel-design clinical trial. Group 1: 5% MTF.
Group 2: Vehicle foam.Both treatments = once daily. 24 weeks Change from baseline in target area hair count (TAHC) at weeks 12 and 24, subject assessment of scalp coverage, and change from baseline in total unit area density (TUAD). At 12 and 24 weeks, 5% MTF treatment resulted in regrowth of 10.9 hairs/cm2 and 9.1hair/cm2 more than the vehicle foam respectively (P<0.0001).
Improved scalp coverage was observed at week 24 over vehicle foam (P<0.0001).
TUAD increased by 658 µm/cm2 and 644 µm/cm2 with 5% MXT than the vehicle foam (P<0.0001).5% MTF once daily for 24 weeks was well-tolerated and promoted hair regrowth in women, leading to improved scalp coverage and increased hair density compared to the vehicle. Not specified 5% MTF was well tolerated with a low incidence of scalp irritation and facial hypertrichosis observed. 3Blume-Peytavi et al. (2016) n=322 (F)
5: 161
Group 2: 161FPHL
Phase III, randomized, investigator-blinded study. Group 1: 5% minoxidil topical foam (MTF).
Group 2: 2% minoxidil topical (MXT).MTF = once-daily.
MXT = twice daily.52 weeks Change from baseline in total area hair count (TAHC) at 12 and 24 weeks. Total unit hair density and change in overall scalp coverage. Once-daily 5% MTF increased TAHC from baseline by 23.9 ± 2.1 hairs/cm2 by week 24. Twice-daily 2% MXT increased TAHC 24.2 ± 2.1 hairs/cm2 at week 24. While both groups were able to induce hair regrowth, the MTF group could not meet the non-inferiority criteria. Not specified Both treatments were reported to be well tolerated.
10 total participants withdrew due to adverse effects.3Mirmirani et al. (2015). n=16 (M)
Group 1: 10
Group 2: 6AGA
A placebo-controlled, double-blinded prospective pilot study. Group 1: MTF.
Group 2: Placebo.Apply twice daily. 8 weeks Stereotactic scalp photographs and scalp biopsies, and microarray analysis. Group 1: MTF-induced hair growth in both the frontal and vertex scalp of patients. MTF treatment induced the expression of hair keratin-associated genes and decreased the expression of inflammatory genes and epidermal differentiation complex (EDC) in both scalp regions. MTF is effective in the treatment of both the frontal and vertex scalps of AGA patients. Small study size, short-term study, and lack of long-term follow-up. No adverse events were specified. 1Olsen et al. (2007) n=352 (M)
Group 1 : = 176
Group 2 : = 176AGA
Multicenter, randomized, placebo-controlled, double-blind clinical trial. Group 1: 5% MTF.
Group 2: placeboOne-half capful (1g) was applied directly to the affected vertex balding scalp twice daily 16 weeks Safety evaluations at weeks 1, 4, 8, 12, and 16; target area hair counts (TAHC), patient self-assessment, global photographic review, and safety evaluation Statistically significant increase in hair counts in the 5% MTF group compared to the placebo (p<0.0001), and subjective assessment of improved hair loss condition (p<0.0001). 5% MTF is a safe and effective treatment for men with AGA. No collection of efficacy data beyond 16 weeks. At week 16:
Group 1 – dryness/scaling (5%), folliculitis (2%), erythema (7%), burning (3%), itching (8%), stinging (4%).
Group 2 - dryness/scaling (7%), folliculitis (2%), erythema (8%), burning (2%), itching (2%), stinging (4%).
Minoxidil levels were within normal levels and consistent with PK study results.3Lucky et al (2004) N=381 (F)
Group 1: 153
Group 2: 154
Group 3: 74FPHL
A double-blind, placebo-controlled, randomized, multicenter trial. Group 1: 5% MXT.
Group 2: 2% MXT.
