- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
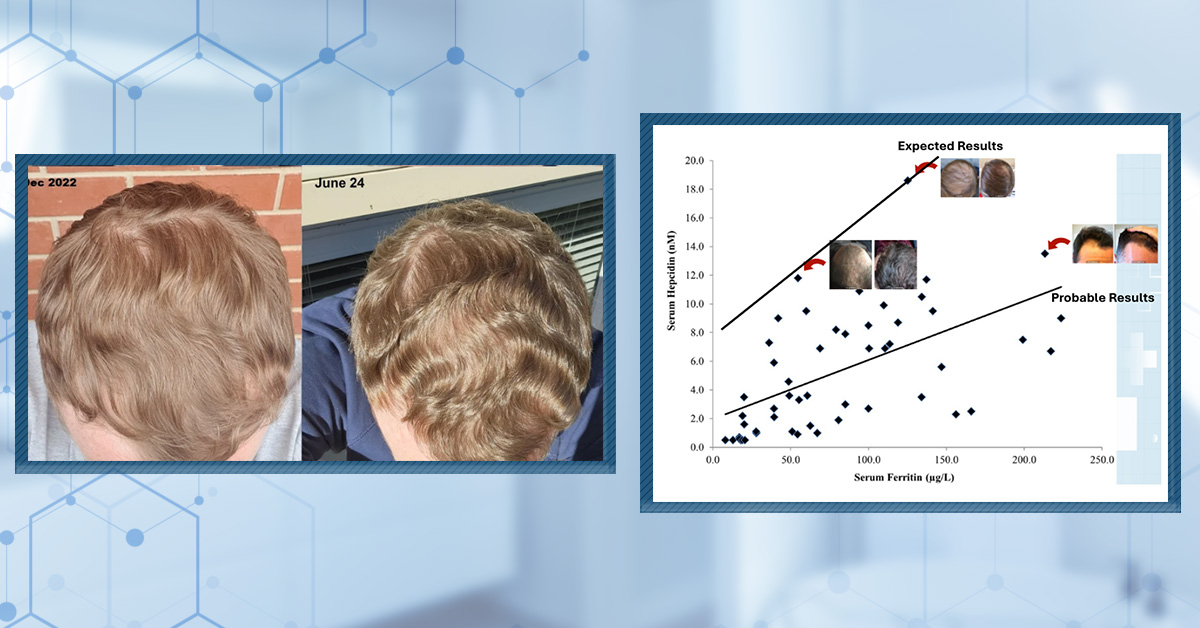
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
Scroll Down
Popular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
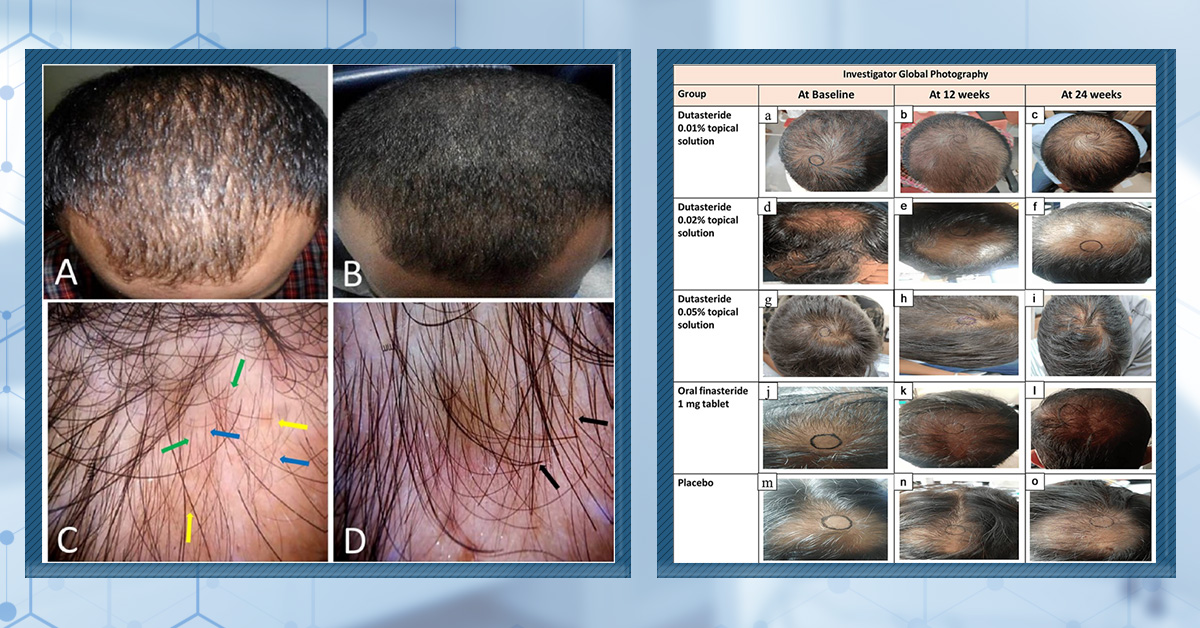
- Dutasteride
- Oral
- Topical
- Mesotherapy
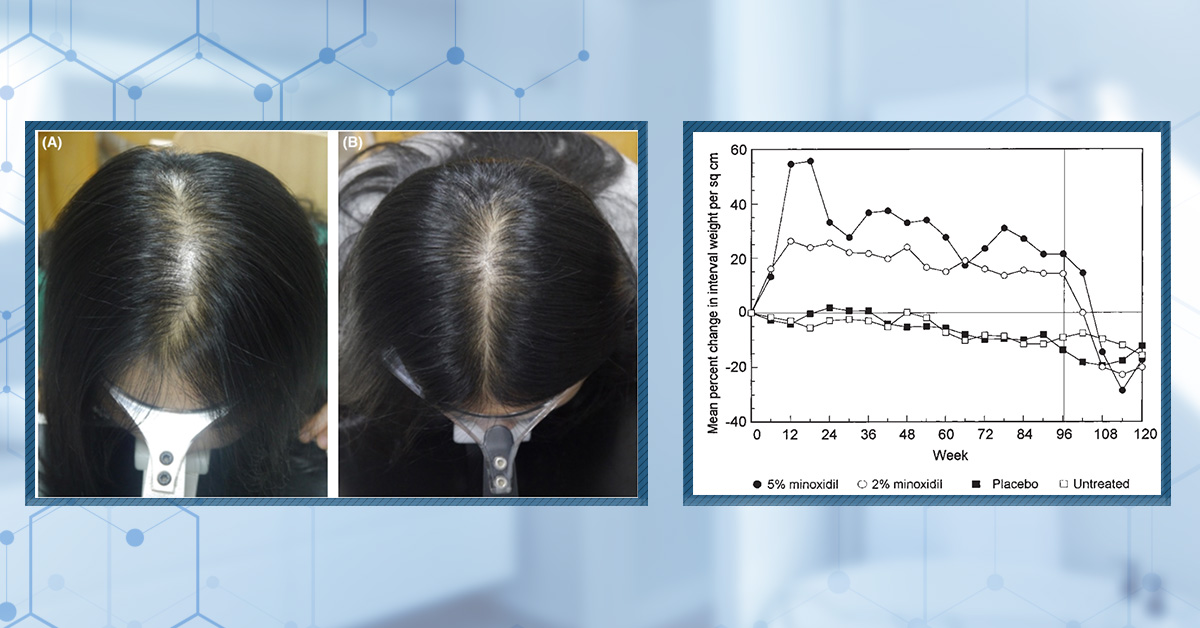
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
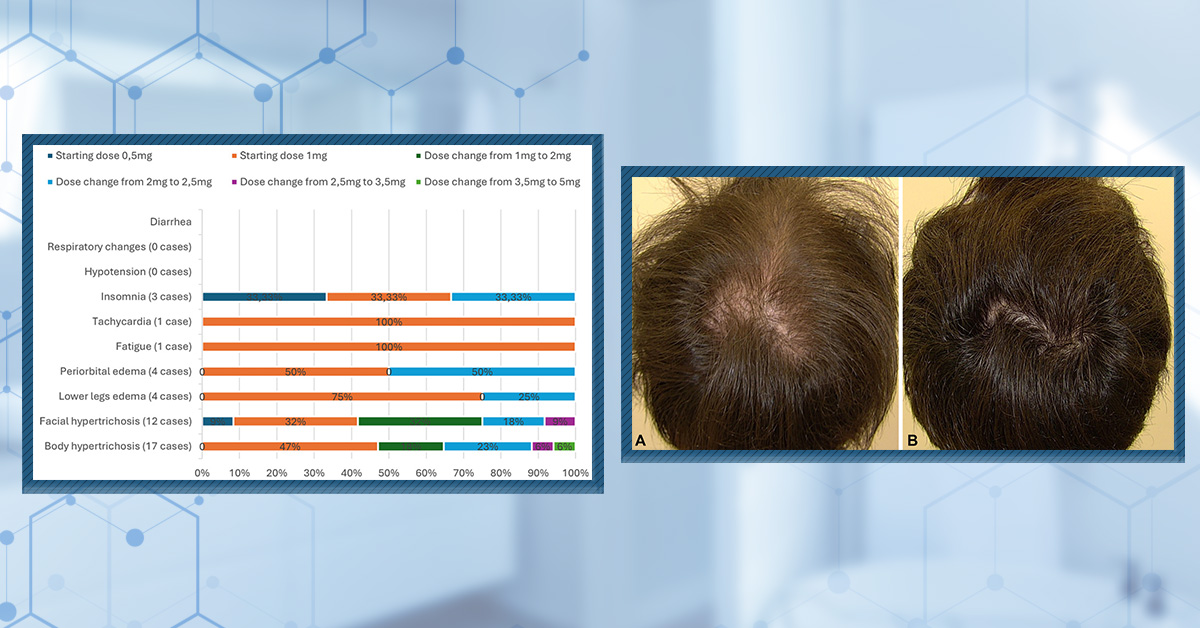
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Free CalculatorTopical Finasteride Calculator
- Free Interactive GuideInteractive Guide: What Causes Hair Loss?
- Free ResourceFree Guide: Standardized Scalp Massages
- Free Course7-Day Hair Loss Email Course
- Free DatabaseIngredients Database
- Free Interactive GuideInteractive Guide: Hair Loss Disorders
- Free DatabaseTreatment Guides
- Free Lab TestsProduct Lab Tests: Purity & Potency
- Free Video & Write-upEvidence Quality Masterclass
- Free Interactive GuideDermatology Appointment Guide
More
Articles100+ free articles.
-
Hims Hair Growth Reviews: The Pros, Cons, and Real Results
-
Topical Finasteride Before and After: Real Case Studies
-
How to Reduce the Risk of Finasteride Side Effects
-
10 Best DHT-Blocking Shampoos
-
Best Minoxidil for Men: Top Picks for 2026
-
7 Best Oils for Hair Growth
-
Switching From Finasteride to Dutasteride
-
Best Minoxidil for Women: Top 6 Brands of 2026
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
Before-Afters- Transformation Photos
Our library of before-after photos.
- Client Testimonials
Read the experiences of members
Before-Afters/ Client Testimonials- Popular Treatments
-
Articles
Progesterone is a steroid hormone with a wide range of physiological and medical effects. It is linked to female fertility and pregnancy, and it plays roles in neuro- and immunoprotection and various gynecological treatments. Studies have linked changes in progesterone levels to androgenic alopecia and postpartum telogen effluvium. Still, mixed evidence, limited research, and potential side effects have led to this treatment not being widely adopted.
In this article, we will explore the association between progesterone and hair loss, particularly female pattern hair loss (FPHL), and determine whether supplementation with progesterone can improve hair loss outcomes.
Key Takeaways
- What Is It? Progesterone is a steroid hormone that is essential for a wide range of physiological processes. Deficiencies are associated with menstrual irregularities, fertility and pregnancy issues, mood and sleep disturbance, and physical symptoms. Other signs can include dry skin and thinning hair.
- Evidence Quality: The evidence quality is 31/100 based on our metrics.
- Clinical Data: There is very limited evidence supporting using progesterone to improve hair loss outcomes.
- Study 1: 10 male patients with AGA were treated with a lotion containing 11a-hydroxyprogesterone. Improvements were observed in the “cranial” region of the scalp but not the left temporal region.
- Study 2: 6 male patients with AGA were treated with 100 mg of progesterone for 6 months. Improvements were observed in new hair growth and the transition from vellus to terminal hairs.
- Dosing & Formulation Considerations: Know your progestins! Many synthetic progesterone formulations are actually androgenic in nature rather than anti-androgenic. While some have more recently been developed to behave more closely to natural progesterone, there is data lacking in their efficacy to improve hair regrowth. We recommend sticking with natural progesterone until further research is available. If you are using natural progesterone, micronized allows for better systemic absorption especially when taken orally. It is typically prescribed at 200 mg daily for 12 days per 28-day cycle. However, it has not been tested for hair loss. If you decide to use non-micronized progesterone, a topical formulation may be more beneficial as oral is heavily metabolized and, therefore, may not reach the strength needed to affect hair growth outcomes. If you decide to take synthetic progestins, you might find results with cyproterone acetate or drospirenone (Slynd); however, once again, data is limited.
All-Natural Hair Supplement + Topical
The top natural ingredients for hair growth, all in one serum & supplement.
Take the next step in your hair growth journey with a world-class natural serum & supplement. Ingredients, doses, & concentrations built by science.

What Is Progesterone?
Progesterone is an important steroid hormone that plays several key roles in the female reproductive system. It is primarily produced by the corpus luteum in the ovaries after ovulation in women. For men, progesterone is produced in smaller amounts by the adrenal glands and is associated with sperm development.[1]Nio-Kobayashi, J., Miyazaki, K., Hashiba, K., Okuda, K., Iwanaga, T. (2016). Histological analysis of arteriovenous anastomosis-like vessels established in the corpus luteum of cows during … Continue reading,[2]Mirihagelle, S., Hughes, J.R., Miller, D.J. (2022). Progesterone-induced sperm release from the oviduct sperm reservoir. Cells. 11(10). 1622. Available at: https://doi.org/10.3390/cells11101622
Figure 1. Progesterone molecule.
The association between progesterone and hair health is multifaceted, involving direct hormonal effects and indirect influences.
Studies have shown that progesterone, due to its 5-alpha-reductase (5-AR) inhibiting properties, can help balance the potentially negative effects of androgens like testosterone. When progesterone levels decline, increased conversion of testosterone to dihydrotestosterone by 5-AR can occur, leading to hair follicle miniaturization and hair thinning.[3]Grymowicz, M., Rudnicka, E., Podfigurna, A., Napierała, P., Smolarczyk, R., Smolarczyk, K., Męczekalski, B. (2020). Hormonal effects on hair follicles. International Journal of Molecular Sciences. … Continue reading
Significant hormonal changes occur in menopausal women, including a decrease in estrogen and progesterone levels. Estrogen prolongs the growing (anagen) phase of the hair follicle cycle, and progesterone indirectly supports this through its androgen-inhibiting activity. Therefore, a reduction in both estrogen and progesterone can leave menopausal women vulnerable to increased androgen levels and subsequent hair loss.
Changes in progesterone levels can also affect postpartum women. During pregnancy, progesterone levels are significantly elevated but drop sharply after childbirth. This sudden decrease in progesterone and estrogen is believed to contribute to postpartum telogen effluvium (PPTE). However, unlike the other examples mentioned above, PPTE is generally self-limiting. It occurs 2-4 months after delivery and resolves typically within 6-24 weeks (although in rare cases, it can persist up to 15 months).[4]Cleveland Clinic. (no date). Postpartum Hair Loss. Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/23297-postpartum-hair-loss (Accessed: September 2024)
So, we know how progesterone deficits might lead to hair loss, but does progesterone supplementation improve hair loss outcomes?
Can Progesterone Improve Hair Loss Outcomes?
As previously mentioned, progesterone has some 5-AR inhibitory properties. However, there is limited evidence to show that it can improve hair loss outcomes.
One 1987 study treated ten male patients with AGA with a lotion containing 1% 11a-hydroxyprogesterone (a progesterone derivative) for one year, and 8 patients were treated with a control.[5]Van der Willigen, A.H., Peereboom-Wynia, J.D.R., van Joost, TH., Stolz, E. (1987). A preliminary study of the effect of 11a hydroxyprogesterone on hair growth in men suffering from androgenetic … Continue reading Those treated with the progesterone derivative showed an increase in the number of anagen hairs (45 to 51) and mean hair shaft diameter (69.6 μm to 71.6 μm) in the “cranial” region of the scalp. Further improvements were seen with reduced regressing/non-growing (catagen/telogen) hairs (46-40). Unfortunately, without images, we can’t see if these improvements led to a clinically significant outcome.
Furthermore, the study also analyzed hair counts on the left temporal side of the scalp. Here, the number of anagen hairs reduced from 67 to 62, and the number of catagen/telogen hairs increased from 21 to 30, indicating a varied response to the treatment.
Figure 2: Hair counts after topical application of a progesterone derivative.[6]Van der Willigen, A.H., Peereboom-Wynia, J.D.R., van Joost, TH., Stolz, E. (1987). A preliminary study of the effect of 11a hydroxyprogesterone on hair growth in men suffering from androgenetic … Continue reading
Another small study was conducted with 6 males with AGA, acne, and benign prostatic hyperplasia (BPH).[7]Kalinchenko, S., Nikiforov, I., Samburskaya, O. (2022). BPH, Androgenic Alopecia, and Acne – Markers of Progesterone Deficiency. Journal of the Endocrine Society. 6. 431-432. Available at: … Continue reading The participants were treated with Vitamin D and 100 mg progesterone daily for 6 months. After this period, the authors reported that the patients had reduced hair loss, new hair growth, and increased vellus transition to terminal hairs. Unfortunately, the authors didn’t report the specific values or show any photos. Furthermore, it is not possible to know if the positive effects were due to supplementing with Vitamin D.
While there is a logical reasoning behind the use of progesterone for women undergoing menopause suffering from female pattern hair loss, there is no clinical evidence demonstrating its efficacy.
Progesterone Formulations
There are a number of formulations of progesterone, but how effective might they be at improving hair loss outcomes?
Oral
Oral progesterone is typically prescribed for hormone replacement therapy (HRT). However, due to its metabolism, oral progesterone may only have limited benefits for hair loss. It undergoes extensive first-pass metabolism in the liver, leading to significant degradation of the hormone before it reaches the systemic circulation, meaning that limited amounts of the hormone may reach the scalp.[8]Coombes, Z., Plant, K., Freire, C., Basit, A.W., Butler, P., Conlan, R.S., Gonzalez, D. (2021). Progesterone metabolism by human and rat hepatic and intestinal tissue. Pharmaceutics. 13(10). 1707. … Continue reading
Topical
Topical progesterone has a few potential benefits, including:
- Localized application
- Fewer systemic side effects
- Bypass first pass metabolism, so more is reaching the target area
According to one source, the most common strength of progesterone applied topically is around 2%. However, this appears to be based on clinical experience rather than published studies.[9]Roseway Labs. (2020). Topicals for Hair Loss. Roseway Labs. Available at: https://rosewaylabs.com/topicals-for-hair-loss/ (Accessed: September 2024)
Injection
While some clinics use injected progesterone combined with other treatments, like platelet-rich plasma (you can find videos of these if you search on YouTube) to treat hair thinning, there is no peer-reviewed, published clinical evidence to suggest that it improves hair loss outcomes.
Micronized
Recently, there has been interest in using micronized progesterone and its potential as a hair growth treatment. This formulation may offer improved absorption and efficacy in balancing hormone levels, potentially aiding hair growth.
Micronized progesterone is a formulation of progesterone that has been processed to create very small particles smaller than 10 μm in size. This process increases the surface area of progesterone particles, allowing for better systemic absorption, especially when taken orally.[10]Hargrove, J.T., Maxson, W.S., Wentz, A.C. (1989). Absorption of oral progesterone is influenced by vehicle and particle size. American Journal of Obstetrics and Gynecology. 161(4). 948-951. Available … Continue reading
Micronized progesterone is chemically identical to the progesterone that is naturally produced in the human body, meaning it should work similarly.[11]de Lignieres, B. (1999). Oral micronized progesterone. Clinical Therapeutics. 21(1). 41-60. Available at: https://doi.org/10.1016/S0149-2917(00)88267-3 It is currently used as an HRT for menopausal symptoms, to support pregnancy and fertility, and to treat gynecological disorders.[12]Memi, E., Pavli, P., Papagianni, M., Vrachnis, N., Mastorakos, G. (2024). Diagnostic and therapeutic use of oral micronized progesterone in endocrinology. Reviews in endocrine and metabolic … Continue reading
While we have recently been getting a lot of emails from members about micronized progesterone, there is a significant gap in the literature about its potential efficacy in treating hair loss in menopausal women or people with AGA.
Synthetic Progesterone
We have discussed natural progesterone in-depth, so let’s also examine synthetic progesterone (progestins) and how it differs from natural progesterone.
Progestins differ from natural progesterone in their chemical structure, which results in different physiological effects. Some common synthetic progestins include norethindrone, medroxyprogesterone acetate (MPA), norethisterone (NET-A), and levonorgestrel. Unlike natural progesterone, many synthetic progestins can increase androgen activity. This is critical to keep in mind when choosing whether to take progestins if you suffer from hair loss. Furthermore, progestins can cause other unwanted side effects like acne, excessive hair growth in unwanted areas, and changes in skin texture, alongside more serious increased risks such as cardiovascular events (heart attacks and strokes) and cancers.
One study published in 2017 examined the androgenic and estrogenic properties of various progestins, including MPA and NET-A. The findings indicated that these progestins bind to the androgen receptor (AR) with affinities comparable to dihydrotestosterone (DHT), suggesting that they can exert androgenic effects in vivo (in cells).[13]Louw-du Toit, R., Perkins, M.S., Hapgood, J.P., Africander, D. (2017). Comparing the androgenic and estrogenic properties of progestins used in contraception and hormone therapy. Biochemical and … Continue reading
Research on hormonal contraceptives highlighted that synthetic progestins can lead to hair loss. One review conducted on data on alopecia associated with the levonorgestrel IUD found a number of women who had the IUD implanted between 2000-2001 experienced hair loss. Furthermore, in some of these cases, when the IUD was removed, women recovered their hair loss, indicating a direct effect of levonorgestrel on hair loss for some people. Unfortunately, this study is limited in many ways, including being a retrospective study and only having 73 total reports of alopecia (in New Zealand and using World Health Organization data).[14]Paterson, H., Clifton, J., Miller, D., Ashton, J., Harrison-Woolrych, M. (2007(. Hair loss with use of the levonorgestrel intrauterine device. Contraception 76. 306-309. Available at: … Continue reading
A case study from 2002, this time conducted on a woman taking a combination low-dose oral contraceptive (norethindrone and ethinyl estradiol), found shortly after starting, she experienced hair loss, which abated when stopped.[15]Yokoyama, Y., Sato, S., Saito, Y. (2002). Alopecia related to low-dose oral contraceptives. Archives of Gynecology and Obstetrics. 47. 266-246. Available at: https://doi.org/10.1007/pl00007489
So, it seems like if you have AGA, you might want to avoid synthetic progestins. But are there exceptions to the rule? There might be.
Cyproterone Acetate
While cyproterone acetate is a progestin, it has shown potential in improving hair regrowth in women with androgenic alopecia. In a study involving 80 women with FPHL treated with either 200 mg spironolactone, 50 mg of cyproterone acetate, or 100 mg daily for 10 days per month if menopausal, 44% of those treated with cyproterone acetate experienced hair regrowth. However, another 44% saw no change, and 12% continued to lose hair. There was also no significant difference between the cyproterone acetate and spironolactone groups.[16]Sinclair, R., Wewerinke, M., Jolley, D. (2005). Treatment of female pattern hair loss with oral antiandrogens. British Journal of Dermatology. 152(3). 466-473. Available at: … Continue reading
Another study reported that 77.1% of 35 women with androgenic alopecia observed hair regrowth after three months of treatment with the combined cyproterone acetate and ethinyl estradiol pill (2mg). 42.8% of participants had slight regrowth, 34.3% had moderate regrowth after trichoscopic assessment, and 22.8% showed no regrowth at all.[17]Coneac, A., Muresan, A., Orasan, M.S. (2014). Antiandrogenic therapy with ciproterone acetate in female patients who suffer from both androgenic alopecia and acne vulgaris. Clujul Medical. 87(4). … Continue reading
Figure 3. Effect of cyproterone acetate on hair regrowth. [18]Coneac, A., Muresan, A., Orasan, M.S. (2014). Antiandrogenic therapy with ciproterone acetate in female patients who suffer from both androgenic alopecia and acne vulgaris. Clujul Medical. 87(4). … Continue reading
A 12-month randomized trial found that cyproterone acetate was more effective than minoxidil at treating hair loss in women with signs of hyperandrogenism, which may be worth considering when considering hair loss treatments.[19]Vexiau, P., Chaspoux, C., Boudou, P., Fiet, J., Jouanique, C., Hardy, N., Reygagne, P. (2002). Effects of minoxidil 2% vs. cyproterone acetate treatment on female androgenetic alopecia: a controlled, … Continue reading
Drospirenone
Drospirenone (also known under the brand name Slynd) is a newer synthetic progesterone that has a unique profile. It is derived from spironolactone, a drug you may be familiar with, as it also has anti-androgenic properties. Like cyproterone acetate, Slynd does not increase androgenic activity. Instead, it has androgenic properties similar to natural progesterone, which makes it an attractive potential treatment.[20]Regidor, P.A., Mueller, A., Mayr, M. (2023). Pharmacological and metabolic effects of drospirenone as a progestin-only pill compared to combined formulations with estrogen. Womens Health (Lond). 19. … Continue reading
However, the data on hair loss is limited. One study evaluated the efficacy of oral finasteride therapy combined with an oral contraceptive containing drosperinone and ethinyl estradiol in premenopausal women with FPHL. The study found that 62% of patients showed some improvement in hair loss, but it was unclear whether the improvement was due to the higher dosage of finasteride or the combination with the oral contraceptive.[21]Iorizzo, M., Vincenzi, C., Voudouris, S., Piraccini, B.M., Tosti, A. (2006). Finasteride treatment of female pattern hair loss. Archives of Dermatology. 142(3). 298-302. Available at: … Continue reading
Furthermore, if you are sensitive or respond poorly to spironolactone, you might also experience side effects with Slynd. Another factor is that as a synthetic progestin, it might also carry elevated cardiovascular and cancer risks.
