Publications
A tenet of Perfect Hair Health is to involve ourselves in hair loss research. This is why we regularly publish peer-reviewed papers, and then make them freely accessible for anyone with an internet connection. You can read our manuscripts below.
Microneedling and Its Use in Hair Loss Disorders:
A Systematic Review
English, R.S., Ruiz, S. & DoAmaral, P. Microneedling and Its Use in Hair Loss Disorders: A Systematic Review. Dermatol Ther (Heidelb) (2021). https://doi.org/10.1007/s13555-021-00653-2
Introduction: Microneedling (MN) is a minimally invasive procedure involving the induction of percutaneous wounds with medical-grade needles. In this literature review, we investigate clinical data on MN for the treatment of hair loss disorders.
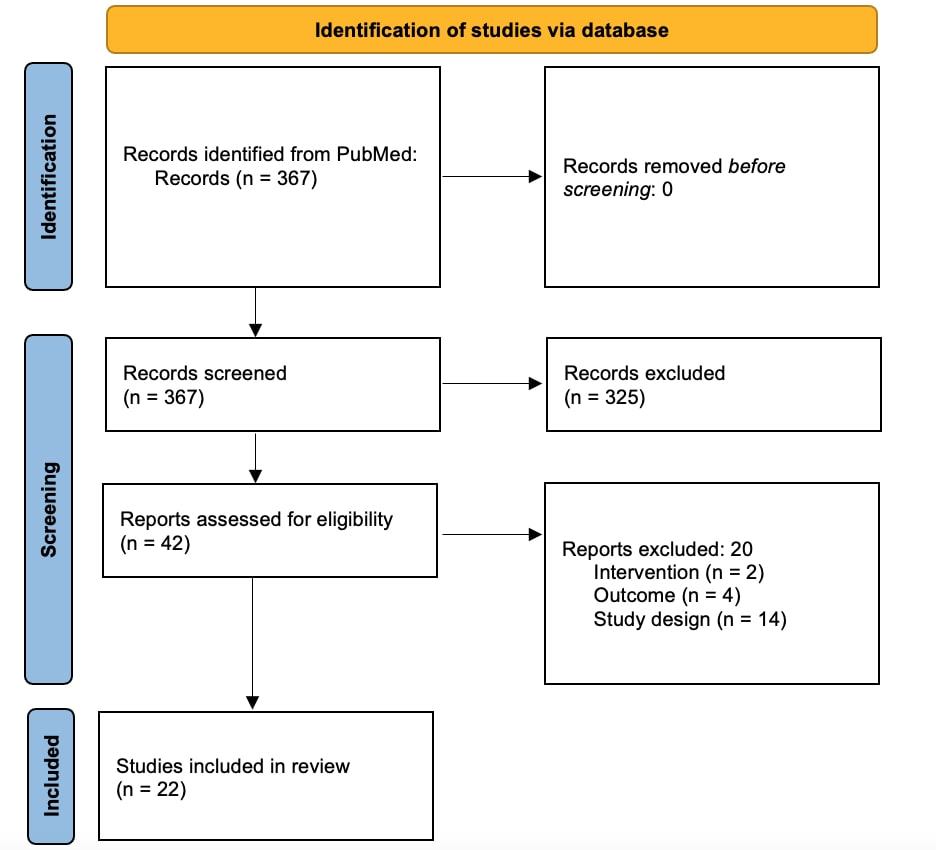
Methods: A literature search was conducted through PubMed up to November 2021 to identify original articles evaluating the use of MN on hair loss disorders. The database was searched using the following keywords: “microneedling,” “micro needling,” “micro needle,” “microneedle,” “needle,” “dermaroller” and “alopecia,” “hair loss,” “alopecia,” “areata,” “cicatricial,” or “effluvium,”
Results: A total of 22 clinical studies featuring 1127 subjects met our criteria for inclusion. Jadad scores ranged from 1 to 3, with a mean of 2. As an adjunct therapy, MN improved hair parameters across genders and a range of hair loss types, severities, needling devices, needling depths of 0.50–2.50 mm, and session frequencies from once weekly to monthly. Across 17 investigations totaling 911 androgenic alopecia (AGA) subjects, MN improved hair parameters when paired with 5% minoxidil, growth factor solutions, and/or platelet-rich plasma (PRP) topicals, or when introduced to subjects whose hair count changes had plateaued for ≥ 6 months on other treatments. Across four investigations on 201 alopecia areata (AA) subjects, MN improved hair parameters as a standalone therapy versus cryotherapy, as an adjunct to 5-aminolevulinic acid and photodynamic therapy, and equivalently when paired with topical PRP versus carbon dioxide laser therapy with topical PRP. Across 657 subjects receiving MN, no serious adverse events were reported.
