Scarring alopecias make up about 7% of patients seen in hair loss clinics. This means almost 1 in 10 hair loss cases are attributed to scarring alopecia.
In this article, we’ll outline what scarring alopecias are, what makes them unique, and why they might develop. Then we’ll uncover why this classification of hair loss – scarring vs. non-scarring – might be a bit outdated.
Finally, we’ll reveal new research that’s changing the way we think about scarring forms of hair loss. Historically, scarring alopecias have been considered irreversible. But new case reports are showing just the opposite: that some people with scarring alopecias can achieve significant – and sometimes complete – hair regrowth.
We’ll dive into why this is important, how this may impact treatment avenues, and what you can do to start combatting the progression of scarring alopecias today, both naturally and conventionally.
What are scarring alopecias?
Scarring alopecias are an umbrella term for hair loss from the rapid destruction and scarring of hair follicles.
There are several types of scarring alopecias (1), and each type varies by its presentation and causes:
- Central centrifugal cicatricial alopecia (CCCA). A type of hair loss that occurs predominantly in African American women. Characterized by a progressive thinning that begins in the center of the scalp and gradually expands to the peripheral regions. The only feature that distinguishes it from female pattern hair loss is the lack of visible follicles in the affected areas and a shiny, smooth scalp. It was once believed to be caused by hair styling techniques; however, recent data (2) has refuted that claim.
- Frontal fibrosing alopecia. This type of scarring alopecia occurs in a band-like distribution in the front of the hair and may also be present in the eyebrows. It mostly affects postmenopausal women. It predominantly affects the hairline, leading to uniform recession as if the hairline marched backward.
- Lichen planopilaris. Patchy hair loss with itchiness, scaling, and visible redness in affected areas. It might also affect non-scalp areas. It sometimes presents as diffuse thinning.
- Chronic cutaneous lupus erythematosus. Patchy, scarring hair loss as a result of an autoimmune disorder: lupus. Onset of this type of scarring alopecia may result from UV exposure, though research hasn’t yet confirmed this.
- Pseudopelade of Brocq. Small and/or large irregular patches of hair loss with no signs of inflammation.
- Folliculitis decalvans. A single patch of hair loss that progressively expands. Typically found on the peripheral regions of the scalp. Affected areas may have pustules, honey-colored crusting, and tufting.
- Dissecting cellulitis of the scalp. Multiple, red, inflamed, and interconnected nodules that erupt from various scalp regions in somewhat of a web-like pattern. It may also be associated with acne conglobota.
How do scarring alopecias happen?
No one is quite sure. However, many researchers believe scarring alopecias are caused by an interaction between inflammation, our immune systems, and (potentially) our hormones.
Similar to other hair loss disorders, the step-process for developing a scarring alopecia seems to be:
Inflammation >> scarring >> hair loss
You might see this step-process and think it looks a lot similar to other hair loss disorders, like androgenic alopecia (AGA). At face-value, you’re right. But there are a few differences that make scarring alopecias unique.
- In scarring alopecias, the location of inflammation is in the hair follicle stem cell bulge; in androgenic alopecia, it’s in the infundibulum (upper third of the hair follicle) and likely deeper below the hair follicles, but above the galea aponeurotica.
- In scarring alopecias, the nature of inflammation in unknown and/or autoimmune-related; in androgenic alopecia, the inflammation is likely related to scalp tension, pathogenic microorganisms, and accelerated hair cycling.
It might seem absurd to distinguish scarring alopecias from androgenic alopecia by the nature and location of inflammation. After all, our hair follicles are already tiny “mini-organs”. What difference does it make if one hair loss disorder’s source of inflammation is just a couple of nanometers away from another’s?
Apparently, a lot. And this is because across hair loss disorders, the location of inflammation predicts where scarring will occur, which predicts what these hair loss disorders will end up looking like.
This is why, in the later stages, androgenic alopecia and scarring alopecias look so different:
With scarring alopecias, the inflammation is far more widespread, so the scarring ends up wiping out the entire hair follicle – the stem cell bulges, sebaceous glands, arrector pili muscles, and hair shaft.
In androgenic alopecia, the scarring remains clustered around the hair follicle. Subsequently, the scarring doesn’t wipe out these other components of our hair follicles until many years into AGA’s progression.
In scarring alopecias, why do a hair follicle’s stem cell bulges become inflamed?
No one is quite sure. While researchers have identified dozens of potential triggers (3) across patients with scarring alopecias…
- Sebaceous gland dysfunction
- Substance P transmission (a neuropeptide released during stress)
- Deficiency in PPAR signaling
- Collapse of hair follicle immune privilege (the hair follicle is generally resistant against to damage by the immune system)
- Bacterial infection
- Abnormal cellular changes
- Genetic factors
- Hairstyling
- Certain drugs (anticonvulsants, hepatitis B vaccine, cyclosporin)
- Autoimmunity
- Sunscreen use on the forehead
…It’s still unclear which causes might apply to each case, why our hair follicle’s stem cell bulges become inflamed, and why this inflammation becomes persistent in the first place.