Group 3: vehicle for 5% solution.Applied twice daily. 48 weeks. Change in non-vellus TAHC (through macro photography), patient self-assessment of hair growth/scalp coverage, and investigator assessment of hair growth/scalp coverage. Hair Count at Week 48:
Group 1 -24.5 ± 21.9
Group 2 -20.7± 17.6
Group 3 -9.4±14.6
Scalp Coverage (0-100) patient:
Group 1 - 60 ±27.6
Group 2- 50.5 ±32.5
Group 3- 41.8 ±29.9
Scalp Coverage (0-100) investigator:
Group 1 -42 ±27.1
Group 2 -37.4 ±30.1
Group 3 -30.2 ±275% MXT was superior to placebo on each of the 3 primary efficacy endpoints. 2% MXT was superior to placebo for assessments of non-vellus hair counts. No limitations specified. Drug-related adverse events of a dermatologic nature (e.g., pruritus, dermatitis, hypertrichosis, scaling) were more prevalent in the 5% topical minoxidil group than in the 2% or placebo groups. 4Olsen et al (2002) N=393 (M)
Group 1: 157
Group 2: 158
Group 3: 78AGA
Double-blind, placebo-controlled, randomized, multicenter trial. Group 1: 5% MXT
Group 2: 2% MXT.
Group 3: placebo (vehicle for 5% solution).Applied twice daily. 48 weeks Hair counts from macro photographs of clipped hair, patient and investigator assessments of hair growth done by validated hair growth questionnaires. Hair Counts at Week 48:
Group 1: 18.6 ±25.4
Group 2: 12.7 ±20.7
Group 3: 3.9 ±21.7
Scalp Coverage (0-100) patient:
Group 1: 62 ±17
Group 2: 56.9 ±11
Group 3: 51 ±14.9
Scalp Coverage (0-100) investigator:
Group 1: 12.3 ±23.1
Group 2: 7 ±20.4
Group 3: 2.5 ±19.55% MXT was superior to 2% MXT and placebo at increasing hair regrowth in men. Men who used 5% MXT also had an earlier response to treatment than those who used 2% MXT. Not specified Group 1:
Pruritus and dermatitis (6 participants), local intolerance leading to withdrawal (5 participants), and headache (5 participants).
Group 2: Pruritus and dermatitis (2 participants), local intolerance (1 participant), headache (1 participant).
Group 3: Pruritus and dermatitis (2 participants), headache (1 participant).5Duvic et al (1996) N=22 (F)
Group 1: 11
Group 2: 9CIA
A randomized, double-blind pilot study. Group 1: 2% MXT
Group 2: placeboApplied twice daily. Throughout the course of chemotherapy and up to 4 months post-chemo treatment. Investigator and patient evaluation of a 2-inch diameter circle on the patient’s scalp. Baseline to maximal hair loss (days):
Group 1: 61.8 ±18.43
Group 2: 50.3 ±14.26
Baseline to maximal hair regrowth (days):
Group 1: 148.5 ±37.37
Group 2: 187.2 ±51.07
Period of baldness:
Group 1: 86.7 ±40.09
Group 2: 136.9 ±51.25
Baseline to first moderate or dense regrowth:
Group 1: 131.2 ±42.37
Group 2: 155.3 ±79.992% MXT appears to reduce the period of baldness from chemotherapy by more than a month in some patients. Small sample size, imbalance in each group. Group 1: Pruritus (4 participants), folliculitis (2 participants), facial hair growth (5 participants).
Group 2: Pruritus (8 participants), scalp folliculitis (3 participants), facial hair growth (3 participants).3Jacobs et al (1993) N=294 (F)
Group 1: 176
Group 2: 170FPHL
A double-blind, placebo-controlled trial Group 1: 2% MX
Group 2: placeboApplied twice daily 32 weeks Hair counts (photography with computer-assisted counting), investigator and patient assessments of visible new hair growth from global photographs. Hair Count: Mean increase in non-vellus hair count was 33 hairs for group 1 compared to 19 hairs for group 2.
Investigator Assessment:
44% of Group 1 achieved new hair growth compared to 29% of Group 2.