Other “new” progestins have also been developed and designed to be closer in mechanism of action to progesterone than other synthetics. These are dienogest, nestorone, nomegestrol acetate, and trimegestone, which have anti-androgenic activity, that may benefit those with hair loss, but again, they haven’t been tested.[22]Sitruk-Ware, R. (2006). New progestagens for contraceptive use. Human Reproduction Update. 12(2). 169-178. Available at: https://doi.org/10.1093/humupd/dmi046
Dosing Considerations
Oral micronized progesterone is typically prescribed at 200 mg daily for 12 days per 28-day cycle for postmenopausal women or 400 mg daily for 10 days for women who have not had a period for at least three consecutive months.[23]Memi, E., Pavli, P., Papagianni, M., Vrachnis, N., Mastorakos, G. (2024). Diagnostic and therapeutic use of oral micronized progesterone in endocrinology. Reviews in endocrine and metabolic … Continue reading It may be beneficial for women with female pattern hair loss.
Topical progesterone creams are often used in doses ranging from 20 to 40 mg, applied once or twice daily. For example, one study conducted with post-menopausal women used 40 mg daily or 20 mg twice daily for 42 days.[24]Carey, B.J., Carey, A.H., Patel, S., Carter, G., Studd, J.W. (2000). A study to evaluate serum and urinary hormone levels following short and long term administration of two regimens of progesterone … Continue reading
Injectable progesterone is injected primarily at around 150 mg every 12 weeks.[25]Nelson, A., (2002). Merits of DMPA relative to other reversible contraceptive methods. Journal of Reproductive Medicine. 47(9). 781-784. PMID: 12380406
Based on the research above, the dose for cyproterone acetate is around 50 – 100 mg, but this was given with ethinyl estradiol. For Slynd, the standard contraceptive dose of 4 mg orally once daily for 24 days followed by 4 inactive days may have potential benefits.
Dosing should be individualized based on the patient’s age, health status, and specific hormonal imbalances. Patients should report any concerning side effects to their doctor straight away. Close monitoring and adjustment of dosage by a healthcare provider are important, as effects can vary between individuals.
Best Practices
- Premenopausal Women: Progesterone supplementation may be used to address hormonal imbalances contributing to hair thinning.
- Postmenopausal Women: HRT with progesterone is more common, particularly in combination with estrogen, to combat hair loss linked to reduced hormone levels during menopause.
- Individuals with Androgenic Hair Loss: Progesterone as an adjunct to other anti-androgen therapies (e.g., spironolactone) for hair loss management (if you are pre-menopausal).[26]Brough, K.R., Torgerson, R.R. (2017). Hormonal therapy in female pattern hair loss. International Journal of Women’s Dermatology. 3. 53-57. Available at: … Continue reading
- Key Considerations: Before starting progesterone therapy, it is important to undergo individualized hormone testing and consult with a healthcare provider. Monitor for side effects such as mood changes, weight gain, or changes in menstrual patterns
Ultimately, due to the lack of evidence, we believe that steering clear of synthetic progestins, for the most part, would be best until newer data comes out supporting their use in hair growth. As it stands there may be some promising candidates, but its clear from our research that there is a gap in the evidence.
Final Thoughts
While progesterone, particularly in topical and micronized formulations, may benefit women suffering from FPHL or other hormonally influenced hair loss, more high-quality research is needed. If you are thinking about using progesterone, consult with your doctor or healthcare professional to ensure that it is tailored to your needs.
References[+]
References ↑1 Nio-Kobayashi, J., Miyazaki, K., Hashiba, K., Okuda, K., Iwanaga, T. (2016). Histological analysis of arteriovenous anastomosis-like vessels established in the corpus luteum of cows during luteolysis. Journal of Ovarian Research. 9(67). 1-14. Available at: https://doi.org/10.1186/s13048-016-0277-0 ↑2 Mirihagelle, S., Hughes, J.R., Miller, D.J. (2022). Progesterone-induced sperm release from the oviduct sperm reservoir. Cells. 11(10). 1622. Available at: https://doi.org/10.3390/cells11101622 ↑3 Grymowicz, M., Rudnicka, E., Podfigurna, A., Napierała, P., Smolarczyk, R., Smolarczyk, K., Męczekalski, B. (2020). Hormonal effects on hair follicles. International Journal of Molecular Sciences. 21(15). 5342. Available at: https://doi.org/10.3390/ijms21155342 ↑4 Cleveland Clinic. (no date). Postpartum Hair Loss. Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/diseases/23297-postpartum-hair-loss (Accessed: September 2024) ↑5, ↑6 Van der Willigen, A.H., Peereboom-Wynia, J.D.R., van Joost, TH., Stolz, E. (1987). A preliminary study of the effect of 11a hydroxyprogesterone on hair growth in men suffering from androgenetic alopecia. Acta dermato-venereologica. 67(1). 82-85. PMID: 2436423 ↑7 Kalinchenko, S., Nikiforov, I., Samburskaya, O. (2022). BPH, Androgenic Alopecia, and Acne – Markers of Progesterone Deficiency. Journal of the Endocrine Society. 6. 431-432. Available at: https://doi.org/10.1210/jendso/bvac150 ↑8 Coombes, Z., Plant, K., Freire, C., Basit, A.W., Butler, P., Conlan, R.S., Gonzalez, D. (2021). Progesterone metabolism by human and rat hepatic and intestinal tissue. Pharmaceutics. 13(10). 1707. Available at: https://doi.org/10.3390/pharmaceutics13101707 ↑9 Roseway Labs. (2020). Topicals for Hair Loss. Roseway Labs. Available at: https://rosewaylabs.com/topicals-for-hair-loss/ (Accessed: September 2024) ↑10 Hargrove, J.T., Maxson, W.S., Wentz, A.C. (1989). Absorption of oral progesterone is influenced by vehicle and particle size. American Journal of Obstetrics and Gynecology. 161(4). 948-951. Available at: https://doi.org/10.1016/0002-9378(89)90759-x ↑11 de Lignieres, B. (1999). Oral micronized progesterone. Clinical Therapeutics. 21(1). 41-60. Available at: https://doi.org/10.1016/S0149-2917(00)88267-3 ↑12, ↑23 Memi, E., Pavli, P., Papagianni, M., Vrachnis, N., Mastorakos, G. (2024). Diagnostic and therapeutic use of oral micronized progesterone in endocrinology. Reviews in endocrine and metabolic disorders. 25(4). 751-772. Available at: https://doi.org/10.1007/s11154-024-09882-0 ↑13 Louw-du Toit, R., Perkins, M.S., Hapgood, J.P., Africander, D. (2017). Comparing the androgenic and estrogenic properties of progestins used in contraception and hormone therapy. Biochemical and Biophysical Research Communications. (491)1. 140-146. Available at: https://doi.org/10.1016/j.bbrc.2017.07.063 ↑14 Paterson, H., Clifton, J., Miller, D., Ashton, J., Harrison-Woolrych, M. (2007(. Hair loss with use of the levonorgestrel intrauterine device. Contraception 76. 306-309. Available at: https://doi.org/10.1016/j.contraception.2007.06.015 ↑15 Yokoyama, Y., Sato, S., Saito, Y. (2002). Alopecia related to low-dose oral contraceptives. Archives of Gynecology and Obstetrics. 47. 266-246. Available at: https://doi.org/10.1007/pl00007489 ↑16 Sinclair, R., Wewerinke, M., Jolley, D. (2005). Treatment of female pattern hair loss with oral antiandrogens. British Journal of Dermatology. 152(3). 466-473. Available at: https://doi.org/10.1111/j.1365-2133.2005.06218.x ↑17 Coneac, A., Muresan, A., Orasan, M.S. (2014). Antiandrogenic therapy with ciproterone acetate in female patients who suffer from both androgenic alopecia and acne vulgaris. Clujul Medical. 87(4). 226-234. Available at: https://doi.org/10.15386/cjmed-386 ↑18 Coneac, A., Muresan, A., Orasan, M.S. (2014). Antiandrogenic therapy with ciproterone acetate in female patients who suffer from both androgenic alopecia and acne vulgaris. Clujul Medical. 87(4). 226-234. Available at: https://doi.org/10.15386/cjmed-386 ↑19 Vexiau, P., Chaspoux, C., Boudou, P., Fiet, J., Jouanique, C., Hardy, N., Reygagne, P. (2002). Effects of minoxidil 2% vs. cyproterone acetate treatment on female androgenetic alopecia: a controlled, 12-month randomized trial. British Journal of Dermatology. 146(6). 992-999. Available at: https//doi.org/10.1046/j.1365-2133.2002.04798.x ↑20 Regidor, P.A., Mueller, A., Mayr, M. (2023). Pharmacological and metabolic effects of drospirenone as a progestin-only pill compared to combined formulations with estrogen. Womens Health (Lond). 19. 1-10. Available at: https://doi.org/10.1177/17455057221147388 ↑21 Iorizzo, M., Vincenzi, C., Voudouris, S., Piraccini, B.M., Tosti, A. (2006). Finasteride treatment of female pattern hair loss. Archives of Dermatology. 142(3). 298-302. Available at: https://doi.org/10.1001/archderm.142.3.298 ↑22 Sitruk-Ware, R. (2006). New progestagens for contraceptive use. Human Reproduction Update. 12(2). 169-178. Available at: https://doi.org/10.1093/humupd/dmi046 ↑24 Carey, B.J., Carey, A.H., Patel, S., Carter, G., Studd, J.W. (2000). A study to evaluate serum and urinary hormone levels following short and long term administration of two regimens of progesterone creams in postmenopausal women. BJOG. 107(6). 722-726. Available at: https://doi.org/10.1111/j.1471-0528.2000.tb13331.x ↑25 Nelson, A., (2002). Merits of DMPA relative to other reversible contraceptive methods. Journal of Reproductive Medicine. 47(9). 781-784. PMID: 12380406 ↑26 Brough, K.R., Torgerson, R.R. (2017). Hormonal therapy in female pattern hair loss. International Journal of Women’s Dermatology. 3. 53-57. Available at: https://doi.org/10.1016/j.ijwd.2017.01.001 CRABP2 is one of two genes found within the CRABP family alongside CRABP1. CRABP2 is a key regulator of retinoic acid, a vitamin A derivative, transporting it around the cell and helping its metabolism. Both CRABP2 and retinoic acid have been suggested in the literature to have roles in the maintenance of hair health. This is particularly evident for retinoic acid, which has been suggested to regulate hair health in a dose-dependent manner. A few studies have also investigated genetic variation in CRABP2, suggesting that some variants may be linked to hair loss. This article will explore how relevant CRABP2 is to hair loss treatment effectiveness and how to interpret your genetic results to make the correct treatment choice.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is CRABP2?
The cellular retinoic acid binding protein (CRABP) gene family is very small, consisting of just two members – cellular retinoic acid binding protein 1 (CRABP1) and cellular retinoic acid binding protein 2 (CRABP2). CRABP1 is expressed throughout the body, whereas CRABP2 expression is restricted to certain tissues, such as the skin. Both CRABP genes are high-affinity binding proteins of retinoic acid, which is a derivative of vitamin A. Although research has yet to fully elucidate their exact functions, it is understood that CRABP1 and CRABP2 both play a role in the transport and metabolism of retinoic acid.[1]Wei, L. N. (2016). Cellular retinoic acid binding proteins: Genomic and non-genomic functions and their regulation. The Biochemistry of Retinoid Signaling II: The Physiology of Vitamin A-Uptake, … Continue reading
In sheep, it has been shown that CRABP2 is highly expressed in dermal papilla cells (DPCs), which play a key role in the growth and development of hair follicles. Moreover, they showed that CRABP2 regulates the proliferation of DPCs and that the overexpression of CRABP2 promoted increased DPC proliferation. Although this research was conducted in cells taken from sheep, it does suggest that CRABP2 may play a role in the maintenance of hair.[2]He, M., Lv, X., Cao, X., Yuan, Z., Quan, K., Getachew, T., Mwacharo, J.M., Haile, A., Li, Y., Wang, S. and Sun, W. (2023). CRABP2 Promotes the Proliferation of Dermal Papilla Cells via the … Continue reading
These results suggest that increased expression of CRABP2 could be beneficial for hair loss. However, the association between CRABP2 and hair maintenance is slightly more complex than it first appears. In tissue taken from a mouse model of alopecia areata (AA), the expression of CRABP2 (both the gene and protein) was increased compared to control mice. Similarly, CRABP2 protein expression was higher in tissue taken from humans with AA. Ultimately, the findings of the paper suggest that increased retinoic acid synthesis may contribute to the pathogenesis of AA.[3]Duncan, F.J., Silva, K.A., Johnson, C.J., King, B.L., Szatkiewicz, J.P., Kamdar, S.P., Ong, D.E., Napoli, J.L., Wang, J., King Jr, L.E. and Whiting, D.A. (2013). Endogenous retinoids in the … Continue reading
Conversely, it has also been shown that a reduction in retinoic acid signaling may be associated with hair loss. Mice lacking a key retinoic acid receptor exhibited impaired anagen initiation within their hair follicles (the growing phase), which was likely a contributory factor in the progressive alopecia that these mice developed.[4]Li, M., Chiba, H., Warot, X., Messaddeq, N., Gérard, C., Chambon, P., & Metzger, D. (2001). RXRα ablation in skin keratinocytes results in alopecia and epidermal alterations. Development, … Continue reading
Further evidence has been added to support these findings, suggesting that retinoic acid signaling may contribute to AGA similarly to androgens. It is widely accepted that androgens drive the pathogenesis of AGA and lead to the miniaturization of hair follicles. However, a study conducted in 30 male patients with AGA revealed that genes involved in retinoic acid signaling are upregulated, suggesting that retinoic acid signaling may promote follicle miniaturization.[5]Ho, B.S.Y., Vaz, C., Ramasamy, S., Chew, E.G.Y., Mohamed, J.S., Jaffar, H., Hillmer, A., Tanavde, V., Bigliardi-Qi, M. and Bigliardi, P.L. (2019). Progressive expression of PPARGC1α is associated … Continue reading
Despite appearing contradictory, it is possible that all of these studies are accurate and that both a deficiency and excess of retinoic acid can contribute to hair loss. Indeed, the literature suggests that retinoic acid may regulate hair health in a dose-dependent manner, whereby the optimal and ‘healthy’ level of retinoic acid sits somewhere between low and high.[6]VanBuren, C. A., & Everts, H. B. (2022). Vitamin A in skin and hair: an update. Nutrients, 14(14), 2952. Available at: https://doi.org/10.3390/nu14142952
This leads to a somewhat paradoxical situation, as retinoic acid is necessary for hair growth, but it can also cause hair loss when present in high concentrations. Thus, the therapeutic use of retinoic acid in treating hair loss is a challenging prospect.[7]Sadgrove, N. J., & Simmonds, M. S. (2021). Topical and nutricosmetic products for healthy hair and dermal antiaging using “dual‐acting”(2 for 1) plant‐based peptides, hormones, and … Continue reading
That said, several studies have shown that the application of tretinoin, a type of retinoic acid, has beneficial effects in treating hair loss. One study was conducted on 56 patients with AGA, who were treated with either a placebo, 0.5% minoxidil, 0.025% tretinoin, or a combination of minoxidil and tretinoin.[8]Bazzano, G. S., Terezakis, N., & Galen, W. (1986). Topical tretinoin for hair growth promotion. Journal of the American Academy of Dermatology, 15(4), 880-893. Available at: … Continue reading Tretinoin treatment alone was shown to stimulate some hair regrowth in more than half of the patients who received the treatment. Further positive results were observed with combination treatment.
Figure 1: Level of hair regrowth after treatment with either a placebo, minoxidil (0.5%), tretinoin (0.025%), or a combination of tretinoin and minoxidil.[9]Bazzano, G. S., Terezakis, N., & Galen, W. (1986). Topical tretinoin for hair growth promotion. Journal of the American Academy of Dermatology, 15(4), 880-893. Available at: … Continue reading
This was also shown in a study conducted on 31 male patients with AGA. The study showed that once-daily application of tretinoin and minoxidil, in combination, was as effective at treating hair loss as twice-daily minoxidil on its own (Figure 1).[10]Shin, H. S., Won, C. H., Lee, S. H., Kwon, O. S., Kim, K. H., & Eun, H. C. (2007). Efficacy of 5% minoxidil versus combined 5% minoxidil and 0.01% tretinoin for male pattern hair loss: a … Continue reading
Figure 2: The effect of combined minoxidil and tretinoin or minoxidil alone on hair growth parameters.[11]Shin, H. S., Won, C. H., Lee, S. H., Kwon, O. S., Kim, K. H., & Eun, H. C. (2007). Efficacy of 5% minoxidil versus combined 5% minoxidil and 0.01% tretinoin for male pattern hair loss: a … Continue reading
What is the Evidence for Targeting CRABP2 for Hair Loss?
Collectively, the evidence does suggest that CRABP2 and retinoic acid are key factors in hair loss. Owing to this, it is feasible that genetic variation in CRABP2 could influence the efficacy of hair loss treatments.
In a study conducted on newborn babies, it was found that the rs12724719 polymorphism was linked to retinoic acid levels. Specifically, those with the AA genotype had a greater concentration of retinoic acid in the blood of their umbilical cord than those with the GA or GG genotypes. It is believed that such an increase in retinoic acid may have been caused by reduced CRABP2 expression, impairing its ability to transport retinoic acid into the nucleus of the cell.[12]Manolescu, D. C., El-Kares, R., Lakhal-Chaieb, L., Montpetit, A., Bhat, P. V., & Goodyer, P. (2010). Newborn serum retinoic acid level is associated with variants of genes in the retinol … Continue reading
Although this study was conducted in newborn umbilical cord blood, and so is probably not representative of how the genetic variant affects adults or hair, the results are still interesting. If adults with the AA genotype also exhibit increased levels of retinoic acid, then therapeutic supplementation with retinoic acid to treat hair loss may be less effective in those individuals. Moreover, given that retinoic acid levels are already high, increasing levels further may increase the risk of those individuals experiencing retinoic acid-induced hair loss, as discussed earlier.
A separate study was conducted on over 25,000 patients with AGA, a mix of both males and females. Interestingly, their analysis revealed an association between the rs12724719 polymorphism and AGA. Unfortunately, the authors did not specifically state which of the genotypes were linked to AGA and which were not. However, this is yet another indication that genetic variation in CRABP2 and the rs12724719 polymorphism may influence hair health and treatments.[13]Francès, M. P., Vila-Vecilla, L., Russo, V., Caetano Polonini, H., & de Souza, G. T. (2024). Utilising SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia … Continue reading
What Do Your Genetic Results Mean?
Your Result CRABP2 (rs12724719)
Variant 1 – GG genotype
Variant 2 – GA genotype Variant 3 – AA genotype
What it Means Associated with normal levels of retinoic acid in the blood Associated with normal levels of retinoic acid in the blood Associated with elevated levels of retinoic acid in the blood The Implication May benefit from retinoic acid supplementation May benefit from retinoic acid supplementation May not benefit from retinoic acid treatment (i.e, vitamin A supplementation or retinoid topicals) What Relevance Does CRABP2 Have for Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes. CRABP2 has been found to be upregulated in patients with alopecia areata (score = 1)
- Does the totality of evidence implicate CRABP2 as a causal agent for hair loss? (1 point)
No. There is very little published literature that indicates CRABP2 causes hair loss. (score = 0)
- Does the totality of evidence implicate CRABP2 as a predictive factor for hair loss treatment responsiveness? (2 points)
No. There is no published literature that shows that CRABP2 polymorphisms affect hair loss treatments (score = 0)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
Since CRABP2 fails question #3, it cannot be awarded points for question #4 (score = 0)
Total Score = 1
Final Thoughts
While there is evidence that genetic variation in CRABP2 is associated with AGA and may affect retinoic acid levels, the evidence is not yet sufficient to make definitive treatment recommendations based solely on genotype. Importantly, no studies have yet explored how genetic variation in CRABP2 affects treatment with retinoic acid or any other therapeutic. Additional studies that seek to answer this question must be conducted to confirm the true predictive value of testing CRABP2 variants to personalize hair treatments.
References[+]
References ↑1 Wei, L. N. (2016). Cellular retinoic acid binding proteins: Genomic and non-genomic functions and their regulation. The Biochemistry of Retinoid Signaling II: The Physiology of Vitamin A-Uptake, Transport, Metabolism and Signaling, 163-178. Available at: https://doi.org/10.1007/978-94-024-0945-1_6 ↑2 He, M., Lv, X., Cao, X., Yuan, Z., Quan, K., Getachew, T., Mwacharo, J.M., Haile, A., Li, Y., Wang, S. and Sun, W. (2023). CRABP2 Promotes the Proliferation of Dermal Papilla Cells via the Wnt/β-Catenin Pathway. Animals, 13(12), 2033. Available at: https://doi.org/10.3390/ani13122033 ↑3 Duncan, F.J., Silva, K.A., Johnson, C.J., King, B.L., Szatkiewicz, J.P., Kamdar, S.P., Ong, D.E., Napoli, J.L., Wang, J., King Jr, L.E. and Whiting, D.A. (2013). Endogenous retinoids in the pathogenesis of alopecia areata. Journal of Investigative Dermatology, 133(2), 334-343. Available at: https://doi.org/10.1038/jid.2012.344 ↑4 Li, M., Chiba, H., Warot, X., Messaddeq, N., Gérard, C., Chambon, P., & Metzger, D. (2001). RXRα ablation in skin keratinocytes results in alopecia and epidermal alterations. Development, 128(5), 675-688. Available at: https://doi.org/10.1242/dev.128.5.675 ↑5 Ho, B.S.Y., Vaz, C., Ramasamy, S., Chew, E.G.Y., Mohamed, J.S., Jaffar, H., Hillmer, A., Tanavde, V., Bigliardi-Qi, M. and Bigliardi, P.L. (2019). Progressive expression of PPARGC1α is associated with hair miniaturization in androgenetic alopecia. Scientific reports, 9(1), 8771. Available at: https://doi.org/10.1038/s41598-019-43998-7 ↑6 VanBuren, C. A., & Everts, H. B. (2022). Vitamin A in skin and hair: an update. Nutrients, 14(14), 2952. Available at: https://doi.org/10.3390/nu14142952 ↑7 Sadgrove, N. J., & Simmonds, M. S. (2021). Topical and nutricosmetic products for healthy hair and dermal antiaging using “dual‐acting”(2 for 1) plant‐based peptides, hormones, and cannabinoids. FASEB BioAdvances, 3(8), 601. Available at: https://doi.org/10.1096/fba.2021-00022 ↑8, ↑9 Bazzano, G. S., Terezakis, N., & Galen, W. (1986). Topical tretinoin for hair growth promotion. Journal of the American Academy of Dermatology, 15(4), 880-893. Available at: https://doi.org/10.1016/S0190-9622(86)80024-X ↑10, ↑11 Shin, H. S., Won, C. H., Lee, S. H., Kwon, O. S., Kim, K. H., & Eun, H. C. (2007). Efficacy of 5% minoxidil versus combined 5% minoxidil and 0.01% tretinoin for male pattern hair loss: a randomized, double-blind, comparative clinical trial. American journal of clinical dermatology, 8, 285-290. Available at: https://doi.org/10.2165/00128071-200708050-00003 ↑12 Manolescu, D. C., El-Kares, R., Lakhal-Chaieb, L., Montpetit, A., Bhat, P. V., & Goodyer, P. (2010). Newborn serum retinoic acid level is associated with variants of genes in the retinol metabolism pathway. Pediatric research, 67(6), 598-602. Available at: https://doi.org/10.1203/PDR.0b013e3181dcf18a ↑13 Francès, M. P., Vila-Vecilla, L., Russo, V., Caetano Polonini, H., & de Souza, G. T. (2024). Utilising SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia Treatment. Dermatology and Therapy, 14(4), 971-981. Available at: https://doi.org/10.1007/s13555-024-01142-y CYP19A1 is a gene within the cytochrome P450 superfamily, a large network of genes that regulate various critical processes throughout the body. CYP19A1 encodes the protein aromatase, which is involved in the conversion of androgens, such as testosterone, into estrogens. Aromatase is believed to play a key role in regulating hair growth, and several studies have also linked aromatase activity to hair loss. A handful of studies have also investigated genetic variation in CYP19A1, suggesting that some variants may cause differential responses to hair loss treatments. This article will explore how relevant CYP19A1 is to hair treatment effectiveness and how to interpret your genetic results to make the correct treatment choice.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Is CYP19A1?