Conclusions: Clinical studies demonstrate generally favorable results for MN as an adjunct therapy for AGA and AA. However, data are of relatively low quality. Significant heterogeneity exists across interventions, comparators, and MN procedures. Large-scale randomized controlled trials are recommended to discern the effects of MN as a standalone and adjunct therapy, determine best practices, and establish long-term safety.
Use of Botulinum Toxin for Androgenic Alopecia:
A Systematic Review
English Jr. R, S, Ruiz S. Skin Appendage Disord. 2021; doi: 10.1159/000518574
Abstract: In this systematic review, we summarize the efficacy and safety of intradermal and intramuscular botulinum toxin injections for androgenic alopecia (AGA). Using PubMed, we conducted a literature search up to February 2021 using the following keyword combinations: “botulinum toxin” or “botox” and “androgenetic alopecia,” “hair loss,” or “alopecia.” Five clinical studies met our inclusion criteria: 4 prospective cohorts and 1 randomized clinical trial (RCT). Study durations ranged from 24 to 60 weeks. No studies included control groups or compared botulinum toxin injections against approved treatments. A total of 165 participants were identified – all of whom were males with AGA. Of the 4 studies measuring response rates (i.e., subjects with >0% hair changes), response rates ranged from 75 to 79.1%. Within studies measuring hair count changes from intramuscular injections, changes ranged from 18 to 20.9%. No serious adverse events were reported. Studies on botulinum toxin injections have produced favorable outcomes for AGA subjects. However, results should be interpreted with caution due to the absence of control groups, small numbers of participants, and relatively low Jadad quality scores. Large RCTs are recommended to confirm efficacy and safety, explore the effects of botulinum toxin on females with pattern hair loss, and establish best practices for intradermal and intramuscular injection methodologies.
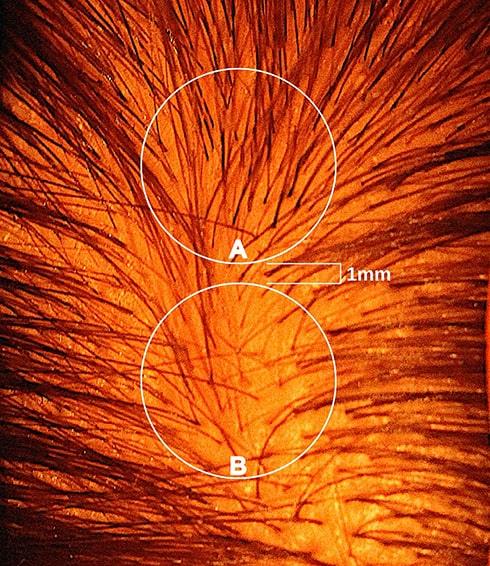
Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia: Are Biopsy Location, Hair Diameter Diversity, & Relative Hair Follicle Miniaturization to Blame?
English Jnr R, Ruiz S. Clin Cosmet Investig Dermatol. 2021;14:357-365 https://doi.org/10.2147/CCID.S306157
Abstract: Despite decades of study, debate persists over the role of inflammation, fibrosis, and prostaglandins in the histopathology of androgenic alopecia (AGA). This brief review proposes that inconsistent findings across histological studies are a consequence of three inadequately controlled variables: 1) biopsy location, 2) hair diameter diversity (HDD), and 3) relative hair follicle miniaturization (HFM) within and across subjects. We suggest new methodological considerations to improve AGA histopathological research, as well as a novel classification system to quantify HFM by its stages. Finally, we hypothesize a dynamic relationship between inflammation, fibrosis, and prostaglandin activity dependent on relative HFM.
Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
English, R.S. & Barazesh, J.M. Dermatol Ther (Heidelb) (2019) 9: 167. https://doi.org/10.1007/s13555-019-0281-6
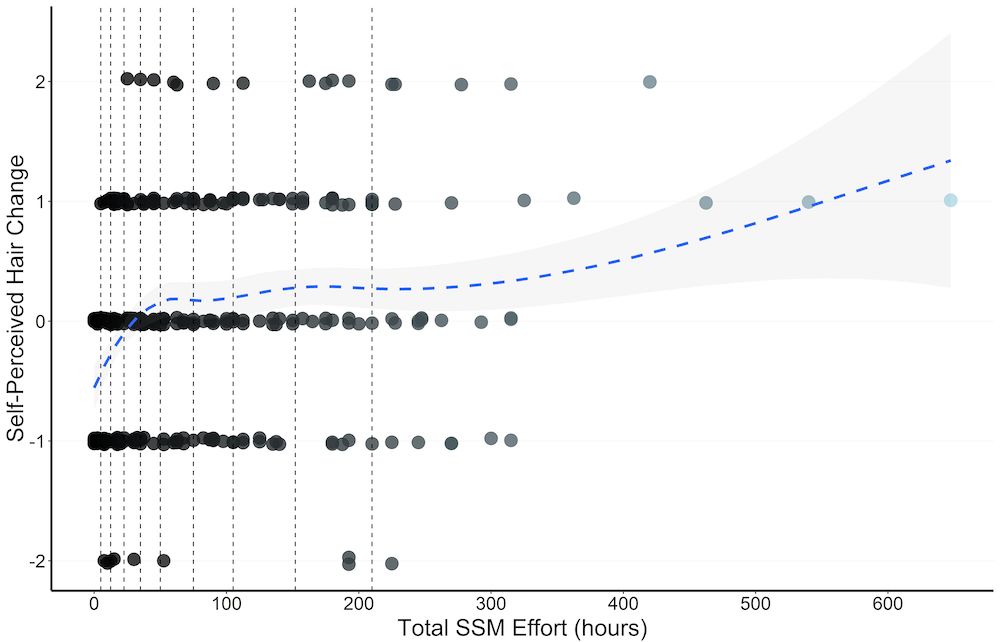
Introduction: Standardized scalp massages (SSMs) improve hair thickness in nonbalding men, but their effects on androgenic alopecia (AGA) have not yet been evaluated. The objective of this study was to investigate the effect of SSMs on self-assessed AGA sufferers (SAGASs).
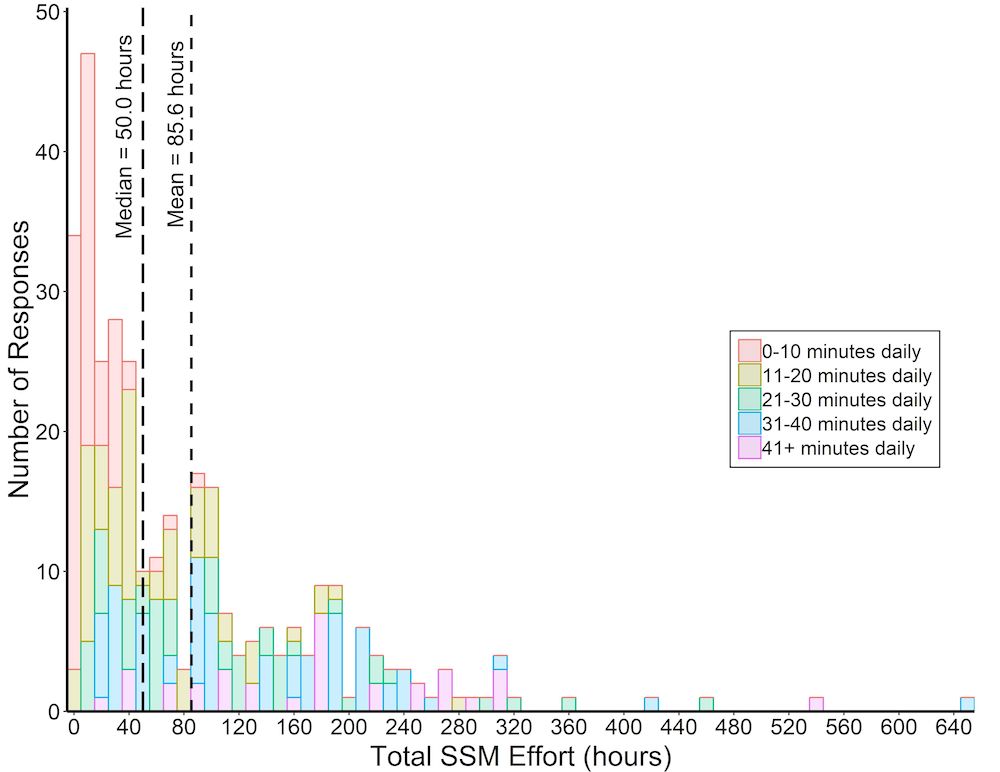
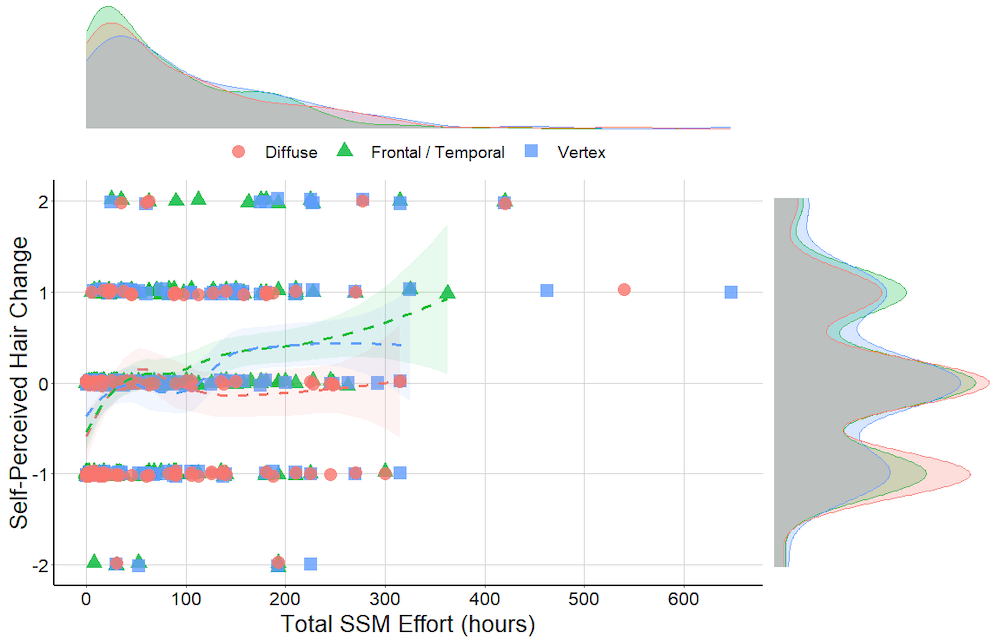
Methods: Between October 2016 and October 2017, 1899 SAGASs searching online for hair loss treatments beyond AGA management drugs accessed literature explaining SSMs as a potential therapy for AGA, then watched a demonstration video detailing twice-daily, 20-min SSMs segmented by three rotational scalp regions using hand-generated presses, pinches, and stretches. In December 2017, SAGASs were contacted once to participate in a retrospective survey study to assess SSM adherence and hair changes. Age, gender, hair loss region and gradient, diet, supplement and topical use, AGA management drug use, estimations for minutes daily and months of massaging, and self-perceived hair changes were reported. Some participants also submitted photosets documenting hair changes throughout SSM adherence.