Patient Assessment:
55% of participants in Group 1 believed they achieved new hair growth compared to 41% in Group 2.Topical MX was more effective than the placebo in the treatment of FPHL. Not specified No clinically significant changes in vital signs were observed during the study, and no serious or unexpected medical events were recorded. 3Whiting and Jacobson (1992) N=33 (F)
Group 1: 17
Group 2: 16FPHL
A multicenter, randomized, double-blind, placebo-controlled trial. Group 1: 2% MXT
Group 2: placebo (vehicle only)Applied twice daily at 12-hour intervals. 32 weeks. Hair counts (macrophotography), investigator and patient subjective evaluations of hair shedding. Hair Counts: For Group 1, the mean no. of hairs increased by 16.8%, and for group 2, the mean no. of hairs increased by 12.7%.
Hair shedding: For group 1, 67% noted decreased shedding compared with 54% in the placebo.Patients with FPHL regrew a minimal to moderate amount of hair after 32 weeks of twice daily application of 2% minoxidil. Small sample size. No side effects were reported. 3 -
-
FREE RESOURCES
Research Tables
Want the latest research on Oral Minoxidil? Every quarter, our research team conducts a literature search on Oral Minoxidil to keep you up-to-date on new studies. See our search criteria & research tables below – including a summary of key findings from every single study.
Last updated: October 2024
Results
Search Criteria
Parameter
Inclusion Criteria
Exclusion Criteria
Patients Patients of any age with hair loss. Patients with no hair loss disorder. Intervention Oral minoxidil as a standalone or adjunct therapy. A study that doesn’t contain oral minoxidil either as a standalone or adjunct therapy. Comparator Placebo and/or other therapies or baseline, or in the observational studies - none. Outcomes Primary Endpoints of phototrichogram, investigator, and/or patient assessments. Any study not designed to adequately test for the standalone or additive effect of oral minoxidil. Study Design Prospective, observational, retrospective, and case series studies. Literature reviews, non-human subjects, or ongoing clinical trials. Search Terms
Search Terms:
oral hair loss alopecia minoxidil-
Abbreviations:
-
FPHLFemale pattern hair loss
-
AGAAndrogenetic alopecia
-
MXMinoxidil
-
pCIAPersistent chemotherapy-induced alopecia
-
EIAEndocrine therapy-induced alopecia
-
TETelogen effluvium
-
AUAlopecia universalies
-
SALTSeverity of Alopecia Scoring Tool
Summarized Studies
Study Participants Design Treatment Results Key Takeaway Adverse Effects Evidence Quality Authors (year) Sex Hair Loss Type Design Dose Usage Duration Endpoints Hair Growth Assessments Summary Limitations Adverse Effects Jadad Score Minta et al. (2023) n=24 (F)
Group 1: 13
Group 2: 11
pCIA
or
EIA
Retrospective Group 1: oral MX 2.25 mg/day
Group 2: 5% solution or foamOnce-daily 16 weeks Pre- and post-treatment standardized clinical photos (vertex, frontal, lateral, and occipital scalp) and degree of alopecia (Dean Scale). Pre-treatment Dean scores were similar between both groups: 1.7 in group 1 vs. 1.5 in group 2. No significant difference between the two groups post-treatment (p=0.9). There is no significant difference between oral and topical MX for patients with EIA. However, oral MX was superior for pCIA patients. Retrospective study design, small sample size, and absence of trichometric analysis. Group 1: Hypertrichosis (n=1), scalp irritation (n=2), headache (n=1) – led to discontinuation.
Group 2: Hypertrichosis (n=1) - led to discontinuation, orthostasis/hypotension (n=1).1Feaster et al (2022) n=210
Group 1: 105 (25 M, 80 F)
Group 2: 105 (25 M, 80 F)
AGA
and/or
TE
Multi-center, retrospective Group 1: 0.625-2.5 mg MX.