It all seems to begin with a miscommunication between an inflammatory stimulant, our immune systems, and our hair.
The miscommunication: inflammatory stimulants, myofibroblasts, and beyond
During a normal inflammatory process, the body encounters some sort of inflammatory stimulus – a wound, a virus, or even an environmental irritant. This stimulus is identified by the immune system as foreign, at which point our immune system recruits cells to “attack” the foreign invader. This leads to inflammation (i.e., tissue swelling), which in many cases, is enough to kill off the foreign invader. Once the threat is gone, the immune system signals these cells to stop attacking, and the inflammation dissipates, leaving us the same as we were prior to the attack.
In scarring alopecias, this process does not go according to plan.
During scarring alopecias, our immune system picks up on a foreign threat and sends a group of cells called myofibroblasts to start attacking. These myofibroblasts have a number of roles in the body – three of which are (1) enhancing the inflammatory response, (2) supporting the healing process, and (3) producing proteins like collagen (which, if produced in a disorganized fashion, form the building blocks of scar tissue).
Under normal settings, myofibroblasts would help enhance the inflammatory response until the foreign threat is destroyed, at which point the myofibroblasts would no longer be needed. At this point, the myofibroblasts would then help to repair the damage caused by inflammation by laying down new collagen fibers (i.e., skin tissues). Then, these myofibroblasts would die off.
However, in the case of scarring alopecias, myofibroblasts fail to die off. To put it simply, there’s a disruption in the normal cell signaling that tells our myofibroblasts that they’re no longer needed. As a result, they continue to lay down collagen, which becomes excessive and disorganized, which then turns to scar tissue.
Subsequently, functional tissue begins to be replaced by poorly-functioning scar tissue. As the fibrosis continues, the affected organs continue to lose functionality. We see this in conditions like cirrhosis, scleroderma, and pulmonary fibrosis (fibrosis of the lungs) – for example, where fibrosis makes it difficult for the liver, skin, and lungs to do their job.
This is exactly what happens in the hair follicle during scarring alopecia.
Infection and sustained inflammation begin to severely damage the hair follicle. And unfortunately, this scarring process ends up destroying our hair follicle stem cell bulges. This stem cell bulge is incredibly important; it contains the “blueprints” – or the building blocks – of each hair follicle. And without a hair follicle stem cell bulge, our hair follicles have no blueprints to follow for replication.
This leads to the complete destruction of the hair follicle… and the scarring of its surrounding skin. And as you can imagine, this is not a position most hair loss sufferers want to be in.
Are scarring alopecias reversible?
Traditionally, researchers have generally held the stance that scarring alopecias aren’t reversible.
This is because of the fact that scarring alopecias (1) lead to widespread scarring of an entire skin region, and thereby (2) wipe out the hair follicle stem cell bulges. For these reasons, many researchers have held onto the belief that scarring alopecias are irreversible – and that the best we can do is slow or stop their progression.
Encouragingly, this belief is now changing. Why? Because new evidence is showing that scarring alopecias are not only theoretically reversible, but that we actually have case studies of this happening. It’s all a matter of unlocking how to do it on a consistent basis.
Here’s why we believe this is possible.
#1: AGA, which also leads to scarring, is reversible even in its latest stages.
To reiterate from earlier, end-stage AGA closely resembles that of end-stage scarring alopecias. In both conditions, we see so much fibrosis (scarring), that there’s a total loss of follicular integrity.