Cytochrome P450 Family 19 Subfamily A Member 1, known as CYP19A1, is part of the cytochrome P450 superfamily. The human genome contains at least 57 genes that belong to various CYP sub-families, collectively regulating several critical roles throughout the body. CYP19A1 encodes the protein aromatase, an enzyme involved in converting androgens to estrogens, such as androgen, into estradiol. For this reason, aromatase is also known as estrogen synthase.[1]Nebert, D. W., Wikvall, K., & Miller, W. L. (2013). Human cytochromes P450 in health and disease. Philosophical Transactions of the Royal Society B: Biological Sciences, 368(1612), 20120431. … Continue reading
Many studies have linked aromatase as a key regulatory factor in hair growth for several years. One such study was conducted on growing (anagen) phase hairs taken from female participants with and without female pattern hair loss (FPHL). Analysis of the hairs revealed that CYP19A1 expression was significantly lower in the participants with FPHL.[2]Sánchez, P., Serrano-Falcón, C., Torres, J. M., Serrano, S., & Ortega, E. (2018). 5α-Reductase isozymes and aromatase mRNA levels in plucked hair from young women with female pattern hair … Continue reading
Similarly, another study measured the aromatase levels in the hair follicles of men and women with androgenic alopecia (AGA). The follicles were taken from different regions of the head, revealing that aromatase levels were higher in the occipital (non-balding) region than in the frontal (balding) region. This difference was identified in both males and females. Still, interestingly, it was also found that aromatase levels were six times higher in the frontal hair follicles of women than in men. This could explain the differences in male and female hair loss patterns.[3]Sawaya, M. E., & Price, V. H. (1997). Different levels of 5α-reductase type I and II, aromatase, and androgen receptor in hair follicles of women and men with androgenetic alopecia. Journal of … Continue reading
Figure 1: Differences in aromatase activity in men and women.[4]Sawaya, M. E., & Price, V. H. (1997). Different levels of 5α-reductase type I and II, aromatase, and androgen receptor in hair follicles of women and men with androgenetic alopecia. Journal of … Continue reading
Associations between aromatase and hair loss have been underlined by the discovery that aromatase inhibitors can lead to the thinning and loss of hair. An analysis of 851 female breast cancer survivors revealed that those who underwent aromatase inhibitor therapy were significantly more likely to report hair loss and hair thinning than those who did not. Moreover, this association was independent of factors such as chemotherapy and radiotherapy, highlighting the importance of aromatase.[5]Gallicchio, L., Calhoun, C., & Helzlsouer, K. J. (2013). Aromatase inhibitor therapy and hair loss among breast cancer survivors. Breast cancer research and treatment, 142, 435-443. Available at: … Continue reading
Although not yet fully understood, the role of aromatase in hair loss is thought to be based on its influence on estrogen, testosterone, and dihydrotestosterone (DHT). In converting testosterone to estradiol, aromatase reduces testosterone levels and, importantly, reduces the amount of testosterone converted to DHT. High levels of DHT have been implicated in the pathogenesis of AGA. These interactions could explain the association between reduced aromatase activity and hair loss.[6]Rossi, A., Caro, G., Magri, F., Fortuna, M. C., & Carlesimo, M. (2021). Clinical aspect, pathogenesis and therapy options of alopecia induced by hormonal therapy for breast cancer. Exploration of … Continue reading
Indeed, it has been shown that aromatase inhibition in mice led to decreased levels of estradiol (a form of estrogen) and increased levels of DHT.[7]Iqbal, R., Jain, G. K., Siraj, F., & Vohora, D. (2018). Aromatase inhibition by letrozole attenuates kainic acid-induced seizures but not neurotoxicity in mice. Epilepsy Research, 143, 60-69. … Continue reading Similar results were reported in men, with aromatase inhibition leading to increased levels of testosterone and DHT. However, it should be noted that this study was conducted on older men who generally have lower levels of testosterone, so the results may not be representative of testosterone modulation in the wider population.[8]Leder, B. Z., Rohrer, J. L., Rubin, S. D., Gallo, J., & Longcope, C. (2004). Effects of aromatase inhibition in elderly men with low or borderline-low serum testosterone levels. The Journal of … Continue reading
Figure 2: Effect of anastrozole (an aromatase inhibitor) on serum testosterone, free testosterone, and dihydrotestosterone in men aged 62-74 years.[9]Leder, B. Z., Rohrer, J. L., Rubin, S. D., Gallo, J., & Longcope, C. (2004). Effects of aromatase inhibition in elderly men with low or borderline-low serum testosterone levels. The Journal of … Continue reading
A recent study has even suggested that Minoxidil, the first FDA-approved treatment for AGA, may exert its effects via interaction with aromatase. They found that Minoxidil increases the activity of aromatase, suggesting that Minoxidil may help to treat AGA by increasing the production of estradiol and decreasing the production of DHT.[10]Shen, Y., Zhu, Y., Zhang, L., Sun, J., Xie, B., Zhang, H., & Song, X. (2023). New target for minoxidil in the treatment of androgenetic alopecia. Drug Design, Development and Therapy, 2537-2547. … Continue reading
Figure 3: Human epidermal-dermal papilla cells treated with minoxidil showed an increase in mRNA levels of CYP19A1, indicating that it enhances the activity of aromatase.[11]Shen, Y., Zhu, Y., Zhang, L., Sun, J., Xie, B., Zhang, H., & Song, X. (2023). New target for minoxidil in the treatment of androgenetic alopecia. Drug Design, Development and Therapy, 2537-2547. … Continue reading
What Is The Evidence for Targeting CYP19A1 For Hair Loss?
Collectively, a significant amount of evidence suggests that aromatase is a key factor in hair loss. Owing to this, it is feasible that genetic variation in CYP19A1 could influence the efficacy of hair loss treatments.
In a study conducted on patients with polycystic ovary syndrome (PCOS), the rs2470152 single nucleotide polymorphism (SNP) in CYP19A1 was suggested to be associated with decreased aromatase activity. Namely, participants with PCOS and the TC genotype were found to exhibit increased levels of testosterone and a reduced ratio of estradiol to testosterone. In participants without PCOS, those with the TC genotype also exhibited a lower ratio of estradiol to testosterone.[12]Zhang, X.L., Zhang, C.W., Xu, P., Liang, F.J., Che, Y.N., Xia, Y.J., Cao, Y.X., Wu, X.K., Wang, W.J., Yi, L. and Gao, Q. (2012). SNP rs2470152 in CYP19 is correlated to aromatase activity in Chinese … Continue reading
Figure 4: Characteristics and serum hormone concentrations in different genotypes of women with and without PCOS. Of interest is the TC genotype; participants exhibited an increased level of estradiol (E2) and a decreased E2/T ratio (meaning increased testosterone and decreased estradiol).[13]Zhang, X.L., Zhang, C.W., Xu, P., Liang, F.J., Che, Y.N., Xia, Y.J., Cao, Y.X., Wu, X.K., Wang, W.J., Yi, L. and Gao, Q. (2012). SNP rs2470152 in CYP19 is correlated to aromatase activity in Chinese … Continue reading
People with the TC genotype may benefit from treatment with estradiol or anti-androgen drugs, given the associations between low estrogen levels, high androgen levels, and hair loss. However, it should be noted that this study was conducted on participants with PCOS; the rs2470152 SNP has not been linked to AGA or other types of hair loss, meaning it may not affect their treatment.
Furthermore, as stated earlier, the relationship between estrogen androgen levels and hair loss is still not understood. Although associations between low estrogen levels and hair loss have been identified, so too have associations between high estrogen levels and hair loss. A study involving 955 females discovered that participants with the rs4646 SNP CC genotype had an increased risk of developing FPHL.[14]Yip, L., Zaloumis, S., Irwin, D., Severi, G., Hopper, J., Giles, G., Harrap, S., Sinclair, R. and Ellis, J. (2009). Gene‐wide association study between the aromatase gene (CYP19A1) and female … Continue reading
Interestingly, the rs4646 SNP CC genotype had previously been shown to be associated with higher estrogen levels in postmenopausal females.[15]Haiman, C.A., Dossus, L., Setiawan, V.W., Stram, D.O., Dunning, A.M., Thomas, G., Thun, M.J., Albanes, D., Altshuler, D., Ardanaz, E. and Boeing, H. (2007). Genetic variation at the CYP19A1 locus … Continue reading The suggestion that higher estrogen levels may increase the risk of developing FPHL contradicts previous literature on the subject, indicating that genetics alone are not sufficient to make treatment recommendations.
Another study investigated the effects of genetic variation on dutasteride treatment, a drug used off-label in treating hair loss. They identified a positive association between the rs700519 SNP in CYP19A1 and the efficacy of dutasteride; in other words, people with this genetic variant responded better to treatment.[16]Rhie, A., Son, H.Y., Kwak, S.J., Lee, S., Kim, D.Y., Lew, B.L., Sim, W.Y., Seo, J.S., Kwon, O., Kim, J.I. and Jo, S.J. (2019). Genetic variations associated with response to dutasteride in the … Continue reading
Figure 5: Genotypic landscape of 42 patients, the cumulative effect of each allele count, and their positive or negative effect. Boxes represent SNPs that exhibited a positive (blue) or negative (red) effect on the patient’s response to dutasteride. Light-colored boxes represent heterozygous SNPs (a variation where an individual has two different versions of a specific DNA sequence at a particular location in the genome), dark-colored boxes represent homozygous SNPs (a variation where an individual has two identical versions of a specific DNA sequence at a particular location in the genome). Patient responses to dutasteride improve from left to right.[17]Rhie, A., Son, H.Y., Kwak, S.J., Lee, S., Kim, D.Y., Lew, B.L., Sim, W.Y., Seo, J.S., Kwon, O., Kim, J.I. and Jo, S.J. (2019). Genetic variations associated with response to dutasteride in the … Continue reading
Despite this positive association, some patients classified as ‘poor responders’ also had the rs700519 SNP. This indicates that having a ‘positive’ SNP in CYP19A1 does not guarantee that you will respond well to dutasteride. Rather, the study presents the likelihood that the combination of SNPs that one possesses is more important.
What Do Your Genetic Results Mean?
Your Result CYP19A1 (rs2470152)
Variant 1 – TT genotype Variant 2 – CC genotype Variant 3 – TC genotype
What it means Not associated with a change in testosterone or estrogen levels Not associated with a change in testosterone or estrogen levels Associated with reduced expression of CYP19A1 and, therefore, an increase in testosterone levels/decrease in estrogen levels The Implication May not benefit from estradiol or anti-androgens May not benefit from estradiol or anti-androgens May benefit from treatment with estradiol as a replacement hormone or anti-androgen drugs Your Result CYP19A1 (rs700519)
Variant 1 – CC genotype
Variant 2 – CT genotype Variant 3 – TT genotype
What it means May be a normal/poor responder to 5α-reductase inhibitors May be a good responder to 5α-reductase inhibitors May be a good responder to 5α-reductase inhibitors The Implication May be a good candidate for typical/higher dosages of 5α-reductase inhibitors May be a good candidate for lower dosages of 5α-reductase inhibitors May be a good candidate for lower dosages of 5α-reductase inhibitors What Relevance Does CYp19A1 Have For Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes. A decrease in aromatase may lead to an increase in testosterone and, subsequently, DHT, which are linked with androgenetic alopecia. (score=1)
- Does the totality of evidence implicate CYP19A1 as a causal agent for hair loss? (1 point)
While there are some hypotheses about how SNPs in CYP19A1 may lead to hair loss, there is no published evidence showing this possible association. (score = 0)
- Does the totality of evidence implicate CYP19A1 as a predictive factor for hair loss treatment responsiveness? (2 points)
No, the data does not suggest that CYP19A1 can be used as a predictor for hair loss treatment responsiveness. (score = 0)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
Since CYP19A1 fails question #3, it cannot be awarded points for question #4 (score = 0)
Total Score = 1
Final Thoughts
While one small study suggests that genetic variation in CYP19A1 may influence your response to treatment with a 5α-reductase inhibitor, the evidence is not yet strong enough to make definitive treatment recommendations based solely on genotype. Furthermore, some evidence regarding CYP19A1 and its associations with hair loss conditions is contradictory. Larger and more robust studies are needed to confirm the true predictive value of genetic testing for CYP19A1 variants to personalize hair loss treatments.
References[+]
References ↑1 Nebert, D. W., Wikvall, K., & Miller, W. L. (2013). Human cytochromes P450 in health and disease. Philosophical Transactions of the Royal Society B: Biological Sciences, 368(1612), 20120431. Available at: https://doi.org/10.1098/rstb.2012.0431 ↑2 Sánchez, P., Serrano-Falcón, C., Torres, J. M., Serrano, S., & Ortega, E. (2018). 5α-Reductase isozymes and aromatase mRNA levels in plucked hair from young women with female pattern hair loss. Archives of dermatological research, 310, 77-83. Available at: https://doi.org/10.1007/s00403-017-1798-0 ↑3, ↑4 Sawaya, M. E., & Price, V. H. (1997). Different levels of 5α-reductase type I and II, aromatase, and androgen receptor in hair follicles of women and men with androgenetic alopecia. Journal of Investigative Dermatology, 109(3), 296-300. Available at: https://doi.org/10.1111/1523-1747.ep12335779 ↑5 Gallicchio, L., Calhoun, C., & Helzlsouer, K. J. (2013). Aromatase inhibitor therapy and hair loss among breast cancer survivors. Breast cancer research and treatment, 142, 435-443. Available at: https://doi.org/10.1007/s10549-013-2744-2 ↑6 Rossi, A., Caro, G., Magri, F., Fortuna, M. C., & Carlesimo, M. (2021). Clinical aspect, pathogenesis and therapy options of alopecia induced by hormonal therapy for breast cancer. Exploration of Targeted Anti-tumor Therapy, 2(5), 490. Available at: https://doi.org/10.37349/etat.2021.00059 ↑7 Iqbal, R., Jain, G. K., Siraj, F., & Vohora, D. (2018). Aromatase inhibition by letrozole attenuates kainic acid-induced seizures but not neurotoxicity in mice. Epilepsy Research, 143, 60-69. Available at: https://doi.org/10.1016/j.eplepsyres.2018.04.004 ↑8, ↑9 Leder, B. Z., Rohrer, J. L., Rubin, S. D., Gallo, J., & Longcope, C. (2004). Effects of aromatase inhibition in elderly men with low or borderline-low serum testosterone levels. The Journal of Clinical Endocrinology & Metabolism, 89(3), 1174-1180. Available at: https://doi.org/10.1210/jc.2003-031467 ↑10, ↑11 Shen, Y., Zhu, Y., Zhang, L., Sun, J., Xie, B., Zhang, H., & Song, X. (2023). New target for minoxidil in the treatment of androgenetic alopecia. Drug Design, Development and Therapy, 2537-2547. Available at: https://doi.org/10.2147/DDDT.S427612 ↑12, ↑13 Zhang, X.L., Zhang, C.W., Xu, P., Liang, F.J., Che, Y.N., Xia, Y.J., Cao, Y.X., Wu, X.K., Wang, W.J., Yi, L. and Gao, Q. (2012). SNP rs2470152 in CYP19 is correlated to aromatase activity in Chinese polycystic ovary syndrome patients. Molecular Medicine Reports, 5(1), 245-249. Available at: https://doi.org/10.3892/mmr.2011.616 ↑14 Yip, L., Zaloumis, S., Irwin, D., Severi, G., Hopper, J., Giles, G., Harrap, S., Sinclair, R. and Ellis, J. (2009). Gene‐wide association study between the aromatase gene (CYP19A1) and female pattern hair loss. British Journal of Dermatology, 161(2), 289-294. Available at: https://doi.org/10.1111/j.1365-2133.2009.09186.x ↑15 Haiman, C.A., Dossus, L., Setiawan, V.W., Stram, D.O., Dunning, A.M., Thomas, G., Thun, M.J., Albanes, D., Altshuler, D., Ardanaz, E. and Boeing, H. (2007). Genetic variation at the CYP19A1 locus predicts circulating estrogen levels but not breast cancer risk in postmenopausal women. Cancer research, 67(5), 1893-1897. Available at: https://doi.org/10.1158/0008-5472.CAN-06-4123 ↑16, ↑17 Rhie, A., Son, H.Y., Kwak, S.J., Lee, S., Kim, D.Y., Lew, B.L., Sim, W.Y., Seo, J.S., Kwon, O., Kim, J.I. and Jo, S.J. (2019). Genetic variations associated with response to dutasteride in the treatment of male subjects with androgenetic alopecia. Plos one, 14(9), e0222533. Available at: https://doi.org/10.1371/journal.pone.0222533 COL1A1 is a gene within the collagen superfamily, a large network that comprises at least 44 genes and 28 proteins. The collagen proteins have a variety of roles, with perhaps their most crucial being to support the structure of tissues throughout the body. COL1A1 and COL1A2 produce the protein chains that combine to form type 1 collagen, the most abundant type of collagen in the body, which has also been linked to regulating hair growth. Moreover, some studies have suggested that genetic variation in COL1A1 may cause differential responses to hair loss treatment.
This article will explore how relevant COL1A1 is to hair treatment effectiveness and how to interpret your genetic results to make the correct treatment choice.
All-Natural Hair Supplement
The top natural ingredients for hair growth, all in one supplement.
Take the next step in your hair growth journey with a world-class natural supplement. Ingredients, doses, & concentrations built by science.

What Is COL1A1?
Collagen Type I Alpha 1 Chain, or COL1A1, is part of the collagen superfamily. There are 44 genes encoding the proteins that make up the 28 different types of collagen, with some collagen types consisting of more than one protein (α chain).[1]Ricard-Blum, S. (2011). The collagen family. Cold Spring Harbor perspectives in biology, 3(1), a004978. Available at: https://doi.org/10.1101/cshperspect.a004978 Collagens have a variety of key roles throughout the body, foremost of which is the promotion of cell growth and supporting the structure and organization of tissues.[2]Sun, H., Wang, Y., Wang, S., Xie, Y., Sun, K., Li, S., Cui, W. and Wang, K. (2023). The involvement of collagen family genes in tumor enlargement of gastric cancer. Scientific Reports, 13(1), 100. … Continue reading
Type 1 collagen (COL1) is the most abundant of all collagen types within the body, representing over a quarter of the total protein content in mammals. It consists of two α1 chains, produced by COL1A1, and one α2 chain, produced by Collagen Type I Alpha 2 Chain (COL1A2). The three α chains assemble into a single procollagen and undergo multiple rounds of modification, with several molecules eventually assembling into a longer collagen fibril and, finally, a type 1 collagen fiber (Figure 1).[3]Kruger, T. E., Miller, A. H., & Wang, J. (2013). Collagen scaffolds in bone sialoprotein‐mediated bone regeneration. The Scientific World Journal, 2013(1), 812718. Available at: … Continue reading
Figure 1: How Type I Collagen is Made in the Body. (a) The process starts with three protein chains: two identical α1(I) chains and one α2(I) chain. (b) These three chains twist together to form a structure called procollagen. (c) An enzyme called procollagen peptidase comes along and snips off the loose ends of the procollagen.(d) After the trimming, what’s left is called a tropocollagen molecule. This is the basic building block of collagen. (e) Multiple tropocollagen molecules then line up and stick together, forming a thin strand called a collagen fibril. This fibril keeps growing as more tropocollagen molecules join in. (f) Finally, many of these collagen fibrils bundle together to create a sturdy collagen fiber. This is the form of collagen that gives strength to our skin, bones, and other tissues.[4]Kruger, T. E., Miller, A. H., & Wang, J. (2013). Collagen scaffolds in bone sialoprotein‐mediated bone regeneration. The Scientific World Journal, 2013(1), 812718. Available at: … Continue reading
Given its abundance within the body, it is hardly surprising that COL1 has been detected in the scalp. Specifically, the connective tissue sheath surrounding the hair follicle was found to be a major source of type 1 procollagen, expressing greater amounts than other parts of the follicle. Moreover, they showed that the expression of type 1 collagen changes throughout the hair cycle, collectively indicating that type 1 collagen may play a key role in the growth and structure of hair follicles.[5]Oh, J.K., Kwon, O.S., Kim, M.H., Jo, S.J., Han, J.H., Kim, K.H., Eun, H.C. and Chung, J.H. (2012). Connective tissue sheath of hair follicle is a major source of dermal type I procollagen in human … Continue reading
These results support an earlier study that found that Col1 levels in mice also changed based on the stage of the hair cycle. They found that levels of Col1 were approximately two-fold higher in the dermis of the skin in the anagen (growing) phase than skin in the telogen (resting) phase. Furthermore, they found that Col1 molecules underwent more modifications during the anagen phase. This indicates that the remodeling of collagen is more active in anagen skin, which may support the growth and migration of hair follicles.[6]Yamamoto, & Yamauchi. (1999). Characterization of dermal type I collagen of C3H mouse at different stages of the hair cycle. British Journal of Dermatology, 141(4), 667-675. Available at: … Continue reading
What is the Evidence for Targeting COL1A1 For Hair Loss?
Although only a few studies have investigated COL1 in relation to hair health, the evidence they have provided is robust and certainly suggests that COL1 may well be an important factor in regulating hair growth. Owing to this, it is feasible that genetic variation in COL1A1 could influence hair loss treatments.
Research into the rs1800012 polymorphism of Col1 revealed that people with the GT genotype had a higher ratio of COL1A1:COL1A2 gene expression and α1:α2 chains than the GG genotype. Generally existing in a 2:1 ratio, due to the structure of COL1, any increase in this ratio would lead to an imbalance between the two types of α chain.[7]Mann, V., Hobson, E.E., Li, B., Stewart, T.L., Grant, S.F., Robins, S.P., Aspden, R.M. and Ralston, S.H. (2001). A COL1A1 Sp1 binding site polymorphism predisposes to osteoporotic fracture by … Continue reading
This could lead to instability of the collagen molecules, indicating that it may be useful for people who exhibit this genotype to take supplements that might support collagen synthesis, such as silicon, cysteine, or collagen.
Figure 2: Collagen protein and mRNA levels in osteoblasts (cells that form new bones) cultured from patients with different genotypes. Different genotypes of the rs1800012 polymorphism are shown. SS genotype = GG genotype; Ss genotype = GT genotype.[8]Mann, V., Hobson, E.E., Li, B., Stewart, T.L., Grant, S.F., Robins, S.P., Aspden, R.M. and Ralston, S.H. (2001). A COL1A1 Sp1 binding site polymorphism predisposes to osteoporotic fracture by … Continue reading
Furthermore, in an analysis of over 26,000 people, it was found that the rs1800012 polymorphism is associated with AGA. Unfortunately, the study does not state which specific genotypes are associated with AGA, but this does suggest that the rs1800012 polymorphism and COL1A1 play a role in hair loss. [9]Francès, M. P., Vila-Vecilla, L., Russo, V., Caetano Polonini, H., & de Souza, G. T. (2024). Utilising SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia … Continue reading
It has also been found that COL1A1 expression is upregulated in people with AGA. However, the upregulation of COL1A1 was not linked to the rs1800012 polymorphism. Moreover, the same study also showed that the expression of COL1A2 is upregulated in people with AGA, which may cause the α1:α2 chain ratio to remain unchanged.[10]Michel, L., Reygagne, P., Benech, P., Jean‐Louis, F., Scalvino, S., Ly Ka So, S., Hamidou, Z., Bianovici, S., Pouch, J., Ducos, B. and Bonnet, M., 2017. Study of gene expression alteration in male … Continue reading
Together, although these studies do suggest that COL1A1 and the rs1800012 polymorphism may be involved in hair loss, they also indicate that the underlying mechanism is not understood. Further studies are required to understand how the expression of COL1A1 and COL1A2, the rs1800012 polymorphism, and the α1:α2 chain ratio link to hair loss and AGA.
What Do Your Genetic Results Mean?
Your Result
COL1A1 (rs1800012) Variant 1 – GG genotype Variant 2 – GT genotype What it means Normal α1 chain synthesis Increased α1 chain synthesis The Implication May not benefit from supplementation that supports collagen formation May benefit from supplementation that supports collagen formation, such as adenosine or cysteine
What Relevance Does COL1A1 Have for Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes, COL1A1 and COL1A2 have been found to be overexpressed in patients with androgenetic alopecia (score=1)
- Does the totality of evidence implicate COL1A1 as a causal agent for hair loss? (1 point)
No, there is no published evidence to suggest that COL1A1 polymorphisms can cause hair loss (score = 0)
- Does the totality of evidence implicate COL1A1 as a predictive factor for hair loss treatment responsiveness? (2 points)
No, there is no data to suggest that COL1A1 polymorphisms can be used as a predictor for hair loss treatment responsiveness (score = 0)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
Since COL1A1 fails question #3, it cannot be awarded points for question #4 (score = 0)
Total Score = 1
Final Thoughts
While there is some evidence to suggest that genetic variation in COL1A1 may influence your response to treatment with collagen supplements, there is not yet strong enough evidence to make definitive treatment recommendations based solely on genotype. Furthermore, it is evident that the association(s) between COL1A1, rs1800012, and hair loss are not yet understood. Larger and more robust studies are needed to confirm the true predictive value of genetic testing for COL1A1 variants to personalize hair loss treatments.
References[+]
References ↑1 Ricard-Blum, S. (2011). The collagen family. Cold Spring Harbor perspectives in biology, 3(1), a004978. Available at: https://doi.org/10.1101/cshperspect.a004978 ↑2 Sun, H., Wang, Y., Wang, S., Xie, Y., Sun, K., Li, S., Cui, W. and Wang, K. (2023). The involvement of collagen family genes in tumor enlargement of gastric cancer. Scientific Reports, 13(1), 100. Available at: https://doi.org/10.1038/s41598-022-25061-0 ↑3, ↑4 Kruger, T. E., Miller, A. H., & Wang, J. (2013). Collagen scaffolds in bone sialoprotein‐mediated bone regeneration. The Scientific World Journal, 2013(1), 812718. Available at: https://doi.org/10.1155/2013/812718 ↑5 Oh, J.K., Kwon, O.S., Kim, M.H., Jo, S.J., Han, J.H., Kim, K.H., Eun, H.C. and Chung, J.H. (2012). Connective tissue sheath of hair follicle is a major source of dermal type I procollagen in human scalp. Journal of Dermatological Science, 68(3), 194-197. Available at: https://doi.org/10.1016/j.jdermsci.2012.09.006 ↑6 Yamamoto, & Yamauchi. (1999). Characterization of dermal type I collagen of C3H mouse at different stages of the hair cycle. British Journal of Dermatology, 141(4), 667-675. Available at: https://doi.org/10.1046/j.1365-2133.1999.03105.x ↑7 Mann, V., Hobson, E.E., Li, B., Stewart, T.L., Grant, S.F., Robins, S.P., Aspden, R.M. and Ralston, S.H. (2001). A COL1A1 Sp1 binding site polymorphism predisposes to osteoporotic fracture by affecting bone density and quality. The Journal of Clinical Investigation, 107(7), 899-907. Available at: https://doi.org/10.1172/JCI10347 ↑8 Mann, V., Hobson, E.E., Li, B., Stewart, T.L., Grant, S.F., Robins, S.P., Aspden, R.M. and Ralston, S.H. (2001). A COL1A1 Sp1 binding site polymorphism predisposes to osteoporotic fracture by affecting bone density and quality. The Journal of clinical investigation, 107(7), 899-907. Available at: https://doi.org/10.1172/JCI10347 ↑9 Francès, M. P., Vila-Vecilla, L., Russo, V., Caetano Polonini, H., & de Souza, G. T. (2024). Utilising SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia Treatment. Dermatology and Therapy, 14(4), 971-981. Available at: https://doi.org/10.1007/s13555-024-01142-y ↑10 Michel, L., Reygagne, P., Benech, P., Jean‐Louis, F., Scalvino, S., Ly Ka So, S., Hamidou, Z., Bianovici, S., Pouch, J., Ducos, B. and Bonnet, M., 2017. Study of gene expression alteration in male androgenetic alopecia: evidence of predominant molecular signalling pathways. British Journal of Dermatology, 177(5), 1322-1336. Available at: https://doi.org/10.1111/bjd.15577 Angiotensin-converting enzyme facilitates the conversion of angiotensin I to angiotensin II. This, alongside the degradation of bradykinin, leads to vasoconstriction (the tightening of blood vessels). As hair follicles require an adequate supply of blood for growth and health, it is thought that increased ACE activity can contribute to hair loss. In this article, we will explore the evidence (or lack thereof) linking ACE to hair loss and whether targeting changes in medication to single nucleotide polymorphisms (SNPs) in the ACE gene can improve hair growth outcomes.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is ACE?