Group 2: Nothing, or other medications that are not minoxidil (unspecified).Once daily 52 weeks Clinical response (improvement, stabilization, worsening) based on provider assessment. Clinical photographic evaluation using a 3-point scale. Safety and tolerability 55 patients (of Group 1) (52.4%) demonstrated clinical improvement in hair growth,
44 patients (41.9%) demonstrated stabilization of hair loss, and 6 patients (5.7%) demonstrated worsening of their conditions.Oral MX is an effective treatment option for male and female AGA/TE. Adverse effects reported by patients were generally mild and did not result in discontinuation. Retrospective, no blinding, patients in both groups were also using other medications, no placebo-controlled group. Adverse effects in Group 1:
Edema - 1.9%
Shedding - 1%
Hypertrichosis - 4.8%
Lower extremity cramping - 1%
Palpitations - 1%
Burning scalp - 1%1Silva et al (2022) n= 26 (F)
Group 1: 14
Group 2: 12
FPHL
Randomized, double-blind trial. Group 1: 0.25 mg MX
Group 2: 1 mg oral MXOnce daily 24 weeks Change in total hair count from baseline to week 24 (photographic review of target area). Hair shedding scores on two scales (Sinclair and Martinez-Velasco). Quality of life was assessed using a questionnaire. Hair shaft count/cm2:
Group 1: (baseline 292±63.1
24 weeks 299.8±70.7) p=0.2.
Group 2: (baseline 277.2±46.6
24 weeks 304±39) p<0.001
Shedding: Both groups showed significant improvements in both shedding scales - however, there was no significant difference between treatments.
QoL: Scores improved significantly for both treatments.Both 0.25 mg/day and 1 mg/day oral MX were effective in reducing hair shedding and improving QoL in patients with FPHL. However, the 1 mg/day dose was superior to the 0.25 mg/day dose in terms of increasing hair shaft count in the target area. No significant adverse effects observed in either group. Single-center study, no placebo group, duration of the study was relatively short, small sample size. Group 2: Mild facial hypertrichosis (n=2), and temporary worsening of hair loss (n=1) at the 8-week visit, but this resolved by the 24-week visit.
No patients withdrew due to adverse effects.2Vahabi-Amlashi et al (2021) n=72 (F)
Group 1: 36
Group 2: 36
FPHL
Triple-blind, randomized clinical trial. Group 1: 0.25 mg MX and 1cc topical placebo solution.
Group 2: 1cc of 2% topical MXOral treatment - once daily.
Topical treatment - twice daily.36 weeks Shedding and Sinclair scores, recorded by 3 different evaluators, Trichoscopy to measure hair density and diameter, liver, kidney, and electrolyte tests. Side effects measured. Both groups showed significant increases in hair diameter and hair density over the treatment period.
Group 1: Improved 13% from baseline.
Group 2: Improved 6% from baseline.
Sinclair and shedding scores decreased significantly in both groups by the end of the study.
No significant differences were found between the two groups for any of the endpoints.Both treatments resulted in significant improvements in hair diameter, density and clinical indexes for women with FPHL. Oral MX showed slightly better recovery in hair density, and topical minoxidil showed slightly better recovery in hair diameter. Pilot study with a relatively small sample size, participants were predominantly in Sinclair stage II and III FPHL, which might limit the generalizability of the findings to more advanced cases. The study also did not address potential underlying causes of hair loss or include a placebo. Group 1: Hirsutism (7.7%), weight gain (3.8%). Gastrointestinal tolerance (7.7%) and hypotension (3.8%) - leading to study exclusion.
Group 2: Hirsutism (8%).2Kumar et al (2021) n=95 (M)
Group 1: 47
Group 2: 48
AGA
Pilot study Group 1: PRP + 1.25 mg MX
Group 2: PRP + 2.5 mgMX - Once daily
PRP - Every 4 weeks24 weeks (PRP treatment lasted 16 weeks) Photographic assessment, trichoscopic evaluation, and patient self-assessment. Photographic Assessement:
Group 1: marked improvement seen in 40% of participants.
Group 2: marked improvement seen in 58.3% of participants.
% increase in total hairs:
Group 1: 15.41%
Group 2: 22.15%
% increase in hair diameter:
Group 1: 25.14%
Group 2: 33.98%Low dose oral MX (1.25 or 2.5 mg) in combination with PRP can be used effectively in patients who are apprehensive of taking finasteride or dutasteride, and are less responsive to MX alone. Small sample size. Group 1: Peripheral edema (1/47), Hypertrichosis (36/47)
Group 1: Peripheral edema (1 - leading to withdrawal), urticaria (1 - leading to withdrawal) and hypertrichosis (39/48).