Results: A total of 340 (17.9%) respondents completed the survey, and 327 (17.2%) reported attempting the SSMs. SSM participants reported a median daily massage effort of 11–20 min and mean adherence of 7.4 ± 6.6 months, with 68.9% reporting hair loss stabilization or regrowth. Estimated minutes daily, months, and total SSM effort (i.e., minutes daily × months) were positively associated with self-perceived hair changes. On average, perceived hair loss stabilization and regrowth occurred after 36.3 h of SSM effort. Results did not vary across age, gender, Norwood gradient, or concomitant supplement, topical, finasteride, minoxidil, or microneedling use. However, hair change improvements were marginally lower for participants reporting diffuse versus frontal/temporal or vertex thinning.
Conclusions: While further research is warranted, these results align with previous findings and suggest the potential for SSMs to improve AGA.
A hypothetical pathogenesis model for androgenic alopecia: clarifying the dihydrotestosterone paradox and rate-limiting recovery factors
English RS Jr. A hypothetical pathogenesis model for androgenic alopecia: clarifying the dihydrotestosterone paradox and rate-limiting recovery factors. Med Hypotheses. 2018;111:73–81.
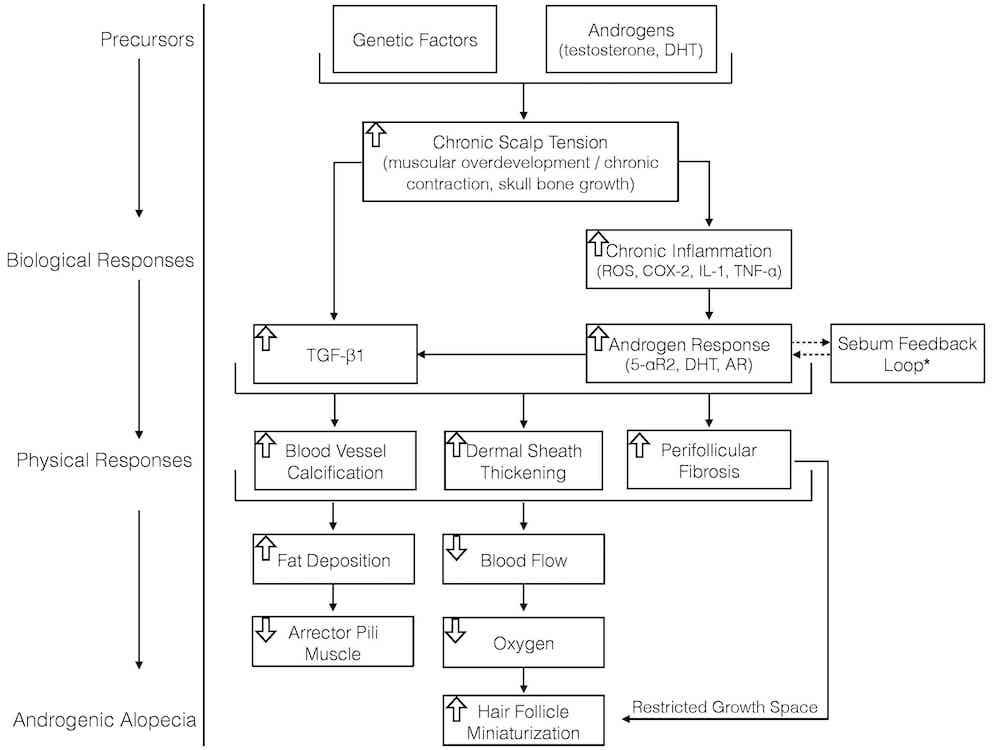
Abstract: Androgenic alopecia, also known as pattern hair loss, is a chronic progressive condition that affects 80% of men and 50% of women throughout a lifetime. But despite its prevalence and extensive study, a coherent pathology model describing androgenic alopecia’s precursors, biological step-processes, and physiological responses does not yet exist. While consensus is that androgenic alopecia is genetic and androgen-mediated by dihydrotestosterone, questions remain regarding dihydrotestosterone’s exact role in androgenic alopecia onset. What causes dihydrotestosterone to increase in androgenic alopecia-prone tissues? By which mechanisms does dihydrotestosterone miniaturize androgenic alopecia-prone hair follicles? Why is dihydrotestosterone also associated with hair growth in secondary body and facial hair? Why does castration (which decreases androgen production by 95%) stop pattern hair loss, but not fully reverse it? Is there a relationship between dihydrotestosterone and tissue remodeling observed alongside androgenic alopecia onset?