Angiotensin-converting enzyme (ACE) is an enzyme that catalyzes the conversion of angiotensin I to angiotensin II (as well as degrading bradykinin), which are important factors in the regulation of blood pressure.[1]Wong, M. K. S. (2016). Angiotensin Converting Enzymes. In Handbook of Hormones. pp. 263-e29D-4. Elsevier. Available at: https://doi.org/10.1016/B978-0-12-801028-0.00254-3 Angiotensin II is known as a vasoconstrictor – i.e., it constricts blood vessels, reducing blood flow. Some research has implicated ACE activity and its gene polymorphisms have been associated with increased susceptibility to androgenic alopecia (AGA), and to the pathogenesis of alopecia areata.[2]Ibrahim, M.A., Ezzat, I.S., Mostafa, G.Y., Fathy, A.H.N., Eman, F., Samir, E.S.O. (2021). Association between angiotensin-converting enzyme gene insertion-deletion polymorphism and androgenetic … Continue reading,[3]Fahim, S., Montazer, F., Tohidinik, H.R., Naraghi, Z.S., Abedini, R., Nasimi, M., Ghandi, N. (2019). Serum and tissue angiotensin-converting enzyme in patients with alopecia areata. Indian Journal … Continue reading
Can Targeting ACE Help Hair Loss?
Insertion or deletion changes in the ACE gene can affect its activity, with the insertion typically leading to reduced ACE activity and the deletion leading to increased ACE activity (and, therefore, increased vasoconstriction).
Characterizing single nucleotide polymorphisms (SNPs) in the ACE gene may help predict responses to treatments that can affect blood flow, such as minoxidil or caffeine.Evidence Supporting Targeting ACE Polymorphisms For Hair Loss
ACE plays a key role in regulating blood pressure, converting angiotensin I to angiotensin II, and constricting blood vessels. Research in androgenic alopecia (AGA) indicates that the insertion/deletion gene mutation in the ACE gene is associated with increased susceptibility to AGA. The researchers found that the deletion/deletion and insertion/deletion genotypes were more frequently found in AGA patients, suggesting a genetic predisposition linked to ACE activity.[4]Mustafa, A.I., Ibrahim, S.E., Gohary, Y.M., Al-Husseini, N.F., Fawzy, E., El-Shimi, O.S. (2022). Association between angiotensin-converting enzyme gene insertion-deletion polymorphism and … Continue reading
Figure 1: Comparison between AGA patients and controls regarding ACE genotypes. The insertion/deletion (ID) and deletion/deletion (DD) genotypes were significantly increased in AGA patients compared to controls.[5]Ibrahim, M.A., Ezzat, I.S., Mostafa, G.Y., Fathy, A.H.N., Eman, F., Samir, E.S.O. (2021). Association between angiotensin-converting enzyme gene insertion-deletion polymorphism and androgenetic … Continue reading
Another study also found a link between ACE activity and the pathogenesis of alopecia areata (AA). In a study conducted on 49 people (25 with alopecia areata and 24 controls), researchers found no significant difference in serum ace activity but a significantly lower ace activity in the tissue. Furthermore, among patients with alopecia areata, higher ACE activity was associated with more severe disease and non-patchy alopecia areata.[6]Fahim, S., Montazer, F., Tohidinik, H.R., Naraghi, Z.S., Abedini, R., Nasimi, M., Ghandi, N. (2019). Serum and tissue angiotensin-converting enzyme in patients with alopecia areata. Indian Journal … Continue reading
While there appears to be a link between ACE and AGA, and AA, there are no studies linking ACE activity or gene polymorphisms to treatment efficacy in hair loss. Some genetic testing companies, however, believe that if you have the deletion polymorphisms of rs4343 or rs4341, you may want to try treatments that improve blood flow to the scalp.
The single nucleotide polymorphisms (SNP) rs4343 and rs4341 are variations in the ACE gene, part of the renin-angiotensin system (RAS). The RAS plays an important role in blood pressure regulation and fluid balance.
The G allele of rs4343 corresponds to the deletion allele of the ACE gene, which has been associated with higher ACE activity.[7]Tsantes, A.E., Kopterides, P., Bonovas, S., Bagos, P., Antonakos, G., Nikolopoulos, G.K., Gialeraki, A., Kapsimali, V., Kyriakou, E., Kokori, S., Dima, K., Armagandis, A., Tsangaris, I. (2013).Effect … Continue readingHigher ACE levels lead to increased production of angiotensin II, which leads to vasoconstriction. Some think that hair loss treatments (such as caffeine or minoxidil), which are thought to work at least in part through vasodilation, might improve hair loss outcomes.
Evidence Against Targeting ACE Polymorphisms For Hair Loss
While it is thought that minoxidil works by increasing blood flow to the hair follicle, no literature suggests that people with particular ACE polymorphisms will respond differently to hair treatments that may improve blood flow, such as caffeine or minoxidil.
Your Genetic Results
Your Result ACE (rs4343)
Variant 1 – AA genotype (insertion/insertion) Variant 2 – AG genotype (insertion/deletion) Variant 3 – GG genotype (deletion/deletion) What it means May have no abnormal vasoconstriction due to normal ACE activity May have moderately elevated vasoconstriction in the scalp due to a slight increase in ACE activity May have elevated vasoconstriction in the scalp due to increased ACE activity The Implication May not benefit from treatments that target blood flow, such as minoxidil or caffeine May want to try managing hair loss with treatments targeting blood flow, such as minoxidil or caffeine May want to try managing hair loss with treatments targeting blood flow, such as minoxidil or caffeine Your Result
ACE (rs4341)
Variant 1 – CC genotype Variant 2 – CG genotype Variant 3 – GG genotype What it means May have no abnormal vasoconstriction due to normal ACE activity May have moderately elevated vasoconstriction in the scalp due to a slight increase in ACE activity May have elevated vasoconstriction in the scalp due to increased ACE activity The Implication May not benefit from treatments that target blood flow, such as minoxidil or caffeine May want to try managing hair loss with treatments targeting blood flow, such as minoxidil or caffeine May want to try managing hair loss with treatments targeting blood flow, such as minoxidil or caffeine Treatment Relevance
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
- Does this gene have any potential relevance for hair loss? (1 point)
There is no evidence to support its significance in hair loss treatments (score=0)
-
- Does the totality of evidence implicate ACE as a causal agent for hair loss? (1 point)
No, there is no published evidence to suggest that ACE polymorphisms can cause hair loss (score = 0)
- Does the totality of evidence implicate ACE as a predictive factor for hair loss treatment responsiveness? (2 points)
No, there is no data to suggest that ACE polymorphisms can be used as a predictor for hair loss treatment responsiveness (score = 0)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
Since ACE fails question #3, it cannot be awarded points for question #4 (score = 0)
Total Score = 0
Final Thoughts
ACE is essential in maintaining circulation throughout the body and may play some role in the pathogenesis of AGA. However, no evidence supports targeting it as a predictor of treatment efficacy.
References[+]
References ↑1 Wong, M. K. S. (2016). Angiotensin Converting Enzymes. In Handbook of Hormones. pp. 263-e29D-4. Elsevier. Available at: https://doi.org/10.1016/B978-0-12-801028-0.00254-3 ↑2 Ibrahim, M.A., Ezzat, I.S., Mostafa, G.Y., Fathy, A.H.N., Eman, F., Samir, E.S.O. (2021). Association between angiotensin-converting enzyme gene insertion-deletion polymorphism and androgenetic alopecia susceptibility among Egyptian patients: A preliminary case-controlled study. Journal of Cosmetic Dermatology. 21(6). 2629-2634. Available at: https://doi.org/10.1111/jocd.14434 ↑3, ↑6 Fahim, S., Montazer, F., Tohidinik, H.R., Naraghi, Z.S., Abedini, R., Nasimi, M., Ghandi, N. (2019). Serum and tissue angiotensin-converting enzyme in patients with alopecia areata. Indian Journal of Dermatology, Venerology and Leprology. (85)3. 295-299 Available at: https://doi.org/10.4103/ijdvl.IJDVL_158_17. ↑4 Mustafa, A.I., Ibrahim, S.E., Gohary, Y.M., Al-Husseini, N.F., Fawzy, E., El-Shimi, O.S. (2022). Association between angiotensin-converting enzyme gene insertion-deletion polymorphism and androgenetic alopecia susceptibility among Egyptian patients: a preliminary case-controlled study. Journal of Cosmetic Dermatology. 21(60). 2629-2634. Available at: https://doi.org/10.1111/jocd ↑5 Ibrahim, M.A., Ezzat, I.S., Mostafa, G.Y., Fathy, A.H.N., Eman, F., Samir, E.S.O. (2021). Association between angiotensin-converting enzyme gene insertion-deletion polymorphism and androgenetic alopecia susceptibility among Egyptian patients: A preliminary case-controlled study. Journal of Cosmetic Dermatology. 21(6). 2629-2634. Available at: https://doi.org/10.1111/jocd.14434 ↑7 Tsantes, A.E., Kopterides, P., Bonovas, S., Bagos, P., Antonakos, G., Nikolopoulos, G.K., Gialeraki, A., Kapsimali, V., Kyriakou, E., Kokori, S., Dima, K., Armagandis, A., Tsangaris, I. (2013).Effect of angiotensin-converting enzyme gene I/D polymorphism and its expression on clinical outcome in acute respiratory distress syndrome. Minerva anestesiologica. 79(8). 861-870. Available at: PMID 23635999 The NR3C1 gene encodes the glucocorticoid receptor, which is essential for mediating the effects of glucocorticoids in various physiological processes, including metabolism, immune response, and stress regulation. This receptor plays a critical role in the body’s ability to respond to glucocorticoid medications, making it a key factor in conditions treated with these drugs.
This article will delve into the role of NR3C1 in glucocorticoid responsiveness and the evidence (or lack thereof) supporting it as a target for hair loss.
What is NR3C1?
The NR3C1 gene codes for the glucocorticoid receptor (GR). This receptor is involved in various physiological processes, including metabolism regulation, immune response, and stress response.[1]GeneCards. (no date). NR3C1 Gene – Nuclear Receptor Subfamily 3 Group C Member 1. GeneCards. Available at: … Continue reading. Glucocorticoids are a type of steroid used to treat inflammatory and autoimmune diseases as well as cancer.[2]Strehl, C., Ehlers, L., Gaber, T., Butthereit, F. (2019). Glucocorticoids – All Rounders Tackling the Versatile Players of the Immune System. Frontiers in Immunology. 10 GR is necessary for … Continue reading
All-Natural Hair Topical
The top natural ingredients for hair growth, all in one serum.
Take the next step in your hair growth journey with a world-class natural serum. Ingredients, doses, & concentrations built by science.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.
What is the Evidence for Targeting NR3C1 for Hair Loss?
GR is essential for glucocorticoids to exert their effects. There are two isoforms of GR encoded by the NR3C1 gene: GRα and GRβ. GRα is the classic GR protein, mediating the action of glucocorticoids.
GRβ contains a unique extra sequence that gives it several distinct properties: GRβ does not bind to activators of glucocorticoids, resides in the nucleus of the cells, and is by itself inactive. However, when expressed alongside GRα, GRβ inhibits the activity of GRα.[3]Oakley, R.H., Cidlowski, J.A. (2013). The Biology of the Glucocorticoid Receptor: New Signaling Mechanisms in Health and Disease. Journal of Allergy and Clinical Immunology. 132(5). 1033-1044. … Continue reading
Simply put, if GRꞵ binds to GRɑ, it stops it from working correctly. This can lead to reduced sensitivity or even resistance to glucocorticoids in tissues expressing GRβ at higher levels.
In one retrospective study involving 122 children with acute lymphoblastic leukemia, researchers found that a specific genetic variant, called rs6198, can affect how the body responds to glucocorticoid medications.[4]Gasic, V., Zukic, B., Stankovic, B., Janic, D., Dokmanovic, L., Lazic, J., Krstovski, N., Dolzan, V., Jazbec, J., Pavlovic, S., Kotur, N. (2018). Pharmacogenomic Markers of Glucocorticoid Response in … Continue reading
When a patient had the GG allele variant, it was found that it stabilized the messenger RNA (mRNA), which is the molecule that carries instructions from DNA to make proteins. This stabilization leads to more of a particular form of the glucocorticoid receptor, which doesn’t bind to the medication as well as the normal form.
Because this receptor doesn’t bind well, the treatment may not work as effectively, which could explain why some patients developed resistance to glucocorticoid therapy. This means their bodies don’t respond as well to the treatment, making it less effective in controlling their condition.
Figure 1: Genotype frequencies associated with glucocorticoid response. The bold numbers indicate a significant difference. NR3C1 6198 shows a significant association with glucocorticoid resistance.[5]Gasic, V., Zukic, B., Stankovic, B., Janic, D., Dokmanovic, L., Lazic, J., Krstovski, N., Dolzan, V., Jazbec, J., Pavlovic, S., Kotur, N. (2018). Pharmacogenomic Markers of Glucocorticoid Response in … Continue reading
What is the Evidence Against Targeting NR3C1 for Hair Loss?
Some companies that test your genotype to suggest treatments use this gene as a marker for glucocorticoid sensitivity. While the evidence suggests that variations of NR3C1 can negatively affect glucocorticoid receptor activity, there is no published evidence showing that there are subsequent effects on corticosteroid treatment responsiveness in hair.
What Do Your Genetic Results Mean?
Your Result NR3C1 (rs6198)
Variant 1 GG genotype
Variant 2 GA genotype Variant 3 AA genotype
What it means Increased expression of the GRβ isoform Moderate expression of the GRβ isoform Normal expression of GR and less expression of the GRβ isoform The Implication You may want to avoid glucocorticoid treatment You may respond less well to glucocorticoid treatment You may respond normally to glucocorticoid treatment What Relevance Does NR3C1 Have For Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes. Due to the inhibitory effect of GRβ on GR activity, this variation may affect response to glucocorticoid treatment in cases of hair loss. (score = 1)
- Does the totality of evidence implicate GRα as a causal agent for hair loss? (1 point)
No, there doesn’t appear to be any evidence implicating GRα in hair loss.
- Does the totality of evidence implicate GRα as a predictive factor for hair loss treatment responsiveness? (2 points)
While there is evidence to suggest that the activity of GRα may be affected by this variation, there is no published evidence to indicate that it can predict responsiveness to glucocorticoid treatment. (score = 0)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
No, the quality of evidence is not strong enough to influence treatment recommendations due to the lack of published evidence. (score = 0)
Total Score = 1
Final Thoughts
The NR3C1 gene, which encodes the glucocorticoid receptor, plays a crucial role in various physiological processes, including stress response and inflammation. While variations in the gene, particularly the rs6198 variant, have been linked to altered glucocorticoid sensitivity, the evidence for its role in hair loss remains inconclusive. Therefore, more research is needed to determine its relevance and utility in predicting or treating hair loss.
References[+]
References ↑1 GeneCards. (no date). NR3C1 Gene – Nuclear Receptor Subfamily 3 Group C Member 1. GeneCards. Available at: https://www.genecards.org/cgi-bin/carddisp.pl?gene=NR3C1#:~:text=This%20gene%20encodes%20glucocorticoid%20receptor,regulator%20of%20other%20transcription%20factors. (Accessed: July 2024) ↑2 Strehl, C., Ehlers, L., Gaber, T., Butthereit, F. (2019). Glucocorticoids – All Rounders Tackling the Versatile Players of the Immune System. Frontiers in Immunology. 10 GR is necessary for glucocorticoids to bind to and exert their biological effects. 10. 1-20. Available at: https://doi.org/10.3389/fimmu.2019.01744 ↑3 Oakley, R.H., Cidlowski, J.A. (2013). The Biology of the Glucocorticoid Receptor: New Signaling Mechanisms in Health and Disease. Journal of Allergy and Clinical Immunology. 132(5). 1033-1044. Available at: https://doi.org/10.1016/j.jaci.2013.09.007 ↑4 Gasic, V., Zukic, B., Stankovic, B., Janic, D., Dokmanovic, L., Lazic, J., Krstovski, N., Dolzan, V., Jazbec, J., Pavlovic, S., Kotur, N. (2018). Pharmacogenomic Markers of Glucocorticoid Response in The Initial Phase of Remission Induction Therapy in Childhood Acute Lymphoblastic Leukemia. Radiology and Oncology. 52(3). 296-306. Available at: https://doi.org/10.2478/raon-2018-0034 ↑5 Gasic, V., Zukic, B., Stankovic, B., Janic, D., Dokmanovic, L., Lazic, J., Krstovski, N., Dolzan, V., Jazbec, J., Pavlovic, S., Kotur, N. (2018). Pharmacogenomic Markers of Glucocorticoid Response in The Initial Phase of Remission Induction Therapy in Childhood Acute Lymphoblastic Leukemia. Radiology and Oncology. 52(3). 296-306. Available at: https://doi.org/10.2478/raon-2018-0034 The PGFTR gene encodes the prostaglandin F2 alpha (PGF2α) receptor, a critical component in various physiological processes. PGFTR is particularly significant in the context of hair loss due to its involvement in hair follicle and melanocyte growth. Studies have shown that PGF2α and its analogs, such as latanoprost, can stimulate hair growth and treat eyelash and eyebrow growth issues like hypotrichosis.
This article will explore the importance of the PGFTR gene in hair loss, its potential as a therapeutic target, and how understanding your genetic makeup could inform more effective treatment decisions.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is PGTFR?
The PGTFR gene encodes the prostaglandin F2 alpha (PGF2α) receptor, which plays an important role in various physiological processes, including reproductive physiology, inflammation, and cancer progression.[1]Ricciotti, E., FitzGerald, G.A. (2011). Prostaglandins and Inflammation. Arteriosclerosis, Thrombosis, and Vascular Biology. 31(5). 986-1000. Available at: https://doi.org/10.1161/ATVBAHA.110.207449.
Studies have suggested that PGF2α and its analogs, like latanoprost, stimulate the hair follicle and melanocyte growth in mice.[2]Sasaki, S., Hozumi, Y., Kondo, S. (2005). Influence of Prostaglandin F2 alpha and its Analogues on Hair Regrowth and Follicular Melanogenesis in a Murine Model. Experimental Dermatology. 14(5). … Continue reading
Can Targeting PGTFR Help Hair Loss?
Latanoprost is an analog of PGF2α and is commonly used as a treatment for an eye condition called glaucoma. Some clinical studies looking at the responsiveness of patients to latanoprost have uncovered multiple gene variants that can either increase or decrease responsiveness to the drug.
One study involved 100 volunteers who applied latanoprost eye drops to one eye once daily for seven days. Intraocular pressure was measured at the beginning and end of the study.[3]Sakurai, M., Higashide, T., Takahashi, M., Sugiyama, K. (2007). Association between Genetic Polymorphisms of the Prostaglandin F2ɑ Receptor Gene and Response to Latanoprost. Ophthalmology. 114(6). … Continue reading
Two key single nucleotide polymorphisms (SNPs) in the PGTFR gene were found to be associated with response to latanoprost treatment. SNPs are single-base pair gene changes. These single changes can have varied effects, from dramatic impacts on gene function or protein structure to no noticeable effect at all.
The results showed that within the rs3753380 SNP, the CC genotype was associated with a greater response to latanoprost, and the CT and TT genotypes were significantly associated with a lesser response. The rs3766355 SNP also found specific genotypes associated with lower latanoprost response. The study also found that the C allele of rs3766355 and the T allele of rs3753380 were associated with lower transcriptional activity of PGTFR, which suggests that these alleles may lead to reduced expression of PGTFR, resulting in a decreased response to latanoprost.
Figure 1: Latanoprost responsiveness based on single nucleotide polymorphism.[4]Sakurai, M., Higashide, T., Takahashi, M., Sugiyama, K. (2007). Association between Genetic Polymorphisms of the Prostaglandin F2ɑ Receptor Gene and Response to Latanoprost. Ophthalmology. 114(6). … Continue reading
This has been repeated in several studies that have evaluated various SNPs associated with the PGTFR gene for latanoprost’s effectiveness in treating glaucoma.
No studies have demonstrated whether SNPs in the PGTFR gene affect treatment responsiveness in relation to hair loss; however, PGF2ɑ analogs have been shown to improve hair growth outcomes.One randomized, double-blind, placebo-controlled study involving 16 men with androgenic alopecia was conducted over 24 weeks. It found that daily application of latanoprost 0.1% significantly increased hair density compared to baseline and placebo-treated areas of the scalp, suggesting that latanoprost can stimulate hair growth.[5]Blume-Peytavi, U., Lonngors, S., Hillmann, K., Bartels, N.G. (2012). A Randomized, Double-Blind, Placebo-Controlled Pilot Study to Assess the Efficacy of a 24-Week Topical Treatment by Latanoprost … Continue reading
Figure 2: number and percentage of anagen and telogen hairs per cm2 at baseline and week 24.[6]Blume-Peytavi, U., Lonngors, S., Hillmann, K., Bartels, N.G. (2012). A Randomized, Double-Blind, Placebo-Controlled Pilot Study to Assess the Efficacy of a 24-Week Topical Treatment by Latanoprost … Continue reading
Furthermore, a recent paper explored the genetic factors associated with androgenic alopecia.[7]Frances, M.P., Vila-Vecilla, L., Russo, V., Polonini, H.C., de Souza, G.T. (2024). Utilizing SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia Treatment. … Continue reading The study analyzed data from 26,607 patients, examining 26 SNPs and their correlation with AGA diagnosis. Eight SNPs were found to show a statistically significant association with AGA, one of which was PTGFR (rs10782665). However, there was no correlation found between these SNPs and the severity of AGA.
While the studies above suggest an effect of PGTFR gene variants on latanoprost effectiveness, no studies have determined this in the context of hair growth.
What Do Your Genetic Results Mean?
Your Result PGTFR (rs10782665)
Variant 1 – TT genotype Variant 2 – GT genotype Variant 3 – GG genotype What it means Associated with a higher percentage of responders to latanoprost treatment Associated with a moderately higher percentage of responders to latanoprost treatment Associated with a higher percentage of non-responders to latanoprost treatment The Implication May benefit from latanoprost treatment May benefit from latanoprost treatment May benefit from treatments other than latanoprost Your Result PGTFR (rs6686438)
Variant 1 – TT genotype Variant 2 – GT genotype Variant 3 – GG genotype What it means Associated with a higher percentage of responders to latanoprost treatment Associated with a higher percentage of responders to latanoprost treatments Associated with a higher percentage of non-responders to latanoprost treatment The Implication May benefit from latanoprost treatment May benefit from latanoprost treatment May benefit from treatments other than latanoprost Your Result PGTFR (rs1328441)
Variant 1 – AA genotype Variant 2 – AG genotype Variant 3 – GG genotype What it means Associated with a higher percentage of responders to latanoprost treatment Not associated with either responsiveness or non-responsiveness to latanoprost Associated with a higher percentage of non-responders to latanoprost treatment The Implication May benefit from latanoprost treatment May benefit from latanoprost treatment May benefit from treatments other than latanoprost Treatment Relevance
We have created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
Does this gene have any potential relevance for hair loss? (1 point)
- Yes. Initial studies have indicated that latanoprost could work as a treatment for hair loss. (score = 1)
Does the totality of evidence implicate PGTFR as a causal agent for hair loss? (1 point)
- There is no literature to suggest that PGTFR is a causal agent for hair loss. (score = 0)
Does the totality of evidence implicate PGTFR as a predictive factor for hair loss treatment responsiveness? (2 points)
- Although some studies have shown that PGTFR gene variations can affect latanoprost treatment responsiveness for patients with glaucoma, this has not also been shown to be true in the hair follicle. (score = 0)
Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
- It may be worth trying or avoiding latanoprost treatments if you have certain gene variations. (score = 1)
Total Score = 2
Final Thoughts
While some small studies suggest that genetic variation in the PGTFR gene may influence responsiveness to treatments like latanoprost, the evidence is not yet strong enough to make definitive treatment recommendations based solely on genotype. Larger and more robust studies are needed to confirm the true predictive value of genetic testing for PGTFR in personalizing hair loss treatments. Understanding the genetic underpinnings of hair loss and treatment responsiveness could eventually lead to more effective and tailored therapeutic approaches, but current data is insufficient to guide clinical decisions at this time.