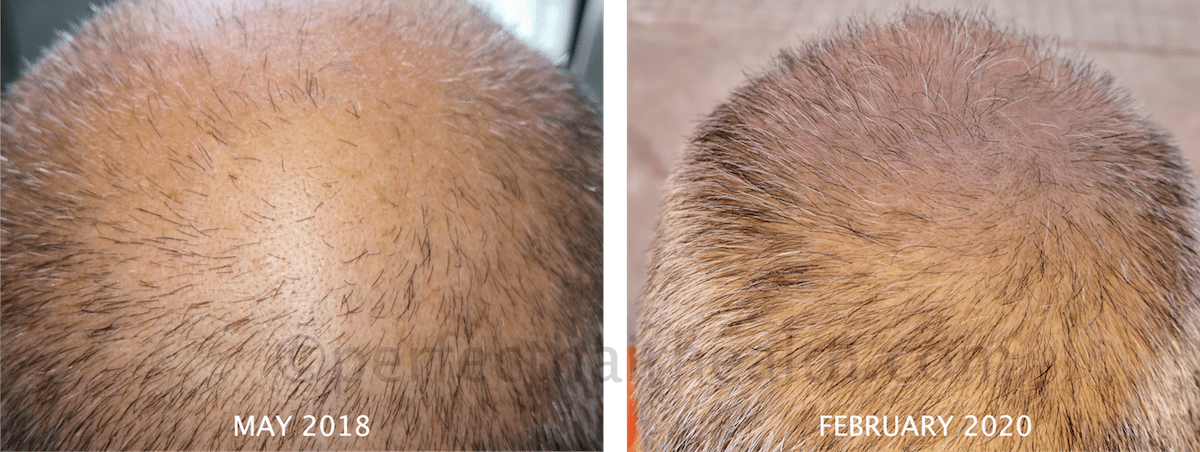
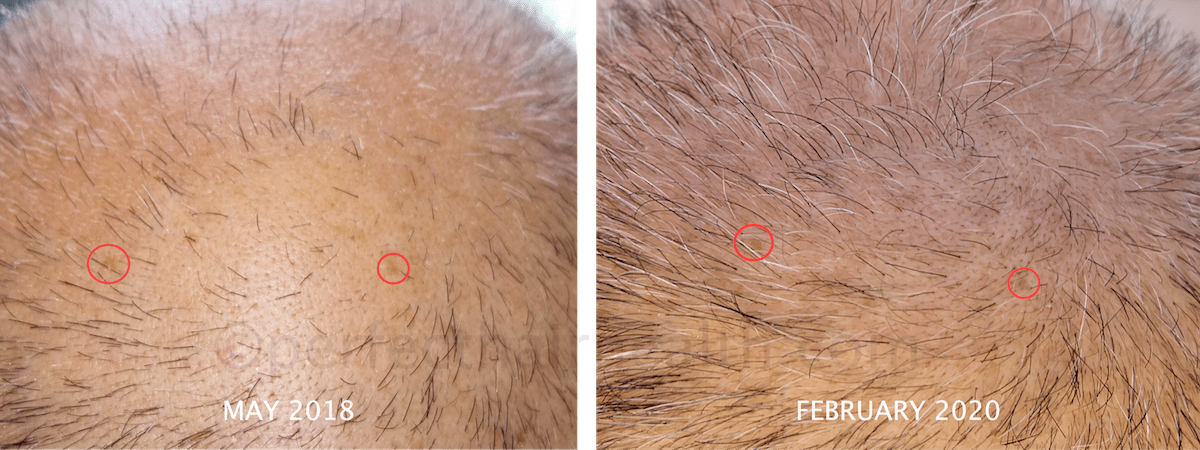
Having said that, even in late stages of androgenic alopecia, we’ve seen pretty significant hair regrowth. This is obvious with examples from a few of our case studies from our membership community – like Mike and Raul – who used natural methods to see regrowth beyond what is typically observed with conventional treatments.
Mike’s Regrowth
Raul’s Regrowth
But perhaps the most impressive example of hair regrowth from advanced AGA happened entirely by accident.
In 1986, a 78-year man who’d been bald for 30+ years fell asleep in his rocking chair. Inadvertently, he slumped over, landed head-first onto hot coals, and received second degree burns across much of his scalp.
He refused to be treated at the hospital and was eventually sent home as an outpatient. Four months later, he returned for a checkup. During that time from the injury, he’d accidentally regrown his entire juvenile hairline (4).
Remember: in advanced cases of AGA, a hair follicle’s stem cell bulges appear either scarred or completely depleted. This implies an inability for hair recovery. Yet here, we see a case of complete hair recovery… just the opposite of what we’d expect.
And as we dig deeper into the research on scarring alopecias, we can find plenty of cases where recoveries happen, too.
#2: scarring alopecias have been reversed before!
There are several case studies of people with scarring alopecias regrowing significant amounts of hair. In some cases, the hair recovers completely.
In some cases, this has happened with interventions as simple as stopping the use of facial sunscreen (5). In other cases, significant regrowth came after using topical metformin (6). In one case of lupus-related scarring alopecia, complete hair regrowth was observed within three months following the use of hydroxychloroquine (7). And in cases of frontal fibrosing alopecia, oral finasteride led to near-complete hairline regrowth after just 12 months (8).
In light of these findings, there are really only two explanations:
- In scarring alopecias, stem cell bulges aren’t totally lost. Therefore, the hair is still recoverable. Or…
- Our understanding of hair follicle stem cell bulges needs to be revised. Maybe hair follicles can regenerate in the absence of stem cells, and through not-yet-discussed processes, like that of follicle-to-follicle communication.
Let’s explore that second idea for a second, as it may shape the next decade of hair loss research.