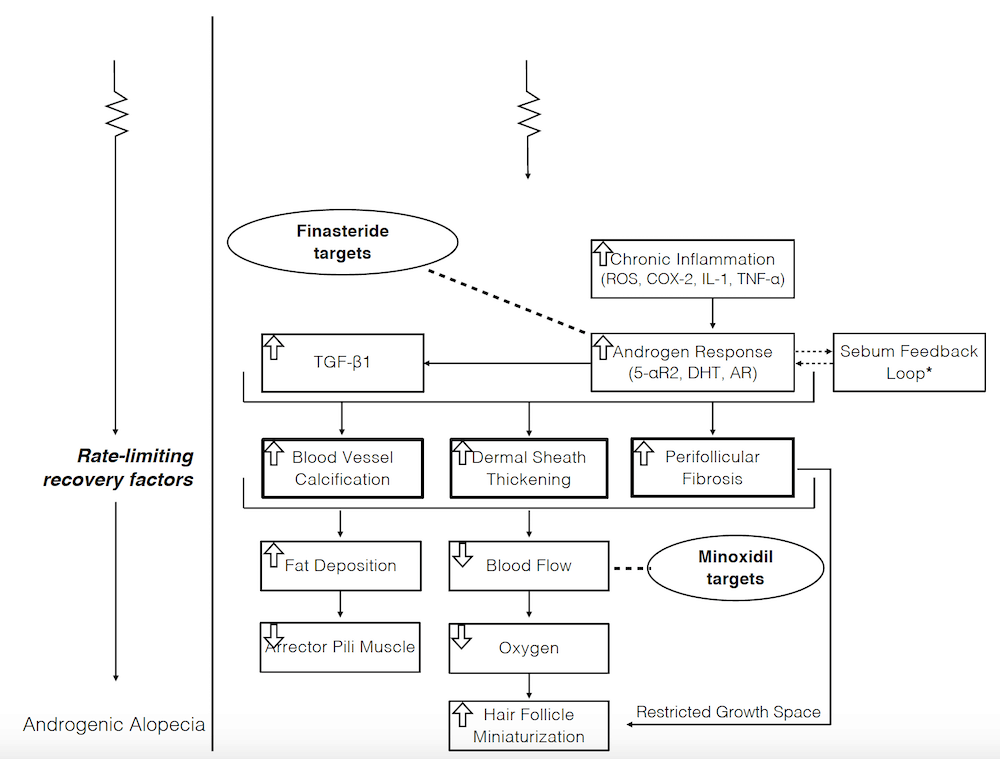
We review evidence supporting and challenging dihydrotestosterone’s causal relationship with androgenic alopecia, then propose an evidence-based pathogenesis model that attempts to answer the above questions, account for additionally-suspected androgenic alopecia mediators, identify rate-limiting recovery factors, and elucidate better treatment targets. The hypothesis argues that: (1) chronic scalp tension transmitted from the galea aponeurotica induces an inflammatory response in androgenic alopecia-prone tissues; (2) dihydrotestosterone increases in androgenic alopecia-prone tissues as part of this inflammatory response; and (3) dihydrotestosterone does not directly miniaturize hair follicles. Rather, dihydrotestosterone is a co-mediator of tissue dermal sheath thickening, perifollicular fibrosis, and calcification – three chronic, progressive conditions concomitant with androgenic alopecia progression. These conditions remodel androgenic alopecia-prone tissues – restricting follicle growth space, oxygen, and nutrient supply – leading to the slow, persistent hair follicle miniaturization characterized in androgenic alopecia.
If true, this hypothetical model explains the mechanisms by which dihydrotestosterone miniaturizes androgenic alopecia-prone hair follicles, describes a rationale for androgenic alopecia progression and patterning, makes sense of dihydrotestosterone’s paradoxical role in hair loss and hair growth, and identifies targets to further improve androgenic alopecia recovery rates: fibrosis, calcification, and chronic scalp tension.