References[+]
References ↑1 Ricciotti, E., FitzGerald, G.A. (2011). Prostaglandins and Inflammation. Arteriosclerosis, Thrombosis, and Vascular Biology. 31(5). 986-1000. Available at: https://doi.org/10.1161/ATVBAHA.110.207449. ↑2 Sasaki, S., Hozumi, Y., Kondo, S. (2005). Influence of Prostaglandin F2 alpha and its Analogues on Hair Regrowth and Follicular Melanogenesis in a Murine Model. Experimental Dermatology. 14(5). 323-328. Available at: https://doi.org/10.1111/j.0906-6705.2005.00270.x. ↑3, ↑4 Sakurai, M., Higashide, T., Takahashi, M., Sugiyama, K. (2007). Association between Genetic Polymorphisms of the Prostaglandin F2ɑ Receptor Gene and Response to Latanoprost. Ophthalmology. 114(6). 1039-1045. Available at: https://doi.org/10.1016/j.ophtha.2007.03.025. ↑5, ↑6 Blume-Peytavi, U., Lonngors, S., Hillmann, K., Bartels, N.G. (2012). A Randomized, Double-Blind, Placebo-Controlled Pilot Study to Assess the Efficacy of a 24-Week Topical Treatment by Latanoprost 0.1% on Hair Growth and Pigmentation in Healthy Volunteers with Androgenetic Alopecia. Journal of the American Academy of Dermatology. 66(5). 797-800. Available at: https://doi.org/10.1016/j.jaad.2011.05.026. ↑7 Frances, M.P., Vila-Vecilla, L., Russo, V., Polonini, H.C., de Souza, G.T. (2024). Utilizing SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia Treatment. Dermatology and Therapy (Heidelb). 14(4). 971-981. Available at: https://doi.org/10.1007/s13555-024-01145-y The PTGES2 gene encodes the enzyme prostaglandin E synthase 2, which plays a crucial role in converting prostaglandin H2 to prostaglandin E2 (PGE2). This enzyme is significant in various physiological processes, including inflammation and hair growth. Notably, studies have identified higher levels of PGE2 in non-balding scalps compared to balding ones, highlighting the potential relevance of PTGES2 in hair loss.
This article will delve into the role of PTGES2 in hair loss, its potential as a therapeutic target, and how genetic insights can guide more personalized and effective treatments.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is PTGES2?
Prostaglandin E synthase 2 (PTGES2) gene encodes the enzyme prostaglandin E synthase 2. This enzyme catalyzes the conversion of prostaglandin H2 (PGH2) to prostaglandin E2 (PGE2). It is a key enzyme in the prostaglandin synthesis pathway and plays a crucial role in various physiological processes, including inflammation and hair growth.
The PTGES2 gene codes for the prostaglandin E synthase enzyme, which is a key element in the synthesis of PGE2. Studies on human scalp samples have found PGE2 to be more abundant in non-balding scalps compared to balding scalps.[1]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading
Can Targeting PTGES2 Help Hair Loss?
There is some evidence to suggest that PTGES2 might be worth targeting:
Elevated PGE2 levels in haired scalp
Multiple studies have consistently shown that PGE2 levels are diminished in balding scalp areas compared to haired areas. For instance, measurements in patients with AGA have shown that PGE2 and PGF2ɑ were significantly lower in bald areas, while PGD2 and prostacyclin were elevated.[2]Chovarda, E., Sotiriou, E., Lazaridoi, E., Vakirlis, E., Ioannides, D. (2021). The Role of Prostaglandins in Androgenetic Alopecia. International Journal of Dermatology. 60. 730-735. Available at: … Continue reading
Figure 1: Prostaglandin mean levels (ng/g tissue) in patients with AGA comparing bald areas with non-balding.[3]Chovarda, E., Sotiriou, E., Lazaridoi, E., Vakirlis, E., Ioannides, D. (2021). The Role of Prostaglandins in Androgenetic Alopecia. International Journal of Dermatology. 60. 730-735. Available at: … Continue reading
PTGES2 Expression in Androgenic Alopecia
A study on 16 Hispanic males with androgenic alopecia (AGA) found that PTGES2 expression was significantly increased in the balding scalp compared to 16 control participants. This overexpression of PTGES2 in early male pattern hair loss is hypothesized to be the body’s attempt to counteract hair loss.[4]Villareal-Villareal, C.D., Sinclair, R.D., Martinez-Jacobo, L., Garza-Rodriguez, V., Rodriguez-Leon, S.A., Lamadrid-Zertuche, A.C., Rodriguez-Gutierrez, R., Ortiz-Lopez, R., Rojas-Martinez, A., … Continue reading
Figure 2: Comparison of relative gene expression of PTGES in patients with AGA and control patients.[5]Villareal-Villareal, C.D., Sinclair, R.D., Martinez-Jacobo, L., Garza-Rodriguez, V., Rodriguez-Leon, S.A., Lamadrid-Zertuche, A.C., Rodriguez-Gutierrez, R., Ortiz-Lopez, R., Rojas-Martinez, A., … Continue reading
Furthermore, a recent study delved into the genetic factors associated with AGA. The researchers analyzed genetic data from 26,607 patients, focusing on 26 SNPS and their correlation with a diagnosis of AGA. Eight SNPs were found to show a statistically significant association with AGA, one of which was PTGES2 (rs13283456).[6]Frances, M.P., Vila-Vecilla, L., Russo, V., Polonini, H.C., de Souza, G.T. (2024). Utilizing SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia Treatment. … Continue reading However, it should be noted that no correlation was found between the SNP and AGA severity.
Moreover, the study does not mention the samples from which the genetic information was gained. Genetic analyses of human scalp hair follicles have found unique gene expression profiles not found in other tissues.[7]Wu, S., Yu, Y., Liu, C., Zhang, X., Zhu, P., Peng, Y., Yan, X., Li, Y., Hua, P., Li, Q., Wang, S., Zhang, L. (2022). Single-cell transcriptomics reveals lineage trajectory of human scalp hair … Continue reading So, PTGES2 gene expression may not have the same association in tissue taken from the scalp.
Therefore, while general genetic studies do provide insights, they should be approached with caution when extrapolating these findings to hair growth processes.
Some believe that this SNP could affect responsiveness to minoxidil when targeting a gene for treatment efficacy. One study conducted on human dermal papilla cells found that minoxidil increased PGE2 production.[8]Michelet, J.F., Commo, S., Billoni, N., Mahe, Y.F., Bernard, B.A. (1997). Activation of cytoprotective prostaglandin synthase-1 by minoxidil as a possible explanation for its hair growth-stimulating … Continue readingSo, if you have the gene variant leading to lower activity of PGE2 synthase, minoxidil may be more beneficial.
What Do Your Genetic Results Mean?
Your Result PTGES2 (rs13283456) Variant 1 – CC genotype Variant 2 – TT genotype Variant 3 – CT genotype What it means Normal enzymatic activity of PGE2 synthase Normal enzymatic activity of PGE2 synthase Lower enzymatic activity of PGE2 synthase The Implication Will not affect the efficacy of minoxidil Will not affect the efficacy of minoxidil May be more beneficial to use minoxidil as a treatment for hair loss What Relevance Does PTGES2 Have for Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes. Studies have found that PGE2 levels are elevated in scalps of patients with a normal amount of hair compared to those with hair loss. (score = 1)
- Does the totality of evidence implicate PTGES2 as a causal agent for hair loss? (1 point)
Whilst this may be a causal agent for hair loss, there doesn’t appear to be literature to support this yet. Furthermore, there have been no studies to determine if a lack of PGE2 leads to the development of hair loss disorders. (0 = score)
- Does the totality of evidence implicate PTGES2 as a predictive factor for hair loss treatment responsiveness? (2 points)
No, the studies show that the gene variant that leads to reduced PTGES2 activity does not have any predictive value in determining patient response to hair loss treatment. (0 = score)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
Since PTGES2 fails question #3, it cannot be awarded points for question #4 (score = 0)
Total Score = 1
Final Thoughts
The PTGES2 gene has shown potential in hair loss treatment. However, current evidence is not sufficient to make definitive treatment recommendations based on PTGES2 genotypes. Research indicates that PGE2 levels are higher in non-balding scalps, and PTGES2 expression is increased in balding areas. Yet, there is still no conclusive proof that PTGES2 is a causal factor in hair loss. Moreover, the genetic variant rs13283456 associated with PTGES2 does not appear to predict treatment responsiveness effectively. Further research is necessary to better understand the role of PTGES2 in hair growth and to determine its potential as a target for hair loss treatments.
References[+]
References ↑1 Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). Prostaglandin D2 Inhibits Hair Growth and is Elevated in Bald Scalp of Men with Androgenetic Alopecia. Science Translational Medicine. 4(126). 1-21. Available at: https://doi.org/10.1126/scitranslmed.3003122 ↑2, ↑3 Chovarda, E., Sotiriou, E., Lazaridoi, E., Vakirlis, E., Ioannides, D. (2021). The Role of Prostaglandins in Androgenetic Alopecia. International Journal of Dermatology. 60. 730-735. Available at: https://doi.org/10.1111/ijd.15378 ↑4, ↑5 Villareal-Villareal, C.D., Sinclair, R.D., Martinez-Jacobo, L., Garza-Rodriguez, V., Rodriguez-Leon, S.A., Lamadrid-Zertuche, A.C., Rodriguez-Gutierrez, R., Ortiz-Lopez, R., Rojas-Martinez, A., Ocampo-Candiani, J. (2019). Prostaglandins in androgenetic alopecia in 12 men and four female. Journal of the European Academy of Dermatology and Venereology. 33(5). E214-e215. Available at: https://doi.org/10.1111/jdv.15479 ↑6 Frances, M.P., Vila-Vecilla, L., Russo, V., Polonini, H.C., de Souza, G.T. (2024). Utilizing SNP Association Analysis as a Prospective Approach for Personalising Androgenetic Alopecia Treatment. Dermatology and Therapy (Heidelb). 14(4). 971-981. Available at: https://doi.org/10.1007/s13555-024-01145-y ↑7 Wu, S., Yu, Y., Liu, C., Zhang, X., Zhu, P., Peng, Y., Yan, X., Li, Y., Hua, P., Li, Q., Wang, S., Zhang, L. (2022). Single-cell transcriptomics reveals lineage trajectory of human scalp hair follicle and informs mechanisms of hair graying. Cell Discovery. 8(49). 1-20. Available at: https://doi.org/10.1038/s41421-022–00394-2 ↑8 Michelet, J.F., Commo, S., Billoni, N., Mahe, Y.F., Bernard, B.A. (1997). Activation of cytoprotective prostaglandin synthase-1 by minoxidil as a possible explanation for its hair growth-stimulating effect. Journal of Investigative Dermatology. 108(2). 205-209. Available at: https://doi.org/10.1111/1523-1747.ep12334249 SRD5A1 and SRD5A2 are both part of the SRD5A gene family, encoding type I and type II 5α-reductase, respectively. With regard to hair loss, 5α-reductase is a type of enzyme that catalyzes the conversion of testosterone into dihydrotestosterone (DHT). DHT is a driving factor in androgenic alopecia (AGA) and, as a result, 5α-reductase inhibitors are a primary treatment for AGA. A collection of studies have investigated genetic variation in SRD5A1 and SRD5A2, with the results suggesting that some variants may cause differential responses to treatment with 5α-reductase inhibitors. This article will explore how relevant SRD5A1 and SRD5A2 are to hair treatment effectiveness and how to interpret your genetic results to make the correct treatment choice.
Interested in Topical Dutasteride?
Hair gains bigger than finasteride? Dutasteride makes this possible, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Are the SR5DA Genes?
The Steroid 5α-Reductase (SRD5A) gene family is thought to be composed of up to five genes, the most prominent being SRD5A1, SRD5A2, and SRD5A3. Despite the name, only SRD5A1 and SRD5A2 exhibit strong 5α-reductase activity, meaning that they are highly efficient at converting testosterone to DHT.[1]Scaglione, A., Montemiglio, L.C., Parisi, G., Asteriti, I.A., Bruni, R., Cerutti, G., Testi, C., Savino, C., Mancia, F., Lavia, P. and Vallone, B. (2017). Subcellular localization of the five members … Continue reading
Both SRD5A1 and SRD5A2 are expressed throughout the body, but it is their expression in the scalp that is important for hair growth outcomes. Type I 5α-reductase (produced by SRD5A1) is only strongly expressed in the sebaceous glands, the part of the hair follicle that produces sebum and keeps the skin moisturized. In contrast, type II 5α-reductase (produced by SRD5A2) is primarily expressed in the infundibulum (upper portion), inner root sheath, and outer root sheath of the hair follicle, indicating that type I and type II 5α-reductase have distinct localization within the skin and hair follicle.[2]Bayne, Flanagan, Einstein, Ayala, Chang, Azzolina, Whiting, Mumford and Thiboutot. (1999). Immunohistochemical localization of types 1 and 2 5α‐reductase in human scalp. British Journal of … Continue reading
Although they do have other roles, the primary function of these enzymes is to convert testosterone into dihydrotestosterone (DHT). One of four androgens (steroid hormones), DHT is known to be a driving factor of androgenic alopecia (AGA) and is implicated in the miniaturization of hair follicles.[3]Marchetti, P.M. and Barth, J.H. (2013). Clinical biochemistry of dihydrotestosterone. Annals of Clinical Biochemistry, 50(2), 95-107. Available at: https://doi.org/10.1258/acb.2012.012159
Due to the aforementioned role of DHT, 5α-reductase is a key target when it comes to the treatment of AGA. Thus, one of the main classes of AGA and hair loss treatments is 5α-reductase inhibitors. These inhibitors work by targeting the 5α-reductase enzymes, reducing their levels in order to disrupt the conversion of testosterone to DHT. Finasteride is the only FDA-approved 5α-reductase inhibitor for the treatment of AGA, which inhibits type II 5α-reductase. Dutasteride, a dual-inhibitor of type I and type II 5α-reductase, is only FDA-approved for the treatment of an enlarged prostate but is also prescribed off-label for AGA.[4]Gupta, A.K., Bamimore, M.A., Wang, T. and Talukder, M. (2024). The impact of monotherapies for male androgenetic alopecia: A network meta‐analysis study. Journal of Cosmetic Dermatology. Available … Continue reading
Other 5α-reductase inhibitors exist, including naturally occurring substances such as saw palmetto and some green tea catechins, but they have varying levels of evidence quality.
What is The Evidence For Targeting SR5DA for Hair Loss?
So, SRD5A1 and SRD5A2 are closely linked to 5α-reductase activity, DHT production, and, therefore, AGA. Owing to this, it is feasible that genetic variation in either SRD5A1 or SRD5A2 could influence the efficacy of 5α-reductase inhibitors in the treatment of hair loss.
In one study, the genotypes of 42 males with AGA were investigated. They had been using dutasteride for 6 months in a clinical trial, which had produced variable results. For the purposes of this study, patients were put into the poor responder (control) group or the good responder (cases) group, based on their increase in hair count during the original study. In their investigation, they identified a number of genetic variants that were statistically significantly associated with the strength of the response to the treatment (Figure 1).[5]Rhie, A., Son, H.Y., Kwak, S.J., Lee, S., Kim, D.Y., Lew, B.L., Sim, W.Y., Seo, J.S., Kwon, O., Kim, J.I. and Jo, S.J. (2019). Genetic variations associated with response to dutasteride in the … Continue reading
Three of these were single nucleotide polymorphisms (SNPs) within the SRD5A1 gene – rs3822430, rs8192186, and rs3736316. Each of these SNPs was positively associated with the response to dutasteride; in other words, patients with these genetic variants responded better to dutasteride treatment.
Figure 1: Genotypic landscape of 42 patients and the cumulative effect of each allele count and their positive or negative effect. Boxes represent SNPs that exhibited a positive (blue) or negative (red) effect on dutasteride response. Light-colored boxes represent heterozygous SNPs (a variation where an individual has two different versions of a specific DNA sequence at a particular location in the genome), dark-colored boxes represent homozygous SNPs (a variation where an individual has two identical versions of a specific DNA sequence at a particular location in the genome). Patient responses to dutasteride improve from left to right.[6]Rhie, A., Son, H.Y., Kwak, S.J., Lee, S., Kim, D.Y., Lew, B.L., Sim, W.Y., Seo, J.S., Kwon, O., Kim, J.I. and Jo, S.J. (2019). Genetic variations associated with response to dutasteride in the … Continue reading
Despite the positive associations, some of the patients who possessed these SNPs were still considered to be poor responders. This suggests that having a ‘positive’ SNP in SRD5A1 does not provide a definitive indication that you will respond well to dutasteride. Rather, the study’s results suggest that the combination of SNPs you possess and how they interact with each other is more important.
Interestingly, SRD5A2 was not associated with the response to dutasteride in the same study and no other studies have investigated the effects of SRD5A2 variants on the efficacy of dutasteride or finasteride treatment for hair loss, but that does not mean there are no effects.
Genetic variation in the SRD5A gene family appears to influence the efficacy of dutasteride treatment, so the question then turns to why this might happen.
In a study conducted on 57 males with type II diabetes, an association was found between the SRD5A1 HinfI SNP and the DHT/testosterone ratio, which is used as an indicator of 5α-reductase enzyme activity.[7]Ellis, J.A., Panagiotopoulos, S., Akdeniz, A., Jerums, G. and Harrap, S.B. (2005). Androgenic correlates of genetic variation in the gene encoding 5α-reductase type 1. Journal of Human Genetics, … Continue reading
HinfI is an enzyme that binds to a specific series of bases (called a restriction site) and cuts the DNA. Any changes to that sequence of bases will prevent HinfI from cutting the DNA, so it can be used to identify SNPs within known restriction sites. Individuals who lacked the SRD5A1 HinfI restriction site had a higher ratio of DHT/testosterone ratio than those with other genotypes, indicating increased activity of 5α-reductase.
In patients with increased levels of DHT, due to genetic variation, treatment with 5α-reductase inhibitors may look different. Higher concentrations of 5α-reductase inhibitors may be necessary, and it might take longer to see results, but the treatment may also have a more noticeable effect on hair loss as DHT levels can be reduced more than normal.
Figure 2: Measurements of testosterone (T), DHT, sex hormone binding globulin (SHBG), and insulin in participants with different genotypes (AA, AB, BB). A=absence of restriction site. Presence of the restriction site. Those lacking the restriction site (AA) had a higher DHT/T ratio meaning increased 5a-reductase activity.[8]Ellis, J.A., Panagiotopoulos, S., Akdeniz, A., Jerums, G. and Harrap, S.B. (2005). Androgenic correlates of genetic variation in the gene encoding 5α-reductase type 1. Journal of Human Genetics, … Continue reading
A different study was conducted on 104 patients with metastatic prostate cancer, investigating SNPs in SRD5A1 and SRD5A2. The authors discovered that patients with the GG genotype in SRD5A2 rs523349 exhibited increased 5α-reductase enzyme activity than those with the GC or CC genotype. #
The patients did not have their DHT levels measured, however, it is possible that increased 5α-reductase enzyme activity would lead to increased levels of DHT, which might make patients with the GG genotype a better candidate for treatment with a 5α-reductase inhibitor.[9]Shiota, M., Fujimoto, N., Yokomizo, A., Takeuchi, A., Itsumi, M., Inokuchi, J., Tatsugami, K., Uchiumi, T. and Naito, S. (2015). SRD5A gene polymorphism in Japanese men predicts prognosis of … Continue reading
These findings were supported by another study, which investigated several genetic variants of the SRD5A2 gene in healthy men. The authors found that, although the expression levels of the type II 5α-reductase enzyme were similar throughout, some of the variants produced type II 5α-reductase with very different properties to the normal (wild-type) enzyme.[10]Makridakis, N.M., di Salle, E. and Reichardt, J.K. (2000). Biochemical and pharmacogenetic dissection of human steroid 5α-reductase type II. Pharmacogenetics and Genomics, 10(5), 407-413. Available … Continue reading
Importantly, the activity of the enzyme (the speed at which it catalyzes reactions) was lower than normal in some variants and higher in others suggesting that DHT production may be lower in people with some SRD5A2 variants and higher in people with others. In contrast to those with higher levels, patients with lower DHT levels than normal may require a reduced dose of 5α-reductase inhibitor, and it is possible that treatment will be less efficient as DHT levels are already low. Or, other treatments that don’t primarily target DHT might be more appropriate.
To investigate this further, the authors produced lab-grown animal cells which contained each of the genetic variants. They then tested finasteride and dutasteride on all of the cells and measured 5α-reductase activity, to determine how efficiently the 5α-reductase inhibitors worked on each variant. They found that finasteride and dutasteride could be more, less, or equally effective as normal, depending on the variant(s).
Moreover, finasteride could be more effective than normal against a variant, while dutasteride was less effective than normal, and vice versa. This suggests that genetic variation could significantly affect the outcomes of treatment with finasteride or dutasteride.
Collectively, the results of these studies suggest that genetic variation in the SRD5A family of genes should be considered when designing treatment regimens for hair loss. However, the data is not without its limitations.
For the most part, studies conducted on SRD5A (including the ones here) have only included male participants. As males and females display differences in DHT expression, it would not be surprising if there were also differences in SRD5A gene expression and 5α-reductase inhibitor activity.
Furthermore, these studies were only conducted on a small number of participants. This reduces the power of a study, as you may not have an accurate representation of the wider population, and it can lead to results being misleading. Repeating the study on a much larger scale would produce more conclusive results. Also, some of the studies were not conducted on patients with AGA or hair loss-related conditions, so the findings are not directly relevant to hair loss treatment.
The final study, which investigated 5α-reductase inhibitor activity on each variant, was performed in vitro. In other words, it was performed on cells that had been genetically modified to express each variant. Furthermore, these cells were not even human cells found in the scalp or hair follicle, but rather animal cells.
Although models such as this can be very useful, the results they produce are not definitive, as the model (cells, in this case) is not a true representation of human anatomy.
Despite these limitations, there is sufficient evidence to suggest that genetic variation in SRD5A1 or SRD5A2 may influence your response to treatment with a 5α-reductase inhibitor. Below are some of the variants which may be relevant to hair loss and treatment.
What Do Your Genetic Results Mean?
Your Result
SRD5A1 (rs248793)
Variant 1 – GG genotype
Variant 2 – CC genotype Variant 3 – GC genotype
What it means At a lower risk of presenting with higher DHT/T ratio At a slightly higher risk of presenting with an increased DHT/T ratio At a higher risk of presenting with a significant increase in DHT/T ratio The Implication You might not be a good candidate for 5α-reductase inhibitors May be a good candidate for normal/increased concentrations of 5α-reductase inhibitors May be a good candidate for increased concentrations of 5α-reductase inhibitors Your Result SRD5A1 (rs3822430)
Variant 1 – AA genotype
Variant 2 – AG genotype Variant 3 – GG genotype
What it means May be a normal/poor responder to 5α-reductase inhibitors May be a good responder to 5α-reductase inhibitors May be a good responder to 5α-reductase inhibitors The Implication May be a good candidate for typical/higher dosages of 5α-reductase inhibitors May be a good candidate for lower dosages of 5α-reductase inhibitors May be a good candidate for lower dosages of 5α-reductase inhibitors Your Result SRD5A1 (rs8192186)
Variant 1 – AA genotype
Variant 2 – AG genotype Variant 3 – GG genotype
What it means May be a good responder to 5α-reductase inhibitors May be a good responder to 5α-reductase inhibitors May be a normal/poor responder to 5α-reductase inhibitors The Implication May be a good candidate for lower dosages of 5α-reductase inhibitors May be a good candidate for lower dosages of 5α-reductase inhibitors May be a good candidate for typical/higher dosages of 5α-reductase inhibitors Your Result SRD5A2 (rs523349)
Variant 1 – GG genotype
Variant 2 – GC genotype Variant 3 – CC genotype
What it means Associated with increased 5α-reductase activity Significantly lower 5α-reductase activity Significantly lower 5α-reductase activity The Implication May be a good candidate for 5α-reductase inhibitors May not be a good candidate for 5α-reductase inhibitors May not be a good candidate for 5α-reductase inhibitors What Relevance Dose SR5DA Have for Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
On a scale of 1-5, how important are these genetic results? (1 is the lowest, 5 is the highest)
This score is a rating based on evidence quality.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes. Increased DHT is associated with hair follicle miniaturization and the onset of androgenic alopecia, and these genes encode enzymes that synthesize DHT (score=1)
- Does the totality of evidence implicate SRD5A1 or SRD5A2 as causal agents for hair loss? (1 point)
Yes, as mentioned above, an increase in DHT is associated with androgenic alopecia, and these genes create an enzyme that synthesizes DHT (score = 1)
- Does the totality of evidence implicate SRD5A1/SRD5A2 as predictive factors for hair loss treatment responsiveness? (2 points)
Yes, there is evidence to suggest that SRD5A1 may be a predictive factor for hair loss treatment responsiveness, however, some of the patients with the SNP’s for treatment responsiveness still performed poorly, indicating that there are a number of factors involved in responsiveness to treatments. (score = 1)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
No. (score = 0)
Total Score = 3
Final Thoughts
While some small studies suggest that genetic variation in SRD5A1 and SRD5A2 may influence your response to treatment with a 5α-reductase inhibitor, the evidence is not yet strong enough to make definitive treatment recommendations based solely on genotype. Larger and more robust studies are needed to confirm the true predictive value of genetic testing for SRD5A1 and SRD5A2 for personalizing hair loss treatments.