Mild pain noted in all patients during PRP.1Dincer et al (2021) n=1 (31-year-old male)
Treatment resistant
AU
Retrospective case study. Tofacitinib 10 mg/kg for 6 months. Then MX powder(concentration unknown) Once daily 24 weeks SALT scores were assessed by an expert investigator. SALT score was originally 100% and dropped to 35% after 24 weeks of minoxidil. A combination of tofacitinib and oral minoxidil may be an effective alternative treatment approach in severe AA cases. Single-case study, with unknown concentration of minoxidil used. None specified 0Panchaprateep and Lueangarun (2020) n=30
(M)
AGA
Open-label, prospective single-arm study. 5 mg Oral MX Once daily 24 weeks Hair counts, hair diameter, photographic assessment, and self-administered questionnaire. Hair Count - significant increase in total hair count compared to baseline (+35.1±18.9 hairs/cm2) P = 0.003
Hair Diameter - significant increase baseline by 15.21% at 24 weeks (p<0.001).
Global Photographic Assessment: 43% of patients achieved an excellent improvement score by the end of the study.Oral MX at 5 mg once daily significantly increased hair growth in men with AGA by 24 weeks of treatments. Open-label, small study, no placebo, and relatively short duration. Pedal edema was present in 3 patients at 1-2 months into treatment, which resolved after 2-3 months, of which 2 patients had obesity.
Hypertrichosis occurred in 93.3% of patients at 24 weeks.1Beach et al (2020) n=51
F:39
M:122
AGA
|
23
Multiple diagnoses
|
15
LPP or FFA
|
6
TA
|
3
CCCA
|
1
TE
|
1
CIA
|
1
Retrospective case series. 1.25 mg MX nightly Once daily 12 weeks Expert assessment at in-clinic visits. 65% of patients showed increased scalp hair growth. 27% of patients showed decreased hair shedding. Patients with nonscarring alopecia showed the most improvement. Patients generally continued therapy for an average of 10 months. Oral MX could lead to increased hair growth and decreased shedding in patients with alopecia, with many patients experiencing positive results. Retrospective, small sample size, lack of comparator, and multiple hair loss disorders. Hypertrichosis - 22
Urticaria - 1
Parasthesia - 1
Ankle edema - 1
Palpitation - 2
Hypotensive symptoms - 41Ramos et al (2020) n=52 (F)
Group 1: 26
Group 2: 26
FPHL
Randomized, open-label, comparative study. Group 1: 1 mg oral MX
Group 2: 5% topical MXOnce daily 24 weeks Total hair density), change in terminal hair density, global photographic evaluation (by 3 dermatologists), and Sinclair hair shedding score. Total hair density: Increased by 12% in Group 1and 7.2% in Group 2.
Global photograph:
Group 1: slightly impaired = 1, no change = 7, slightly improved = 16, and greatly improved = 2. Group 2: slightly impaired = 2, no change = 12, slightly improved = 11, and greatly improved = 1.
Hair Shedding: Group 1: reduced from 5 - 3.
Group 2: stayed the same (from 4 to 4).Oral MX showed superior performance to topical MX in the majority of outcomes. Oral MX can be considered an option for FPHL patients with poor compliance or who cannot tolerate topical minoxidil. Open-label, small sample size, lack of placebo group. Group 1: Edema of limbs =1, Hypertrichosis = 7.
Group 2: Hypertrichosis = 1.2Perera and Sinclair (2017) n=36 (F)
AGA
and/or
TE
Retrospective 0.25 - 2.5 mg oral MX Once daily 52 weeks Change in hair shedding scores (HSS). Patient improvement of trichodynia, changes in blood pressure, and adverse events. Mean baseline score = 5.64. After 6 months of treatment there was a reduction in mean HSS by 1.7 (p<0.001), and after12 months there was a reduction by 2.58 (p<0.001).
Five women with trichodynia at baseline noted improvement or resolution within 3 months.Once-daily oral MX appears to reduce hair shedding in Chronic TE. The treatment was generally well-tolerated, with mild adverse events. Retrospective, non-standardized dose, small study size. Postural dizziness that resolved with continued treatment = 2
Ankle edema = 1
Facial hypertrichosis = 131 -
- Mission Statement
 Scroll Down
Scroll Down