References[+]
References ↑1 Scaglione, A., Montemiglio, L.C., Parisi, G., Asteriti, I.A., Bruni, R., Cerutti, G., Testi, C., Savino, C., Mancia, F., Lavia, P. and Vallone, B. (2017). Subcellular localization of the five members of the human steroid 5α-reductase family. Biochimie open, 4, 99-106. Available at: https://doi.org/10.1016/j.biopen.2017.03.003 ↑2 Bayne, Flanagan, Einstein, Ayala, Chang, Azzolina, Whiting, Mumford and Thiboutot. (1999). Immunohistochemical localization of types 1 and 2 5α‐reductase in human scalp. British Journal of Dermatology, 141(3), 481-491. Available at: https://doi.org/10.1046/j.1365-2133.1999.03042.x ↑3 Marchetti, P.M. and Barth, J.H. (2013). Clinical biochemistry of dihydrotestosterone. Annals of Clinical Biochemistry, 50(2), 95-107. Available at: https://doi.org/10.1258/acb.2012.012159 ↑4 Gupta, A.K., Bamimore, M.A., Wang, T. and Talukder, M. (2024). The impact of monotherapies for male androgenetic alopecia: A network meta‐analysis study. Journal of Cosmetic Dermatology. Available at: https://doi.org/10.1111/jocd.16362 ↑5, ↑6 Rhie, A., Son, H.Y., Kwak, S.J., Lee, S., Kim, D.Y., Lew, B.L., Sim, W.Y., Seo, J.S., Kwon, O., Kim, J.I. and Jo, S.J. (2019). Genetic variations associated with response to dutasteride in the treatment of male subjects with androgenetic alopecia. Plos one, 14(9), e0222533. Available at: https://doi.org/10.1371/journal.pone.0222533 ↑7, ↑8 Ellis, J.A., Panagiotopoulos, S., Akdeniz, A., Jerums, G. and Harrap, S.B. (2005). Androgenic correlates of genetic variation in the gene encoding 5α-reductase type 1. Journal of Human Genetics, 50(10), 534-537. Available at: https://doi.org/10.1007/s10038-005-0289-x ↑9 Shiota, M., Fujimoto, N., Yokomizo, A., Takeuchi, A., Itsumi, M., Inokuchi, J., Tatsugami, K., Uchiumi, T. and Naito, S. (2015). SRD5A gene polymorphism in Japanese men predicts prognosis of metastatic prostate cancer with androgen deprivation therapy. European Journal of Cancer, 51(14), 1962-1969. Available at: https://doi.org/10.1016/j.ejca.2015.06.122 ↑10 Makridakis, N.M., di Salle, E. and Reichardt, J.K. (2000). Biochemical and pharmacogenetic dissection of human steroid 5α-reductase type II. Pharmacogenetics and Genomics, 10(5), 407-413. Available at: https://doi.org/10.1097/00008571-200007000-00004 SULT1A1 is a gene that encodes for sulfotransferase, an enzyme that catalyzes various reactions throughout the body. Regarding hair loss, sulfotransferase is crucial for activating minoxidil, which requires sulfonation to exert its effects.
Some studies suggest that measuring sulfotransferase levels may be possible to predict whether minoxidil will be effective. Others have claimed that the expression of a specific variant of the SULT1A1 gene can indicate whether the drug is likely to work.
This article will explore how relevant SULT1A1 is to hair treatment effectiveness and how to interpret your genetic results to make the correct treatment choice.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is SULT1A1?
The SULT1A1 gene codes for an enzyme called sulfotransferase 1A1 (SULTS). The SULT family of enzymes catalyzes the transfer of a sulfonate (SO3-) group from the universal donor 3’-phosphoadenosine 5’-phosphosulfate (PAPS) to an acceptor molecule. This reaction is known as sulfation or sulfurylation.[1]Negishi, M., Pederson, L.G., Petrochenko, E., Shevtsov, S., Gorokhov, A., Kakuta, Y., Pederson, L.C. (2001). Structure and function of sulfotransferases. Archives of biochemistry and biophysics. … Continue reading
These reactions play a crucial role in the metabolism and detoxification of various compounds, including hormones, neurotransmitters, and drugs (including minoxidil which we will get to), increasing their water solubility and facilitating their elimination.[2]Gamage, N., Barnett, A., Hempel, N., Duggleby, R.G., Windmill, K.F., Martin, J.L., McManus, M.E. (2006). Human Sulfotransferases and Their Role in Chemical Metabolism. Toxicological Sciences. 90(1). … Continue reading
The SULT1 family in humans consists of at least nine members, including SULT1A1, SULT1A2, SULT1A3, SULT1A4, SULT1B1, SULT1C2, SULT1C3, SULT1C4, and SULT1E1. Genetic variations in SULT1A1 can influence enzyme activity and have been associated with differences in drug response, toxicity, and disease susceptibility.[3]National Library of Medicine. (2024). SULT1A1 sulfotransferase family 1A member 1 [Homo sapiens (human)]. NIH. Available at: … Continue reading
Some studies have found different variants of the SULT1A1 gene, which are associated with different activity levels. The GG variant was associated with high activity, whereas GA and AA variants were associated with low activity.[4]Ramos, P.M., Gohad, P., McCoy, J., Wambier, C., Goren, A. (2021). Minoxidil Sulfotransferase Enzyme (SULT1A1) Genetic Variants Predicts Response to Oral Minoxidil Treatment for Female Pattern Hair … Continue reading
So, we know what SULT1A1 is and about the enzyme it codes for. But how relevant is it to hair loss outcomes?
What is the Evidence For Targeting SULT1A1 for Hair Loss?
One crucial piece of evidence for targeting SULT1A1 for hair loss is the link between sulfotransferase and minoxidil. SULT1A1 codes for the sulfotransferase enzyme that catalyzes the conversion of minoxidil (a prodrug that needs activation to exert its effect) to minoxidil sulfate (the activated form of the drug). As such, some studies have evaluated the correlation between minoxidil efficacy and sulfotransferase activity.
One study was conducted with 34 patients who had been treated with minoxidil alone for a minimum of 6 months.[5]Goren, A., Castano, J.A., McCoy, J., Bermudez, F., Lotti, T. (2014). Novel enzymatic assay predicts minoxidil response in the treatment of androgenetic alopecia. Dermatologic Therapy. 27. 171-173. … Continue reading These patients were evaluated as “responders” or “non-responders” based on global photographic assessment. Hairs in the growing (anagen phase) were plucked from the border between bald and non-bald scalp areas and evaluated for sulfotransferase activity. Each patient’s sulfotransferase activity was measured and compared to their “responder” or “non-responder” status. The researchers found that most “responders” had a higher sulfotransferase activity, whereas most “non-responders” had a lower sulfotransferase activity.
Figure 1. Sulfotransferase activity compared to “responder or non-responder status”.[6]Goren, A., Castano, J.A., McCoy, J., Bermudez, F., Lotti, T. (2014). Novel enzymatic assay predicts minoxidil response in the treatment of androgenetic alopecia. Dermatologic Therapy. 27. 171-173. … Continue reading
Another study of the same group also measured sulfotransferase activity in 21 women with female pattern hair loss who had been treated with 5% minoxidil for a minimum of 6 months.[7]Roberts, J., Desai, N., McCoy, J., Goren, A. (2014). Sulfotransferase activity in plucked hair follicles predicts response to topical minoxidil in the treatment of female androgenetic alopecia. … Continue reading Fifteen “responders” and 6 “non-responders” were identified, with only two not correctly identified after the assay.
Why Do Some People Have Lower SULT1A1 Activity Levels Than Others?
Well, the SULT1A1*2 variant of the SULT1A is associated with low enzyme activity and thermal stability of SULT1A1.[8]Raftogianis, R.B., Wood, T.C., Otterness, D.M., Loon, J.A.V., Weinshilboum, R.M. (1997). Phenol Sulfotransferase Pharmacogenetics in Humans: Association of Common SULT1A1 Alleles with TS PST … Continue reading Therefore, it can be reasonably inferred that those with lower sulfotransferase activity might have this gene variant and, therefore, be less responsive to minoxidil.
SULT1A1 Gene Variants & Minoxidil: Clinical Studies
There are two studies that explore different gene variants of SULT1A1 and their effect on minoxidil efficacy.
In the first study, 17 males and 18 females with androgenic alopecia were included.[9]Raghad, N.A., Al-Gazally, M.E., Ewahd, W.A. (2017). Assessment the effect of different genotypes of sulfotransferase 1A1 gene on the response to minoxidil in patients with androgenic alopecia. … Continue reading The participants had been using topical minoxidil for at least 3 months before being assessed for response and allocated into “responder” and “non-responder” groups. The participants were then genotyped to determine what allele variant was present in the SULT1A1 gene and compared.
84% of participants who carried the G allele of the SULT1A1 gene were in the “responder” group, compared to only 16% of those with the A allele.
Figure 2. The proportion of participants in the R0 (“non-responder”) and R1 (“responder”) groups with each allele variation.[10]Raghad, N.A., Al-Gazally, M.E., Ewahd, W.A. (2017). Assessment the effect of different genotypes of sulfotransferase 1A1 gene on the response to minoxidil in patients with androgenic alopecia. … Continue reading
Furthermore, of those carrying the GG variant, 68.8% were “responders” compared to 15.8% who were “non-responders”. Conversely, 84.2% of “non-responders” had the GA genotype compared to 31.2% of “responders”.
Figure 3. The proportion of participants in the R0 (“non-responder”) and R1 (“responder”) groups with each genotype variation.[11]Raghad, N.A., Al-Gazally, M.E., Ewahd, W.A. (2017). Assessment the effect of different genotypes of sulfotransferase 1A1 gene on the response to minoxidil in patients with androgenic alopecia. … Continue reading
Interestingly, a higher proportion of “responders” were female (25.7%), indicating a potential for women to respond better to minoxidil (possibly due to more women having the GG allele variation) – however, this would need to be confirmed in further studies.
Figure 4. Red: Proportion of males and females in the “responder” group (R1). Blue: Proportion of males and females in the “non-responder” group (R0).[12]Raghad, N.A., Al-Gazally, M.E., Ewahd, W.A. (2017). Assessment the effect of different genotypes of sulfotransferase 1A1 gene on the response to minoxidil in patients with androgenic alopecia. … Continue reading
A further study was conducted in 2020 in which 10 participants with female pattern hair loss were treated with 1 mg oral minoxidil daily for six months.[13]Ramos, P.M., Gohad, P., McCoy, J., Wambier, C., Goren, A. (2021). Minoxidil Sulfotransferase Enzyme (SULT1A1) genetic variants predict response to oral minoxidil treatment for female pattern hair … Continue reading Hairs were counted within a 2.2 cm2 area, with a minimum 13% increase in hair count considered as a “responder”. Genotyping was conducted alongside this. Participants with the GG allele variant showed a 13.3% average increase in hair count, while participants with the GA allele variant showed a 6.9% average increase.
The researchers concluded that this gene variant can predict response to oral minoxidil treatment, but we see some issues. There are clearly some are some exceptions to the rule (which you can see below).
One person with the GA allele variant showed a 21.8% increase in hair which is a larger increase than nearly all of the GG allele variants! Furthermore, three of the GG variants did not reach the minimum 13% increase in hair count to actually be labeled a “responder”.
Figure 5. Effect of allele variants on hair follicle growth.[14]Ramos, P.M., Gohad, P., McCoy, J., Wambier, C., Goren, A. (2021). Minoxidil Sulfotransferase Enzyme (SULT1A1) genetic variants predict response to oral minoxidil treatment for female pattern hair … Continue reading
To confirm whether the variants actually affect response rates to minoxidil treatment, larger-scale studies are needed.
Can I Get Better Results with Oral Minoxidil?
On the internet, some individuals have mentioned that if you have a variant of SULT1A1, that means you’re less likely to respond to topical minoxidil, then you should take low-dose oral minoxidil. This is because the liver has abundant sulfotransferase activity which can also convert oral minoxidil to its active form. This active form could then circulate through the bloodstream to the scalp and exert its effects that way.
But is this true?
Well, it is true that the liver has high sulfotransferase activity. This suggests that individuals with low sulfotransferase activity in their hair follicles (due to SULT1A1 gene variants) might still benefit from oral minoxidil. However, as you can see above, studies have shown mixed results regarding the efficacy of oral minoxidil in “non-responders”.
Would Switching From Topical to Oral Help?
Switching to oral minoxidil may help some who don’t respond to topical minoxidil. One study by Ramos et al. found that in their study population of female patients, oral minoxidil slightly outperformed topical minoxidil in improving hair density and reducing shedding over 24 weeks.[15]Ramos, P.M., Sinclair, R.D., Kasprzak, M., Miot, H.A. (2020). Minoxidil 1 mg oral versus minoxidil 5% topical solution for the treatment of female-pattern hair loss: a randomized clinical … Continue reading
Another study, however, found that although topical minoxidil had a better overall effect than 1 mg oral minoxidil, there was no significant difference between the two groups, indicating that switching might actually just lead to the same response.[16]Asilian, A., Farmani, A., Saber, M. (2023). Clinical efficacy and safety of low-dose oral minoxidil versus topical solution in the improvement of androgenetic alopecia: a randomized controlled … Continue reading
Will Switching Make a Difference?
Not necessarily. It looks like the effectiveness of oral minoxidil can still be influenced by the same genetic factors that affect topical minoxidil response. Additionally, oral minoxidil carried potential safety risks, as it is not FDA-approved for hair loss and may have systemic side effects that need to be carefully managed.
In recent years, genetic testing companies have sprung up that claim to analyze your genotype to help you choose a personalized hair loss treatment. However, concerns remain about the accuracy of their recommendations, privacy issues regarding genetic data, and the potential for overpromising results without comprehensive clinical validation.
These companies often include the SULT1A1 gene as a predictor of responsiveness to minoxidil. So, we collated all of the potential SULT1A1 gene variants that might be relevant to hair loss and recommendations, depending on your genotype.
SULT1A1 genetic variants play a significant role in predicting the effectiveness of minoxidil for hair loss treatment. While the enzyme’s activity in hair follicles can indicate responsiveness to topical minoxidil, switching to oral minoxidil may offer limited additional benefits due to similar genetic influences on enzyme activity. Enhancing sulfotransferase activity through methods like tretinoin application and microneedling has shown promise in improving treatment outcomes for non-responders.
What Do Your Genetic Results Mean?
There are a number of variants that your genetic testing results might tell you that you have. You can see the possible variants that might come up within your own gene testing and reference these tables once you get your results to find out what they mean.
Your Result SULT1A1-1 Variant 1 SULT1A1-1 Variant 2 SULT1A1-1 Variant 3 rs9282861 GG genotype rs9282861 GA genotype rs9282861 AA genotype What it Means High sulfotransferase activity Moderate sulfotransferase activity Low sulfotransferase activity The Implication May respond well to topical minoxidil. Recommend treatment. May respond normally to topical minoxidil. May not respond well to topical minoxidil. You may want to try oral minoxidil or an alternative treatment. Your Result SULT1A1-2 Variant 1 SULT1A1-2 Variant 2 SULT1A1-2 Variant 3 rs1042028 GG genotype rs1042028 GA genotype rs1042028 AA genotype What it Means High sulfotransferase activity Moderate sulfotransferase activity Low sulfotransferase activity and low thermal stability The Implication May respond well to topical minoxidil. Recommend treatment. May respond normally to topical minoxidil. May not respond well to topical minoxidil. You may want to try oral minoxidil or an alternative treatment. Your Result SULT1A1-3 Variant 1 SULT1A1-3 Variant 2 SULT1A1-3 Variant 3 rs1042157 TT genotype rs1042157 CT genotype rs1042157 CC genotype What it Means Low sulfotransferase activity. You may want to try oral minoxidil or an alternative treatment. Moderate sulfotransferase activity High sulfotransferase activity The Implication May not respond well to topical minoxidil. You may want to try oral minoxidil or an alternative treatment. May respond normally to topical minoxidil. May respond well to topical minoxidil. Recommend treatment. Your Result SULT1A1-4 Variant 1 SULT1A1-3 Variant 2 SULT1A1-4 Variant 3 rs6839 GG genotype rs6839 AG genotype rs6839 AA genotype What it Means Low sulfotransferase activity Moderate sulfotransferase activity High sulfotransferase activity The Implication May not respond well to topical minoxidil. You may want to try oral minoxidil or an alternative treatment. May respond normally to topical minoxidil. May respond well to topical minoxidil. Recommend treatment. Table 1: Different potential allele variants of the SULT1A1 gene and the implication in terms of hair treatments.
What Relevance Does SULT1A1 Have for Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes. Some studies have shown that people with variations in the SULT1A1 gene may respond differentially to minoxidil. (score = 1)
- Does the totality of evidence implicate SULT1A1 as a causal agent for hair loss? (1 point)
There is no evidence to suggest that SULT1A1 variations cause hair loss (score = 0)
- Does the totality of evidence implicate SULT1A1 as a predictive factor for hair loss treatment responsiveness? (2 points)
Yes. There are a number of studies implicating SULT1A1 as a predictive factor for minoxidil responsiveness. (score =2)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
No. One paper was published in a journal with a low/no impact factor. The sample sizes were small, and the results where genotyping was actually conducted were variable. (score= 0)
Total Score = 3
How Can I Improve My Sulfotransferase Activity?
So, you have tried minoxidil, but the regrowth hasn’t been as impactful as you hoped, and you find out that this is because your sulfotransferase levels are low. How can you boost it? Well, studies show that combining retinoic acid or tretinoin with minoxidil can increase sulfotransferase activity.
The topical application of tretinoin increases the expression and activity of follicular sulfotransferase enzymes. One study was conducted on 20 participants (10 males and 10 females) with androgenic alopecia.[17]Sharma, A., Goren, A., Dhurat, R., Agrawal, S., Sinclair, R., Trueb, R., Vano-Galvan, S., Chen, G., Tan, Y., Kovacevic, M., Situm, M., McCoy, J. (2019). Tretinoin enhances minoxidil response in … Continue reading
The participants’ hair follicles were analyzed using the Minoxidil Response Test and determined as “responders” or “non-responders” to minoxidil treatment. The participants then underwent 5 days of treatment with 0.1% topical tretinoin. The average sulfotransferase activity for the whole cohort did not significantly improve after the five days, however, when the cohort was separated into “responders” and “non-responders”, something interesting happened. Those predicted to be “non-responders” to topical minoxidil did show a significant increase in sulfotransferase activity, with a total of 43% of “non-responders” converted to “responders” after five days of application.
Figure 6. Sulfotransferase activity before and after five days of 0.1% topical tretinoin application. NR = Non-responder. R = Responder.[18]Sharma, A., Goren, A., Dhurat, R., Agrawal, S., Sinclair, R., Trueb, R., Vano-Galvan, S., Chen, G., Tan, Y., Kovacevic, M., Situm, M., McCoy, J. (2019). Tretinoin enhances minoxidil response in … Continue reading
Another way to improve sulfotransferase levels and, therefore, minoxidil efficacy is by undergoing microneedling. One study by Sharma et al. investigated the effect of microneedling on follicular sulfotransferase enzymes in male subjects with androgenic alopecia.[19]Sharma, A., Surve, R., Dhurat, R., Sinclair, R., Tan, Y., Zou, Y., Muller Ramos, R., Wambier, C., Verner, I., Kovacevic, M., Goren, A. (2020). Microneedling improves minoxidil response in … Continue reading Six male subjects underwent 3 weekly sessions of microneedling at 1.5 mm depth on a target area of the scalp. Sulfotransferase enzyme activity was analyzed in the hair follicle at the baseline and at the end of the three weeks. 66% of participants had an increase in sulfotransferase activity compared to the baseline, and 16% of subjects who were previously classified as “non-responders” to topical minoxidil were converted to “responder” status.
Figure 7. Sulfotransferase enzyme activity following microneedling treatment.[20]Sharma, A., Surve, R., Dhurat, R., Sinclair, R., Tan, Y., Zou, Y., Muller Ramos, R., Wambier, C., Verner, I., Kovacevic, M., Goren, A. (2020). Microneedling improves minoxidil response in … Continue reading
Final Thoughts
While some small studies suggest that testing for SULT1A1 variants might help to predict minoxidil efficacy, the evidence is not yet strong enough to make definitive treatment recommendations based solely on genotype. Larger and more robust studies are needed to confirm the true predictive value of genetic testing for SULT1A1 for personalizing hair loss treatments.
References[+]
References ↑1 Negishi, M., Pederson, L.G., Petrochenko, E., Shevtsov, S., Gorokhov, A., Kakuta, Y., Pederson, L.C. (2001). Structure and function of sulfotransferases. Archives of biochemistry and biophysics. 390(2). 149-157. Available at: https://doi.org/10.1006/abbi.2001.2368 ↑2 Gamage, N., Barnett, A., Hempel, N., Duggleby, R.G., Windmill, K.F., Martin, J.L., McManus, M.E. (2006). Human Sulfotransferases and Their Role in Chemical Metabolism. Toxicological Sciences. 90(1). 5-22. Available at: https://doi.org/10.1093/toxsci/kfj061 ↑3 National Library of Medicine. (2024). SULT1A1 sulfotransferase family 1A member 1 [Homo sapiens (human)]. NIH. Available at: https://www.ncbi.nlm.nih.gov/gene?Cmd=DetailsSearch&Db=gene&Term=6817 (Accessed: 03 June 2024) ↑4 Ramos, P.M., Gohad, P., McCoy, J., Wambier, C., Goren, A. (2021). Minoxidil Sulfotransferase Enzyme (SULT1A1) Genetic Variants Predicts Response to Oral Minoxidil Treatment for Female Pattern Hair Loss. Journal of the European Academy of Dermatology and Venereology: JEADV. 35(1). E24-e26. Available at: https://doi.org/10.1111/jdv.16765 ↑5 Goren, A., Castano, J.A., McCoy, J., Bermudez, F., Lotti, T. (2014). Novel enzymatic assay predicts minoxidil response in the treatment of androgenetic alopecia. Dermatologic Therapy. 27. 171-173. Available at: https://doi.org/10.1111/dth.12111 ↑6 Goren, A., Castano, J.A., McCoy, J., Bermudez, F., Lotti, T. (2014). Novel enzymatic assay predicts minoxidil response in the treatment of androgenetic alopecia. Dermatologic Therapy. 27. 171-173. Available at: https://doi.org/10.1111/dth.12111 ↑7 Roberts, J., Desai, N., McCoy, J., Goren, A. (2014). Sulfotransferase activity in plucked hair follicles predicts response to topical minoxidil in the treatment of female androgenetic alopecia. Dermatologic Therapy. 27(4). 252-254. Available at https://doi.org/10.1111/dth.12130 ↑8 Raftogianis, R.B., Wood, T.C., Otterness, D.M., Loon, J.A.V., Weinshilboum, R.M. (1997). Phenol Sulfotransferase Pharmacogenetics in Humans: Association of Common SULT1A1 Alleles with TS PST Phenotype. Biochemical and Biophysical Research Communications. 239(1). 298-304. Available at: https://doi.org/10.1006/bbrc.1997.7466 ↑9 Raghad, N.A., Al-Gazally, M.E., Ewahd, W.A. (2017). Assessment the effect of different genotypes of sulfotransferase 1A1 gene on the response to minoxidil in patients with androgenic alopecia. Journal of Global Pharma Technology. 10(9). 144-149 ↑10, ↑11, ↑12 Raghad, N.A., Al-Gazally, M.E., Ewahd, W.A. (2017). Assessment the effect of different genotypes of sulfotransferase 1A1 gene on the response to minoxidil in patients with androgenic alopecia. Journal of Global Pharma Technology. 10(9). 144-149 ↑13 Ramos, P.M., Gohad, P., McCoy, J., Wambier, C., Goren, A. (2021). Minoxidil Sulfotransferase Enzyme (SULT1A1) genetic variants predict response to oral minoxidil treatment for female pattern hair loss. Journal of the European Academy of Dermatology and Venererology. 35(1). E24-e26. Available at: https://doi.org/10.1111/jdv.16765 ↑14 Ramos, P.M., Gohad, P., McCoy, J., Wambier, C., Goren, A. (2021). Minoxidil Sulfotransferase Enzyme (SULT1A1) genetic variants predict response to oral minoxidil treatment for female pattern hair loss. Journal of the European Academy of Dermatology and Venererology. 35(1). E24-e26. Available at: https://doi.org/10.1111/jdv.16765 ↑15 Ramos, P.M., Sinclair, R.D., Kasprzak, M., Miot, H.A. (2020). Minoxidil 1 mg oral versus minoxidil 5% topical solution for the treatment of female-pattern hair loss: a randomized clinical trial. Journal of the American Academy of Dermatology. 82(1): 252-253. Available at: https://doi.org/10.1016/j.jaad.2019.08.060 ↑16 Asilian, A., Farmani, A., Saber, M. (2023). Clinical efficacy and safety of low-dose oral minoxidil versus topical solution in the improvement of androgenetic alopecia: a randomized controlled trial. Journal of Cosmetic Dermatology. 23(3). 949-957. Available at: https://doi/org/10.1111/jocd.16086 ↑17 Sharma, A., Goren, A., Dhurat, R., Agrawal, S., Sinclair, R., Trueb, R., Vano-Galvan, S., Chen, G., Tan, Y., Kovacevic, M., Situm, M., McCoy, J. (2019). Tretinoin enhances minoxidil response in androgenetic alopecia patients by upregulating follicular sulfotransferase enzymes. Dermatologic Therapy. 32(3). e12915. Available at: https://doi.org/10.1111/dth.12915 ↑18 Sharma, A., Goren, A., Dhurat, R., Agrawal, S., Sinclair, R., Trueb, R., Vano-Galvan, S., Chen, G., Tan, Y., Kovacevic, M., Situm, M., McCoy, J. (2019). Tretinoin enhances minoxidil response in androgenetic alopecia patients by upregulating follicular sulfotransferase enzymes. Dermatologic Therapy. 32(3). e12915. Available at: https://doi.org/10.1111/dth.12915 ↑19 Sharma, A., Surve, R., Dhurat, R., Sinclair, R., Tan, Y., Zou, Y., Muller Ramos, R., Wambier, C., Verner, I., Kovacevic, M., Goren, A. (2020). Microneedling improves minoxidil response in androgenetic alopecia patients by upregulating follicular sulfotransferase enzymes. Journal of Biological Regulators & Homeostatic Agents. 34(2). 659-661. Available at: 10.23812/19-385-L-51 ↑20 Sharma, A., Surve, R., Dhurat, R., Sinclair, R., Tan, Y., Zou, Y., Muller Ramos, R., Wambier, C., Verner, I., Kovacevic, M., Goren, A. (2020). Microneedling improves minoxidil response in androgenetic alopecia patients by upregulating follicular sulfotransferase enzymes. Journal of Biological Regulators & Homeostatic Agents. 34(2). 659-661. Available at: 10.23812/19-385-L-51 GPR44 is a gene that encodes the G-protein-coupled receptor 44, also known as the prostaglandin D2 receptor (DP2). This receptor plays a pivotal role in various physiological processes, including inflammation and immune responses.
GPR44 is considered significant in the context of hair loss because some believe it is involved in hair growth inhibition.
Early studies evaluating prostaglandin activity in the hair follicle found that elevated levels of prostaglandin D2 (PGD2) have been found in the scalps of individuals with androgenic alopecia. PGD2 exerts its effects through the GPR44 receptor.
This article will delve into the importance of the GPR44 gene in hair loss, its potential as a therapeutic target, and the significant role that understanding your genetic makeup can play in making informed treatment decisions.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is GPR44?
The GPR44 gene (also called CRTh2) codes for the expression of a type of receptor for prostaglandins, specifically PGD2.[1]National Library of Medicine. (2024). PTGDR2 Prostaglandin D2 Receptor 2 [Homo sapiens (human)]. NIH. Available at: https://www.ncbi.nlm.nih.gov/gene/11251 (Accessed: 12 July 2024.) Prostaglandin D2 is a bioactive lipid compound that belongs to the family of prostaglandins, which are derived from arachidonic acid. Prostaglandins are involved in various physiological processes, including inflammation, allergic reactions, and regulation of sleep-wake cycles. PGD2 is produced by several types of cells, including mast cells, dendritic cells, and other types of immune cells.
Studies suggest that PGD2 has been found to inhibit hair growth in isolated human hair follicles and mice. Furthermore, PGD2 has been found to be elevated in the scalps of balding men diagnosed with androgenetic alopecia.[2]Nieves, A., Garza, L.A. (2014). Does Prostaglandin D2 Hold the Cure to Male Pattern Baldness? Experimental Dermatology. 23(4). 224-227. Available at: https://doi.org/10.1111/exd.12348[3]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading
What is the Evidence for Targeting GPR44 for Hair Loss?
As mentioned above, PGD2 binds to its receptor, GPR44, to exert its effects. Studies on human scalp samples from the bald and haired areas of balding men found that the level of PGD2 was significantly higher in the scalps of the balding areas (Figure 1). Furthermore, PGE2, which has been linked to human hair growth, was found to be significantly lower in the bald scalp (Figure 1).[4]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading
Figure 1: Fold change in PGD2, 15-dPGJ2, and PGE2 expression in the bald scalp compared to the haired scalp. *P<0.05; **P<0.01.[5]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading
The same study evaluated the effect of high levels of PGD2 in mouse skin, hypothesizing that it might lead to the initiation of features of androgenic alopecia. The researchers used K14-Ptgs2 transgenic mice that are genetically modified to overexpress the Ptgs2 gene (also known as COX-2) specifically in the skin. These mice are often used in prostaglandin signaling studies as these specific genetic modifications increase levels of PGD2, PGE2, and 15-dPGJ2.
The mice overexpressing this gene were found to have hair follicles that entered premature catagen with subsequent development of alopecia.[6]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading
In a series of experiments, researchers investigated the effects of prostaglandin D2 (PGD2) on hair growth using C57Bl/6 mice, a common laboratory strain. They topically applied PGD2 to the shaved backs of these mice and measured hair length 20 days after depilation.
The results showed a significant inhibition of hair growth in the treated areas. To further explore the mechanism, the team used a separate mouse model with the GPR44 gene (which encodes a PGD2 receptor) knocked out. Interestingly, these GPR44-deficient mice demonstrated resistance to hair loss when PGD2 was applied topically, indicating that PGD2’s effect on hair loss was through the GPR44 receptor.[7]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading
Figure 2. Hair length 10 days after topical PGD2 (1 ug), 15-dPGJ2 (1 ug) or vehicle treatment.[8]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading
Clinical studies have found an association between the rs533116 and rs545659 polymorphisms of the GPR44 gene that enhances the expression of GPR44 in the lungs, resulting in an increase in asthma severity.[9]Campos Alberto, E., Maclean, E., Davidson, C., Palikhe, N.S., Storie, J., Tse, C., Brenner, D., Mayers, I., Vliagoftis, H., El-Sohemy, A., Cameron, L. (2012). The Single Nucleotide Polymorphism CRTh2 … Continue reading[10]Huang, J.L., Gao, P.S., Mathias, R.A., Yao, T.C., Chen, L.C., Kuo, M.L., Hsu, S.C., Plunkett, B., Togias, A., Barnes, K.C., Stellato, C., Beaty, T.H., Huang, S.K. Sequence Variants of the Gene … Continue reading
This increase in the expression of receptors like GPR44 may increase responsiveness to PGD2, so it’s possible that these findings may also apply to people with androgenic alopecia.
What is the Evidence Against Targeting GPR44 for Hair Loss?
In 2012, a study from the University of Pennsylvania and Johns Hopkins University generated a lot of excitement about a potential new treatment avenue for hair loss. The researchers found that PGD2 was elevated in the balding scalp but not in non-balding areas of the scalp of men with hair loss. Furthermore, they found that PGD2 inhibits hair growth.[11]Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). … Continue reading. This sparked an interest in prostaglandins as hair growth inhibitors.
Unfortunately, follow-up studies showed conflicting results – thanks to poorly controlled variables – and it is still unclear whether there is a causal relationship between prostaglandins and androgenetic alopecia.[12]English, R., Ruiz, S. (2021). Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia: Are Biopsy Location, Hair Diameter Diversity, and Relative Hair Follicle … Continue reading
A randomized, double-blind, placebo-controlled Phase 2a trial on setipiprant, a drug designed to bind to GPR44 and block PGD2 from exerting its effect, was conducted on males aged 18-49 with androgenic alopecia. The study found that setipiprant at 1000 mg twice daily for 24 weeks did not demonstrate efficacy compared to a placebo in improving hair growth, as measured by target area hair count and participant self-assessment. While setipiprant was safe and well-tolerated, it failed to show significant improvements indicating that targeting PGD2 alone is not sufficient to treat male pattern hair loss.[13]DuBois, J., Bruce, S., Stewart, D., Kempers, S., Harutunian, C., Boodhoo, T., Weitzenfeld, A, Chang-Lin, J.E. (2021). Setipiprant for Androgenetic Alopecia in Males: Results from a Randomized, … Continue reading
What Do Your Genetic Results Mean?
Your Result GPR44-1 Variant 1 GPR44-2 Variant 2 Rs545659 TT Rs545659 AA What it means May be at a lower risk of having elevated levels of PGD2 in the lungs/scalp. May be at an increased risk of having higher levels of GPR44 in the lungs/scalp. The Implication You might not be a good candidate for PGD2 inhibitors as a treatment for hair loss You might be a better candidate for PGD2 inhibitors as a treatment for hair loss Your Result GPR44-1 Variant 1 GPR44-2 Variant 2 GPR44-2 Variant 3 Rs533116 AA Rs533116 GG Rs533116 GA What it means May be at a lower risk of having elevated levels of PGD2 In the lungs/scalp. May be at moderate risk of having higher levels of GPR44 in the lungs/scalp. May be at an increased risk of having higher levels of GPR44 in the lungs/scalp. The Implication You might not be a good candidate for PGD2 inhibitors as a treatment for hair loss You might be an average candidate for PGD2 inhibitors as a treatment for hair loss You might be a better candidate for PGD2 inhibitors as a treatment for hair loss What Relevance Does GPR44 Have for Hair Loss Treatment?
We have also created a rubric that helps to determine the relevance of a specific gene to hair loss based on the quality of the evidence in the above studies.
- Does this gene have any potential relevance for hair loss? (1 point)
Yes, initial studies have shown that PGD2 levels are increased in the scalps of balding men. Experiments in mice suggest that PGD2 may inhibit hair growth. (score = 1)
- Does the totality of evidence implicate GPR44 as a causal agent for hair loss? (1 point)
There is not enough consistency of evidence to support the relationship between prostaglandin activity and androgenetic alopecia, due to further results conflicting with initial results. (score = 0)
- Does the totality of evidence implicate GPR44 as a predictive factor for hair loss treatment responsiveness? (2 points)
Although earlier studies showed that PGD2 is elevated in balding scalps, targeting this has not shown to be effective at treating hair loss. (score = 0)
- Is this quality of evidence on (3) strong enough to influence treatment recommendations? (1 point)
No score on number (3). (score = 0)
Total Score = 1
Final Thoughts
While early research has highlighted the potential involvement of the GPR44 gene in hair loss through its interaction with prostaglandin D2 (PGD2), the current evidence is not robust enough to make definitive treatment recommendations based solely on the GPR44 genotype. Therefore, more comprehensive and consistent research is needed to validate the role of GPR44 in hair loss and its potential as a predictive factor for treatment responsiveness.
References[+]
References ↑1 National Library of Medicine. (2024). PTGDR2 Prostaglandin D2 Receptor 2 [Homo sapiens (human)]. NIH. Available at: https://www.ncbi.nlm.nih.gov/gene/11251 (Accessed: 12 July 2024.) ↑2 Nieves, A., Garza, L.A. (2014). Does Prostaglandin D2 Hold the Cure to Male Pattern Baldness? Experimental Dermatology. 23(4). 224-227. Available at: https://doi.org/10.1111/exd.12348 ↑3, ↑4, ↑6, ↑7 Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). Prostaglandin D2 Inhibits Hair Growth and is Elevated in Bald Scalp of Men with Androgenetic Alopecia. Science Translational Medicine. 4(126). 1-21. Available at: https://doi.org/10.1126/scitranslmed.3003122 ↑5, ↑8, ↑11 Garza, L.A., Liu, Y., Alagesan, B., Lawson, J.A., Norberg, S.M., Loy, D.R., Zhao, T., Blatt, H.B., Stanton, D.C., Carrasco, L., Ahluwalia, G., Fischer, S.M., Fitzgerald, G.A., Cotsarelis, G. (2012). Prostaglandin D2 Inhibits Hair Growth and is Elevated in Bald Scalp of Men with Androgenetic Alopecia. Science Translational Medicine. 4(126). 1-21. Available at: https://doi.org/10.1126/scitranslmed.3003122 ↑9 Campos Alberto, E., Maclean, E., Davidson, C., Palikhe, N.S., Storie, J., Tse, C., Brenner, D., Mayers, I., Vliagoftis, H., El-Sohemy, A., Cameron, L. (2012). The Single Nucleotide Polymorphism CRTh2 rs533116 is Associated with Allergic Asthma and Increased Expression of CRTh2. Allergy. 67(11). 1357-1364. Available at: https://doi.org/10.1111/all.12003 ↑10 Huang, J.L., Gao, P.S., Mathias, R.A., Yao, T.C., Chen, L.C., Kuo, M.L., Hsu, S.C., Plunkett, B., Togias, A., Barnes, K.C., Stellato, C., Beaty, T.H., Huang, S.K. Sequence Variants of the Gene Encoding Chemoattractant Receptor Expressed on Th2 Cells (CRTH2) are Associated with Asthma and Differentially Influence mRNA Stability. Human Molecular Genetics. 13(21). 2691-2697. Available at: https://doi.org/10.1093/hmg/ddh279 ↑12 English, R., Ruiz, S. (2021). Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia: Are Biopsy Location, Hair Diameter Diversity, and Relative Hair Follicle Miniaturization Partly to Blame? Clinical, Cosmetic, and Investigational Dermatology. 14. 357-365. Available at: https://doi.org/10.2147/CCID.S306157 ↑13 DuBois, J., Bruce, S., Stewart, D., Kempers, S., Harutunian, C., Boodhoo, T., Weitzenfeld, A, Chang-Lin, J.E. (2021). Setipiprant for Androgenetic Alopecia in Males: Results from a Randomized, Double-Blind, Placebo-Controlled Phase 2a Trial. Clinical Cosmetic and Investigative Dermatology. 14. 1507-1517. Available at: https://doi.org/10.2147/CCID.S319676 HMI-115 is a potential new treatment for hair loss that is licensed by Hope Medicine Inc. HMI-115 has been used in a phase 1 clinical trial for hair loss and has been approved by the FDA for phase 2 trials. This treatment is also in phase 2 clinical trials for use in endometriosis. HMI-115 is gathering media attention as a treatment that may come to the market within the next few years.
HMI-115 belongs to a class of drugs known as prolactin (PRL) receptor antagonists – it works by blocking the effects of prolactin within the hair follicle by binding to and blocking the prolactin receptor. In this article, we will take a look at what HMI-115 and prolactin are and then consider how prolactin might be involved in hair follicle biology and hair loss disorders. Furthermore, we will investigate the potential impact of HMI-115 in treating androgenetic alopecia and determine whether it is likely that phase 2 clinical trials for HMI-115 will return positive results.
Key Takeaways
- Drug. HMI-115 is a drug that comes under a class of therapeutics called prolactin receptor antagonists. This drug is licensed by Bayer, which is investigating its use as a drug treatment for endometriosis. HMI-115 is also licensed by Hope Medicine Inc., which used the drug in a phase 1 clinical trial for patients with androgenetic alopecia. The FDA has also approved HMI-115 for phase 2 trials for treating hair loss, although these trials have not yet started.
- Clinical Data. In a press release, Hope Medicine Inc. reported results from its phase 1 trial, which included a significant increase in the mean non-vellus total area hair count across the 12 males in the trial—an increase of 14 hairs/cm2 after 24 weeks. The study has not been peer-reviewed, nor have the full results been published. Furthermore, no data was provided for the 4 women included in the study.
- Safety. There was a phase 1 safety trial completed by Bayer (who licensed HMI-115 to Hope Medicine Inc.) in which up to 90 mg of the drug, delivered via subcutaneous injections every 2 weeks, was found to be well tolerated. This study, however, aimed toward using HMI-115 to treat endometriosis. The phase 1 clinical trial on hair loss, sponsored by Hope Medicine Inc., delivered 240mg of HMI-115 via subcutaneous injection every two weeks; they reported it to be safe and tolerable, though no supporting data was provided.
- Evidence Quality. HMI-115 serum scored 21/100 for evidence quality, by our metrics (this is subject to change depending on the results of clinical trials currently being undertaken).
All-Natural Hair Supplement + Topical
The top natural ingredients for hair growth, all in one serum & supplement.
Take the next step in your hair growth journey with a world-class natural serum & supplement. Ingredients, doses, & concentrations built by science.

What is HMI-115?
HMI-115 (also known as BAY1158061) is a new pharmaceutical drug developed by a biopharmaceutical company called Bioinvent and licensed by Bayer – a German multinational pharmaceutical and biotechnology company. HMI-115 has been subsequently licensed from Bayer by Hope Medicine Inc. for use as a hair loss treatment. So far, research around HMI-115 is geared toward treating endometriosis and male and female pattern hair loss. In terms of administration, HMI-115 is delivered via subcutaneous injection.
HMI-115 is a prolactin receptor antagonistic antibody.[1]Hope Medicine, (no date). Clinical Development. Research and Development. Available at: https://www.hopemedinc.com/research-platform?tp2 (Accessed: 21 April 2023) This is a type of therapeutic antibody that binds to the prolactin receptor, thereby inhibiting its activity by stopping prolactin from binding to its receptor.[2]Ferraris, J., Bernichten, S., Pisera, D., Goffin, V. (2013). Use of prolactin receptor antagonists to better understand prolactin regulation of pituitary homeostasis. Neuroendocrinology. 98. 171-179. … Continue reading Prolactin is a type of hormone produced by the pituitary gland. As indicated by its name, prolactin is a hormone that promotes lactation (milk production). In reality, prolactin is a pleiotropic hormone with many different functions in both men and women. We will go into more detail below about prolactin, its potential role in hair loss, and how HMI-115 might work to restore hair growth by inhibiting prolactin.
What is Hope Medicine Incorporated?
Hope Medicine Inc. is a Chinese biopharmaceutical company founded by Professor Rui Ping Xiao of Peking University. According to their website, Hope Medicine Inc. was founded on the basis of a thorough understanding of disease biology and the practical application of medical research.[3]Hope Medicine, (no date), About Hope Medicine. Available at: https://www.hopemedinc.com/ (Accessed: 21 April 2023) Hope Medicine Inc. focuses on developing small molecule drugs that target specific proteins or pathways involved in disease.
In 2019, Hope Medicine Inc. announced a license agreement with Bayer AG in which Hope Medicine will develop and commercialize HMI-115 as a treatment for male and female pattern hair loss, endometriosis, and other conditions.[4]Cision, (no date), Hope Medicine announces global license agreement with Bayer AG to advance the development and commercialization of the monoclonal antibody directed against prolactin (PRL) … Continue reading
In 2022, Hope Medicine announced that the US Food and Drug Administration (FDA) had approved an application for HMI-115 to be used as an investigational new drug for the treatment of androgenetic alopecia or pattern hair loss, meaning that phase 2 clinical trials can begin in the US. Hope Medicine stated that the company’s plans for its phase 2 trial for androgenetic alopecia would be an international multi-center, randomized, double-blind, placebo-controlled study. Participating countries include the US, Australia, and others. [5]Cision, (no date), Hope Medicine announces a global license agreement with Bayer AG to advance the development and commercialization of the monoclonal antibody directed against prolactin (PRL) … Continue reading
Are these trials likely to work? Let’s get into the science of how this prolactin receptor antagonist, HMI-115, might function. First, we’ll take a deep dive into what prolactin is and how it might affect hair follicle biology.
What is Prolactin?
Prolactin is a hormone produced and secreted by the anterior pituitary gland. Prolactin is named for its stimulatory effect on lactation (milk production), but in actuality, prolactin has many different functions in both men and women.[6]Freeman, M.A., Kanyicska, B., Lerant, A., Nagy, Gyorgy. (2000). Prolactin: structure, function, and regulation of secretion. Physiological Reviews. 80(4), 1523-1631. Available at: … Continue reading The normal range of prolactin in non-pregnant women is below 25 ng/ml and in men, below 20 ng/ml.[7]Majumdar, A., Mangal, N.S. (2013). Hyperprolactinemia. Journal of Human Reproductive Sciences. 6(3). 168-175. Available at: https://doi.org/10.4103/0974-1208.121400
High levels of prolactin can lead to a medical condition called hyperprolactinemia. Symptoms of hyperprolactinemia can include irregular menstrual periods/loss of menstrual periods in women, decreased sex drive and erectile dysfunction in men, infertility, overproduction of breast milk in non-pregnant or non-breastfeeding women, and also osteoporosis.[8]Capozzi, A., Scambia, G., Pontecorvi, A., Lello, S. (2015). Hyperprolactinemia: pathophysiology and therapeutic approach. Gynecological Endocrinology. 31(7). 506-510. Available at: … Continue reading
It is also thought that high prolactin levels may also be involved in hair loss (more on that below).[9]Schmidt, J.B. (1994). Hormonal basis of male and female androgenic alopecia: clinical relevance. Skin Pharmacology. 7. 61-66. Available at: https://doi.org/10.1159/000211275
How is Prolactin Involved in Hair Cycling and Loss?
Prolactin upregulates several molecular signaling pathways that are associated with hair loss. For example, the Janus kinase-signal transducer and activator of transcription (JAK/STAT) pathway is activated by prolactin.[10]Ma, F.Y., Anderson, G.M., Gunn, T.D., Goffin, V., Grattan, D.R., Bunn, S.J. (2005). Prolactin specifically activates signal transducer and activator of transcription 5b in neuroendocrine dopaminergic … Continue reading The JAK/STAT pathway is known to be involved in hair loss in patients with alopecia areata; therefore, elevated prolactin levels may subsequently enhance the JAK/STAT pathway, leading to worse severity of the disease.
Prolactin and prolactin receptors are expressed at both the mRNA and protein levels in the hair follicle. Furthermore, both of these appear to be up-regulated in the late growing stage (anagen) into the transitional stage (catagen) of the hair follicle cycle.[11]Foitzik, K., Krause, K., Conrad, F., Nakamura, M., Funk, W., Paus, R. (2006). Human scalp hair follicles are both a target and a source of prolactin, which serves as an autocrine and/or paracrine … Continue reading The researchers also found that treatment of isolated human hair follicles with high doses of prolactin (around 400 ng/ml) resulted in significant inhibition of hair growth and premature transition into catagen compared to control hair follicles. Additionally, markers for cell growth and cell death were reduced and increased, respectively, following prolactin treatment. Hair follicles were also staged for the hair cycle following prolactin treatment, and there was a significant increase in the number of treated follicles in the catagen stage. These findings indicate that prolactin can impact hair follicle biology and that prolactin may function as an inducer of catagen.
Figure 1: Effect of 400 ng/ml of prolactin on (LEFT): hair follicle growth and (RIGHT): stage of the hair follicle cycle.[12]Foitzik, K., Krause, K., Conrad, F., Nakamura, M., Funk, W., Paus, R. (2006). Human scalp hair follicles are both a target and a source of prolactin, which serves as an autocrine and/or paracrine … Continue reading
In another study, in mice, it was found that prolactin is closely involved in regulating the hair follicle cycle. Prolactin levels increased in mice at 3 weeks, just before the onset of anagen (Figure 2), with a subsequent increase in the prolactin receptor at the start of the anagen stage. This increase in prolactin levels was associated with a concomitant increase in levels of prolactin receptors in the hair follicle. Suppression of prolactin secretion (through oral treatment of a known inhibitor of prolactin called bromocriptine) from the pituitary gland induced hair growth 3-5 days earlier, which was returned to normal by treating the mice with prolactin for 3 days. Increasing the duration of treatment had an inhibitory effect on hair growth.[13]Craven, A.J., Nixon, A.J., Ashby, M.G., Ormandy, C.J., Blazek, K., Wilkins, R.J., Pearson, A.J. (2006). Prolactin delays hair regrowth in mice. Journal of Endocrinology. 191. 415-425. Available at: … Continue reading
Figure 2: Levels of circulating prolactin in mice. Prolactin levels appear to increase at around 21 days (3 weeks) of age – around one week before the mice enter the anagen stage of the hair follicle cycle.[14]Craven, A.J., Nixon, A.J., Ashby, M.G., Ormandy, C.J., Blazek, K., Wilkins, R.J., Pearson, A.J. (2006). Prolactin delays hair regrowth in mice. Journal of Endocrinology. 191. 415-425. Available at: … Continue reading
There is some evidence demonstrating that prolactin is involved in regulating hair follicle cycling. However, is prolactin relevant to hair loss disorders in humans?
In women, hyperprolactinemia was found to be associated with androgenetic alopecia-pattern hair loss, as well as hirsutism (excess facial hair).[15]Schmidt, J.B. (1994). Hormonal basis of male and female androgenic alopecia: clinical relevance. Skin Pharmacology. 7. 61-66. Available at: https://doi.org/10.1159/000211275 A study involving 65 males (mean age of 24) and 46 females (mean age of 34) with androgenetic alopecia was conducted, and levels of different hormones were measured in comparison to 58 male and 45 female healthy controls. Prolactin, however, was only measured in the females in the study. Using a TRH test – which stimulates prolactin release from the pituitary – the researchers measured the levels of TRH-induced prolactin in both hair loss patients and controls (Figure 3). The researchers wanted to see whether the total stores of prolactin were increased in those with hair loss or whether the prolactin system was hypersensitive in some way. The female Patients were administered 0.2 mg of TRH and then had blood taken after 0 minutes, 20 minutes, and 40 minutes of treatment. Prolactin levels were then measured. This was taken during the luteal phase of the menstrual cycle (around day 14 to 28) when prolactin levels were higher than normal. It is important to note, however, that prolactin levels can be highly dynamic.
The researchers found an increase in prolactin levels at minute 0 and minute 20 following TRH administration in patients with androgenetic alopecia compared to the control patients, but these results were not statistically significant. However, there was a significant increase in prolactin levels after 40 minutes of TRH administration (p=<0.05). In conclusion, the findings of this study suggest that prolactin levels may be elevated in patients with androgenetic alopecia.
Figure 3: Median basal and stimulated levels of prolactin (PRL) and thyroid stimulating hormone (TSH), 0 minutes, 20 minutes, and 40 minutes after stimulation with TRH in female hair loss patients and controls. Adapted from:[16]Schmidt, J.B. (1994). Hormonal basis of male and female androgenic alopecia: clinical relevance. Skin Pharmacology. 7. 61-66. Available at: https://doi.org/10.1159/000211275
Another study looked at 40 women (aged between 30 and 65) with moderately increased prolactin levels, alongside androgenetic alopecia or diffuse hair loss, to determine the effects that prolactin might have on hair loss.[17]Lutz, G. (2011). Hair loss and hyperprolactinemia in women. Dermato-Endocrinology. 4(1). 70-76. Available at: https://doi.org/10.4161/der.19472 Prolactin levels varied widely in these patients, with the lowest level being 25.1 ng/ml and the highest being 1390 ng/ml. Interestingly, there did not appear to be any correlation between the number of non-growing hairs and prolactin levels, leading the researchers to conclude that it was not likely that elevated prolactin levels were the cause of diffuse or androgenetic alopecia (Figures 4 & 5).
Figure 4: Prolactin levels in patients with either diffuse or androgenetic alopecia. Adapted from:[18]Lutz, G. (2011). Hair loss and hyperprolactinemia in women. Dermato-Endocrinology. 4(1). 70-76. Available at: https://doi.org/10.4161/der.19472
Figure 5: Number of telogen hairs of patients with either diffuse or androgenetic alopecia. Vertical axis = the number of telogen hairs; Horizontal axis = patient. Adapted from: [19]Lutz, G. (2011). Hair loss and hyperprolactinemia in women. Dermato-Endocrinology. 4(1). 70-76. Available at: https://doi.org/10.4161/der.19472
A case-control study of 30 patients (16 men and 14 women) aged between 18-46 with alopecia areata (AA) and 20 controls (9 males and 11 females) aged between 18-45 was undertaken.[20]Tahlawi, S.M.E., Eishi, N.H.E., Kahhal, R.K., Hegazy, R.A., Hanafy, G.M.E., Hay, R.M.A., Shaker, O.G. (2018). Do prolactin and its receptor play a role in alopecia areata? Indian Journal of … Continue reading When comparing the serum prolactin level between AA patients and controls using an ELISA assay, no significant differences were found. PCRs were then completed with RNA harvested from biopsies taken from the lesional skin of AA patients and the occipital scalp skin of controls. An increase in the level of prolactin receptors was observed in the AA patients compared to the control patients (Figure 6). This indicates a potential hypersensitivity to prolactin in patients with AA rather than excess prolactin.
Figure 6: Comparison of the mean serum prolactin level and mean tissue prolactin receptor levels in AA patients vs. control patients. Adapted from:[21]Tahlawi, S.M.E., Eishi, N.H.E., Kahhal, R.K., Hegazy, R.A., Hanafy, G.M.E., Hay, R.M.A., Shaker, O.G. (2018). Do prolactin and its receptor play a role in alopecia areata? Indian Journal of … Continue reading
Furthermore, the levels of prolactin receptors correlate with the SALT score (Severity of Alopecia Tool) – a common score used in studies to assess the extent of scalp hair loss.
Overall, some evidence implicates prolactin in the pathogenesis of androgenetic alopecia. However, there are some contradicting findings about whether prolactin is involved in the pathogenesis of hair loss. Moreover, one might expect there to be more of a concrete link between pregnancy and hair loss, given the large changes in prolactin that occur during late pregnancy and throughout breastfeeding. However, there is little evidence of changes in hair loss and ratios of anagen/telogen hairs between different stages of pregnancy or breastfeeding status.[22]Mirallas, O., Grimalt, R. (2016). The postpartum telogen effluvium fallacy. 1(4), 198-201. Available at: https://doi.org/10.1159/000445385
However, given the caveats above, let us assume for a moment that prolactin is a definitive cause of hair loss, so why not just use already-known treatments for hyperprolactinemia, such as the drug cabergoline?
A major mechanism regulating prolactin levels is dopamine secretion by neurons in the hypothalamus. Dopamine then inhibits the secretion of prolactin from the pituitary. Cabergoline is a dopamine agonist and so promotes the action of dopamine. Some case studies have indicated that dopamine agonists like cabergoline may cause hair loss in some people. One such study included a 71-year-old woman with Parkinson’s disease who experienced progressive hair loss after taking 3 mg of cabergoline for one month. After 4 months of decreasing the dose, however, (from 3 mg to 1 mg), the patient’s hair was completely re-grown.[23]Miwa, H., Kondo, T. (2003). Hair loss induced by dopamine agonist: case report and review of the literature. Parkinsonism & Related Disorders. 10. 51-52. Available at: … Continue reading An earlier study also reports two women suffering from diffuse alopecia as a result of taking levodopa (dopamine replacement) as a treatment for Parkinson’s.[24]Marshall, A., Williams M.J. (1971). Alopecia and levodopa. British Medical Journal. 2(5752), 47. Available at: https://doi.org/10.1136/bmj.2.5752.47 Whether dopaminergic drugs could benefit hair loss in otherwise healthy people is unclear. In any case, given the widespread importance of dopamine in regulating mood and behavior, targeting this system as a therapy for hair loss may not be a wise strategy. Therefore, other pharmaceutical approaches, like the blockade of prolactin receptors, may be a better method. That is if prolactin is indeed related to hair loss.
So, let’s have a look at whether there is any evidence currently to suggest that the prolactin receptor antagonist HMI-115 might benefit those with hair loss.
Could HMI-115 work for Patients with Androgenetic Alopecia?
Recent data showing the potential effects of HMI-115 in humans has been released, but let’s first look at the published animal data.
Animals
Bayer AG did complete a study using a primate model of androgenetic alopecia, which Bayer AG goes into detail about in their patent application.[25]Ekkehard, M., Joachim, S., Jorn, K., Christiane, O. (2017). Prolactin receptor antibody for male and female pattern hair loss. World Intellectual Property Organization. Available at: … Continue reading Unfortunately, this study does not appear to be published anywhere other than in the patent application that we found on Google (such as in a peer-reviewed scientific journal).
This study attempted to leverage an apparent phenomenon of spontaneous post-adolescence scalp hair loss in stump-tailed macaques as a model system to test the effects of HIM-115. Over a period of 6 months, the macaques were treated with HMI-115. The researchers claim that terminal hairs nearly doubled throughout the treatment. Unfortunately, the data is only given in terms of change from baseline, and there does not seem to be an untreated control group, which makes it difficult to conclude whether HMI-115 is doing anything (Figure 7).
Figure 7: Effect of HMI-115 treatment on Hair Growth in Stump-Tailed Macaques with Androgenetic Alopecia over 24 weeks. Adapted from:[26]Ekkehard, M., Joachim, S., Jorn, K., Christiane, O. (2017). Prolactin receptor antibody for male and female pattern hair loss. World Intellectual Property Organization. Available at: … Continue reading
Humans
There are two clinical trials currently recruiting for HMI-115: one phase 2 trial for endometriosis-associated pain and another phase 2 trial for treating male androgenetic alopecia over 24 weeks.[27]Clinical Trials, (no date). HMI-115. Available at: https://clinicaltrials.gov/ct2/results?cond=&term=HMI-115&cntry=&state=&city=&dist= (Accessed: 02 May 2024) The latter of the two follows on from a now complete phase 1 trial, whereby HMI-115 was tested as a treatment for male and female androgenetic alopecia.[28]Hope Medicine. (2023). An Open Label Study, to Evaluate Safety, Tolerability, and Efficacy in Male and Female With Androgenetic Alopecia Treated With HMI-115 Over a 24-Week Treatment Period (Clinical … Continue reading Importantly, this means that we have some information regarding the efficacy and safety of HMI-115 in humans – here’s what they found.
The study investigated the potential of HMI-115 as a treatment for both male and female androgenetic alopecia. 12 male and 4 female participants were given 240mg of HMI-115 every two weeks by subcutaneous injection for 24 weeks. The primary measurement was a change in target area hair count (TAHC) of non-vellus hair from baseline (week 0) to week 24.
In a press release, Hope Medicine Inc. (the sponsor of the trial) stated that “HMI-115 demonstrated positive efficacy results. It is also safe and well-tolerated”.[29]Hope Medicine. (No date). Positive Outcome from a Phase Ib Study in Australia Treating Patients with Androgenic Alopecia. Hope Medicine Available at: https://www.hopemedinc.com/company-release-37 … Continue reading. The press release also showed that the mean non-vellus TAHC increased by 14 hairs/cm2 in the male group, which was reported as a statistically significant increase. Hope Medicine Inc. acknowledges that this is the first indication that a prolactin blockade receptor may promote hair growth in patients with androgenetic alopecia, potentially opening the door for its use as a novel therapeutic.
While this does sound promising, there are several drawbacks. First and foremost, these results have (at the time of writing) only been shared as a press release. This means that the study and the results have not been peer-reviewed. In other words, no external reviewers have evaluated the study and ensured its integrity.[30]Kelly, J., Sadeghieh, T., Khosrow, A. (2014). Peer Review in Scientific Publications: Benefits, Critiques, & A Survival Guide. eJIFCC. 25(3). 227-243. PMID: 27683470 The lack of peer review means that we can’t be sure that unwanted results have not been omitted. Of the single measurement that has been reported, change in non-vellus TAHC, it is difficult to contextualize an increase of 14 hairs/cm2 – is that a large, moderate, or small change?
Furthermore, the study was conducted on a small number of participants. Generally speaking, the greater the sample size, the more reliable the results. In testing just 12 males and 4 females, the statistical power is low, and there is a risk of obtaining false-positive and false-negative results.[31]Andrade, C., (2020). Sample Size and its Importance in Research. Indian Journal of Psychological Medicine. 42(1). 102-103. Available at: https://doi.org/10.4103/IJPSYM.IJPSYM_504_19
On the one hand, it can be difficult to determine outliers, subjects who differ greatly from the average. For example, a few hyper-responders could see huge increases in their TAHC and cause the mean change of the group to be significant, while the majority of the subjects see no change. On the other hand, small sample sizes can obscure meaningful changes and smaller positive effects that do not reach significance. In either case, small sample sizes do not offer a good estimation of how the treatment may perform in the wider population. Furthermore, Hope Medicine didn’t include any results for the 4 women included, but it is unlikely that there would have been any statistically significant differences anyway.
With that said, HMI-115 does seem to have produced some positive effects, and the phase 2 trial should address some of the issues that hold back its phase 1 counterpart.
What are the Chances of HMI-115 Making it Through Phase 2 Clinical Trials?
So, as mentioned, Hope Medicine Inc. has been approved by the FDA to conduct Phase 2 clinical trials, and they are currently attempting to recruit 180 males with androgenetic alopecia for another 24-week study.
This may sound promising, but, in actual fact, phase 2 trials are generally considered to be the biggest milestone in drug development. The biggest reasons that phase 2 testing might fail are:
- Previously unknown serious side effects occur
- The trial shows insufficient efficacy – i.e., it doesn’t work as well as the researchers initially thought
- Poor commercial viability
It should also be noted that more than 30% of drugs entering phase 2 studies fail to progress, and more than 58% of drugs that do progress then go on to fail in phase 3 trials.[32]Norman, G.A.V. (2019). Phase II trials in drug development and adaptive trial design. JACC Basic to Translational Science. 4(3). 428-437. Available at: https://doi.org/10.1016/j.jacbts.2019.02.005
While the odds are stacked against anyone trying to get their drug through phase 2 clinical trials, the phase 1 trial did provide some hope for HMI-115. Although the study has a number of drawbacks, if the positive effect seen in the males is true (and that’s a big ‘if’), then it provides the best (and only) indication thus far that prolactin receptor blockades may be compatible as a treatment for androgenetic alopecia.
Is HMI-115 Safe?
A safety study was conducted by Bayer AG in a randomized controlled trial with 29 healthy postmenopausal women.[33]Nave, R., Jodi, S., Hoffman, A., Gashaw, I., Zollmann, F., Berse, M., Hochel, J., Kratzschmar, J., Rohde, B. (2019). Monoclonal antibody against prolactin receptor: a randomized placebo-controlled … Continue reading
Participants were split into four groups and administered either HMI-115 or a placebo via subcutaneous injection. Treatments were administered either once every two weeks or once every 3 weeks. The treatment doses were 30 mg (14-day interval), 60 mg (28-day interval), or 90 mg (14-day interval) of HMI-115 or a placebo control on three occasions.
The most frequently occurring adverse events in more than 10% of all study participants (including placebo) were headache, nasopharyngitis (common cold), nausea, lower abdominal pain, injection site bruises, general weakness, back pain, hot flush, oral herpes, temperature increase, and pain in extremities. The adverse events in more than 10% of participants that were associated with HMI-115 were headache, lower abdominal pain, hot flush, and nausea. Compared to the placebo, the frequency of adverse events was not increased with HMI-115, and no dose-dependent increase in adverse event frequency was observed.
Furthermore, the treatment was slowly absorbed, reaching peak concentrations approximately 5 – 11 days after dosing. After the final 90 mg dose, HMI-115 was eliminated from the blood plasma around 16 days later. The researchers determined that the three different dosages of HMI-115 were well-tolerated in healthy postmenopausal women, with no allergic reactions seen.
It remains to be seen if HMI-115 is safe in the long term, or across a larger, more representative group of patients. Furthermore, this study was completed in the context of treating endometriosis; therefore, the number of treatments, the concentration of the drug, and the duration of treatment time may differ from those who may be administered this drug for hair loss disorders.
For comparison, the completed phase 1 clinical trial, which Hope Medicine Inc. sponsored, treated patients with androgenetic alopecia 240 mg of HMI-115 every 2 weeks via subcutaneous injection, which is much higher than the concentrations used in the safety study completed by Bayer.[34]Clinical Trials, (no date). HMI-115. Available at: https://clinicaltrials.gov/ct2/results?cond=&term=HMI-115&cntry=&state=&city=&dist= (Accessed: 21 April 2023) Hope Medicine Inc. reported that this delivery of HMI-115 proved safe and tolerable, though they did not provide any data to support this statement.
Is HMI-115 for Me?
Well, HMI-115 is not yet available, and it looks like it won’t be available for another few years, at least as we look to the beginning of the phase 2 trials. While it’s still too early to tell if this product will make it to the market, we look forward to seeing the full results from the phase 1 trial and those from further trials to come.
References[+]
References ↑1 Hope Medicine, (no date). Clinical Development. Research and Development. Available at: https://www.hopemedinc.com/research-platform?tp2 (Accessed: 21 April 2023) ↑2 Ferraris, J., Bernichten, S., Pisera, D., Goffin, V. (2013). Use of prolactin receptor antagonists to better understand prolactin regulation of pituitary homeostasis. Neuroendocrinology. 98. 171-179. Available at: https://doi.org/10.1159/000354701 ↑3 Hope Medicine, (no date), About Hope Medicine. Available at: https://www.hopemedinc.com/ (Accessed: 21 April 2023) ↑4 Cision, (no date), Hope Medicine announces global license agreement with Bayer AG to advance the development and commercialization of the monoclonal antibody directed against prolactin (PRL) receptor. CISION PR Newswire. Available at: https://en.prnasia.com/releases/apac/hope-medicine-announced-global-license-agreement-with-bayer-ag-to-advance-the-development-and-commercialization-of-the-monoclonal-antibody-directed-against-prolactin-prl-receptor-242094.shtml (Accessed: 21 April 2023) ↑5 Cision, (no date), Hope Medicine announces a global license agreement with Bayer AG to advance the development and commercialization of the monoclonal antibody directed against prolactin (PRL) receptor. CISION PR Newswire. Available at: https://en.prnasia.com/releases/apac/hope-medicine-announced-global-license-agreement-with-bayer-ag-to-advance-the-development-and-commercialization-of-the-monoclonal-antibody-directed-against-prolactin-prl-receptor-242094.shtml (Accessed: 21 April 2023) ↑6 Freeman, M.A., Kanyicska, B., Lerant, A., Nagy, Gyorgy. (2000). Prolactin: structure, function, and regulation of secretion. Physiological Reviews. 80(4), 1523-1631. Available at: https://doi.org/10.1152/physrev.2000.80.4.1523 ↑7 Majumdar, A., Mangal, N.S. (2013). Hyperprolactinemia. Journal of Human Reproductive Sciences. 6(3). 168-175. Available at: https://doi.org/10.4103/0974-1208.121400 ↑8 Capozzi, A., Scambia, G., Pontecorvi, A., Lello, S. (2015). Hyperprolactinemia: pathophysiology and therapeutic approach. Gynecological Endocrinology. 31(7). 506-510. Available at: https://doi.org/10.3109/09513590.2015.1017810 ↑9, ↑15, ↑16 Schmidt, J.B. (1994). Hormonal basis of male and female androgenic alopecia: clinical relevance. Skin Pharmacology. 7. 61-66. Available at: https://doi.org/10.1159/000211275 ↑10 Ma, F.Y., Anderson, G.M., Gunn, T.D., Goffin, V., Grattan, D.R., Bunn, S.J. (2005). Prolactin specifically activates signal transducer and activator of transcription 5b in neuroendocrine dopaminergic neurons. Endocrinology. 146(12). 5112-5119. Available at: https://doi.org/10.1210/en.2005-0770 ↑11, ↑12 Foitzik, K., Krause, K., Conrad, F., Nakamura, M., Funk, W., Paus, R. (2006). Human scalp hair follicles are both a target and a source of prolactin, which serves as an autocrine and/or paracrine promoter of apoptosis-driven hair follicle regression. The American Journal of Pathology. 168(3). 748-756. Available at: https://doi.org/10.2353/ajpath.2006.050468 ↑13, ↑14 Craven, A.J., Nixon, A.J., Ashby, M.G., Ormandy, C.J., Blazek, K., Wilkins, R.J., Pearson, A.J. (2006). Prolactin delays hair regrowth in mice. Journal of Endocrinology. 191. 415-425. Available at: https://doi.org/10.1677/joe.1.06685 ↑17, ↑18, ↑19 Lutz, G. (2011). Hair loss and hyperprolactinemia in women. Dermato-Endocrinology. 4(1). 70-76. Available at: https://doi.org/10.4161/der.19472 ↑20 Tahlawi, S.M.E., Eishi, N.H.E., Kahhal, R.K., Hegazy, R.A., Hanafy, G.M.E., Hay, R.M.A., Shaker, O.G. (2018). Do prolactin and its receptor play a role in alopecia areata? Indian Journal of Dermatology. 63(3), 241-245. https://doi.org/10.4103/ijd.IJD_590_17 ↑21 Tahlawi, S.M.E., Eishi, N.H.E., Kahhal, R.K., Hegazy, R.A., Hanafy, G.M.E., Hay, R.M.A., Shaker, O.G. (2018). Do prolactin and its receptor play a role in alopecia areata? Indian Journal of Dermatology. 63(3), 241-245. https://doi.org/10.4103/ijd.IJD_590_17 ↑22 Mirallas, O., Grimalt, R. (2016). The postpartum telogen effluvium fallacy. 1(4), 198-201. Available at: https://doi.org/10.1159/000445385 ↑23 Miwa, H., Kondo, T. (2003). Hair loss induced by dopamine agonist: case report and review of the literature. Parkinsonism & Related Disorders. 10. 51-52. Available at: https://doi.org/10.1016/S1353-8020(03)00058-0 ↑24 Marshall, A., Williams M.J. (1971). Alopecia and levodopa. British Medical Journal. 2(5752), 47. Available at: https://doi.org/10.1136/bmj.2.5752.47 ↑25 Ekkehard, M., Joachim, S., Jorn, K., Christiane, O. (2017). Prolactin receptor antibody for male and female pattern hair loss. World Intellectual Property Organization. Available at: https://patentimages.storage.googleapis.com/56/cc/a3/7d3ac32f1537b2/WO2019011719A1.pdf (Accessed: 23 April 2023) ↑26 Ekkehard, M., Joachim, S., Jorn, K., Christiane, O. (2017). Prolactin receptor antibody for male and female pattern hair loss. World Intellectual Property Organization. Available at: https://patentimages.storage.googleapis.com/56/cc/a3/7d3ac32f1537b2/WO2019011719A1.pdf (Accessed: 23 April 2023) ↑27 Clinical Trials, (no date). HMI-115. Available at: https://clinicaltrials.gov/ct2/results?cond=&term=HMI-115&cntry=&state=&city=&dist= (Accessed: 02 May 2024) ↑28 Hope Medicine. (2023). An Open Label Study, to Evaluate Safety, Tolerability, and Efficacy in Male and Female With Androgenetic Alopecia Treated With HMI-115 Over a 24-Week Treatment Period (Clinical Trial Registration NCT05324293). Clinical Trials. (Accessed: 02 May 2024) ↑29 Hope Medicine. (No date). Positive Outcome from a Phase Ib Study in Australia Treating Patients with Androgenic Alopecia. Hope Medicine Available at: https://www.hopemedinc.com/company-release-37 (Accessed 2 May 2024) ↑30 Kelly, J., Sadeghieh, T., Khosrow, A. (2014). Peer Review in Scientific Publications: Benefits, Critiques, & A Survival Guide. eJIFCC. 25(3). 227-243. PMID: 27683470 ↑31 Andrade, C., (2020). Sample Size and its Importance in Research. Indian Journal of Psychological Medicine. 42(1). 102-103. Available at: https://doi.org/10.4103/IJPSYM.IJPSYM_504_19 ↑32 Norman, G.A.V. (2019). Phase II trials in drug development and adaptive trial design. JACC Basic to Translational Science. 4(3). 428-437. Available at: https://doi.org/10.1016/j.jacbts.2019.02.005 ↑33 Nave, R., Jodi, S., Hoffman, A., Gashaw, I., Zollmann, F., Berse, M., Hochel, J., Kratzschmar, J., Rohde, B. (2019). Monoclonal antibody against prolactin receptor: a randomized placebo-controlled study evaluating safety, tolerability, and pharmacokinetics of repeated subcutaneous administrations in postmenopausal women. Reproductive Sciences. 26(4). 523-531. Available at: https://doi.org/10.1177/1933719118776806 ↑34 Clinical Trials, (no date). HMI-115. Available at: https://clinicaltrials.gov/ct2/results?cond=&term=HMI-115&cntry=&state=&city=&dist= (Accessed: 21 April 2023) IngredientsPharmaceuticalsNatural RemediesCompany ReviewsBy Perfect Hair Health TeamNov 4, 20255 Natural DHT Blockers… But Should You Use Them?
Natural DHT blockers are popular among hair loss sufferers who want to lower DHT without the use of drugs. Unfortunately, most natural DHT reducers lack enough DHT-reducing capabilities to regrow hair. This article separates fact from fiction to reveal the best (and worst) natural DHT blockers for p...By Perfect Hair Health TeamSep 24, 2025Topical Dutasteride Before and After: 10 Successes
Recent clinical data show that topical dutasteride offers promising hair regrowth and reduced side effects, but results vary widely, and more research is needed. Learn how to interpret anecdotal stories, set realistic goals, and combine therapies for the best outcomes....By Perfect Hair Health TeamSep 24, 2025Minoxidil Before and After Photos [2025] | Does It Work?
Topical minoxidil is the most widely used hair loss treatment, with decades of clinical evidence supporting its effectiveness. But while many experience stabilization and regrowth, others see little to no change. Learn why minoxidil response is so variable, how to interpret before-and-after photos, ...By Sarah King, PhDSep 18, 2025Does Topical Dutasteride Work?
Topical dutasteride is gaining attention as a potent alternative to oral dutasteride (and finasteride) in treating androgenic alopecia, aiming to deliver robust DHT suppression at the scalp with fewer systemic side effects. But does topical dutasteride work? In this article, we break down how topica...By Sarah King, PhDSep 16, 2025Where to Buy Topical Finasteride?
Topical finasteride is gaining traction as a lower-risk alternative to oral finasteride, especially for those concerned about systemic side effects. In the U.S., providers like Ulo and Strut stand out for customization and lab-tested purity. Canadian options include Xyon Health and Essential Clinic,...By Perfect Hair Health TeamSep 10, 2025Dutasteride Before and After: 10 Success Stories
Oral dutasteride is one of the most powerful treatments for androgenic alopecia, offering deeper DHT suppression than finasteride. But what kind of results should you realistically expect? In this article, we break down how dutasteride works, what clinical studies actually show, how typical outcomes...By Sarah King, PhDJul 31, 2025Where To Buy Topical Dutasteride?
Topical dutasteride is an exciting option in the hair loss arsenal, and sourcing it has become easier with the advent of modern telehealth. The U.S. market offers the greatest flexibility (with Ulo leading in customization and lab‑verified purity). In Canada, Xyon Health and Jupiter provide solid op...By Sarah King, PhDJul 16, 2025Topical Minoxidil for Hair Growth: Efficacy, Safety, and How to Enhance Results
Topical minoxidil is the most established over-the-counter treatment for hair loss, with decades of use behind its FDA approval. But how does it actually work, and what determines whether it will work for you? In this article, we explore the science behind topical minoxidil, its strengths and limita...By Sarah King, PhDJul 9, 2025Oral Minoxidil for Hair Growth: Is it Effective and Safe? Our Analysis
Oral minoxidil, once a blood pressure medication, is now gaining traction as a powerful off-label treatment for hair loss. But how does it compare to topical minoxidil, and is it safe? In this article, we explore the mechanisms behind oral minoxidil’s hair growth effects, its role in treating differ...By Perfect Hair Health TeamJul 8, 2025Introducing Ulo: The Future of Hair Loss Telemedicine
Ulo is a new telehealth brand focused exclusively on hair growth. With its commitments to evidence, personalization, & consumer safety, the company aims to provide best-in-class products that have not only been independently lab tested, but also offer a level of customization unrivaled by other ... - Mission Statement
 Scroll Down
Scroll Down







































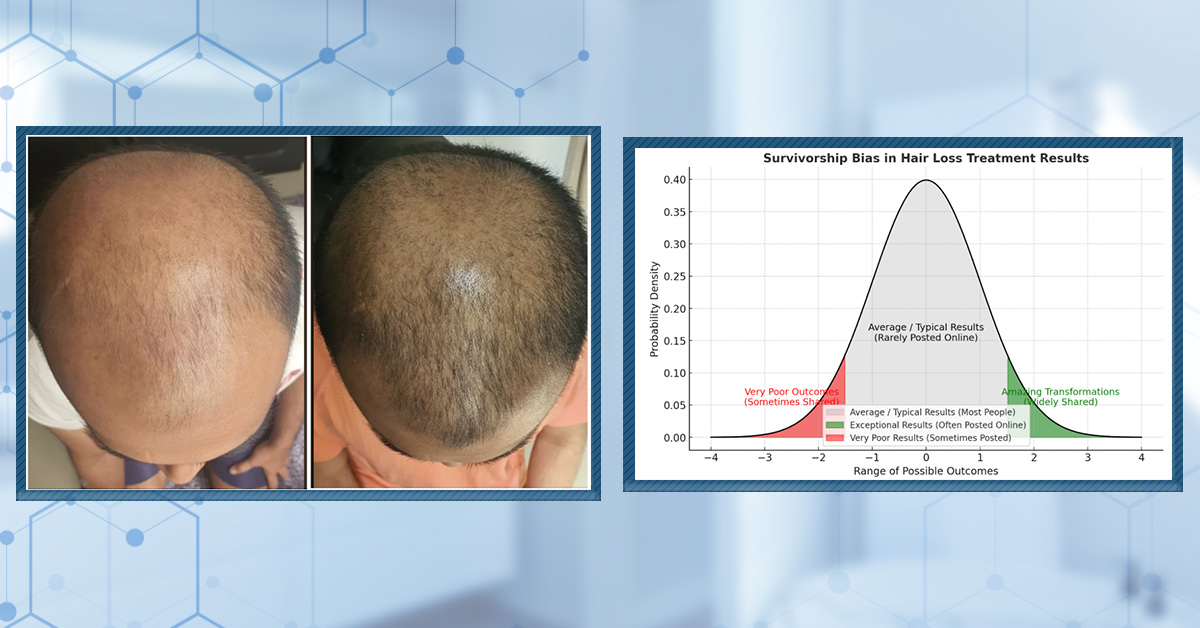
![Minoxidil Before and After Photos [2025] | Does It Work?](https://perfecthairhealth.com/wp-content/uploads/2025/09/92-TM.jpg)