What do we know about follicle-to-follicle communication?
Follicle-to-follicle communication is a phenomenon that was originally observed in one fascinating study (9) – the findings of which we described in this article. To summarize:
In 2015, researchers wanted to see if hair follicles could communicate with each other to coordinate behaviors – like making new hair follicles. So they set up a test…
They plucked 200 hairs from the backs of mice… but did so while controlling for the diameter of a plucking region. In some cases, 200 hairs were plucked in a 2.4mm region. In other cases, 200 hairs were plucked from an 8mm region. The smaller the region, the higher-density the plucking – and vice-versa.
The goal: to see if hair follicle behavior changed on how closely hairs were plucked from one another. So they measured hair growth over the next several weeks.
The results were fascinating.
With low-density plucking, hair follicles either didn’t grow back at all… or grew back to their normal pre-plucking densities. That’s what we would expect to happen.
But with higher-density plucking, additional hair follicles were created… to the tune of a five-fold increase.
What’s more interesting is why this happened. The researchers theorized that higher-density plucking created more inflammatory signaling, which led to more cross-communication between hair follicles directly next to each other, which signaled to hair follicles to start regenerating – regardless of whether they’d been plucked.
The end-result: a huge increase in hair.
The implications? That nearby hair follicles can communicate with one another (!), and that these communications must include signaling for hair follicle regeneration. Based on this study, it’s clear that healthy hair follicles can coordinate regeneration with damaged hair follicles.
So, how does this relate to scarring alopecia?
Considering hair loss from scarring alopecia is a result of complete hair follicle destruction, and considering that this destruction has puzzlingly reversed itself across many case studies…
We can presume that follicle-to-follicle communication is playing a role here, and that understanding this role (and harnessing this cellular crosstalk) is probably one way people with scarring alopecias can unlock huge hair recoveries.
So, how do we do this?
We don’t yet know! Research is still emerging, and as it continues to evolve, we’ll update this article.
In the meantime, there’s plenty we can do to stop the progression of scarring alopecias – and potentially even see major recoveries.
What are the current treatments for scarring alopecias?
Step 1: connect with a dermatologist
The first step is always making an appointment with a dermatologist. By understanding what kind of scarring alopecia you have, you can better target your treatment regimens to save yourself time, effort, and money.
Step 2: identify and remove any potential inflammatory “triggers”
Once you’ve scheduled your appointment, one of the most critical next steps is to make your best effort to identify and remove some of the most common triggers of scarring alopecias. This will be highly individual and dependent, again, on the type of scarring alopecia with which you’re diagnosed.
Here are a few of the common inflammatory stimulants suspected in scarring alopecias:
- Sunscreen use: there is a weak link between sunscreen use and frontal fibrosing alopecia (FFA) (5). Some researchers hypothesize this could be due to decreased sebum production during the time in which a woman is most likely to be affected by FFA, menopause. This results in an inability to clear topical products, like sunscreen, from the follicle, potentially leading to an autoimmune reaction. Other researchers have proposed an alternate view: with the anti-inflammatory, immunomodulatory effects of UV light, blocking UV light (using sunscreen) may actually encourage autoimmunity in the follicle. Cessation of sunscreen use has been shown to produce noticeable regrowth in as little as 6 months with an almost full recovery in 36+ months.
- Hairstyling: While studies have failed to establish hairstyling as the sole cause of CCCA, certain hairstyling techniques may contribute to at least some cases of scarring alopecia. If you find yourself dealing with a potential case of scarring alopecia and you regularly receive hair relaxant treatments, employ hot combing, or style your hair in braids, cornrows, or using other traction styling methods (10) – it might be best to avoid these treatments and/or stylings (or at least reduce their frequency) until you can rule out their potential involvement.
- Environmental toxins as inducers of autoimmunity: Autoimmunity is one of the purported causes underpinning the development of scarring alopecia. This is due to the fact that the stem cell bulge of the follicle is normally a site of immune privilege, meaning it is usually protected from the action of the immune system. However, autoimmune processes can actually cause this immune privilege to be lost. Interestingly, environmental toxins have the ability to induce autoimmunity. For this reason, avoidance of environmental triggers linked to autoimmunity, like rancid vegetable oils, mineral oils, and sources of heavy metals, is a good precautionary measure (11).
- UV exposure: Some causes of scarring alopecia, like chronic cutaneous lupus erythematosus, are exacerbated by UV exposure. Use of sunscreen or UV-blocking clothing/hats may be needed to prevent the worsening of lesions that contribute to hair loss.
Step 3: settle on a treatment approach
There are two ways we can approach this: drug-based treatments and non-drug treatments.
We’ve divided these interventions into their respective sections and described who these treatments might be best for, which dosages are used in the literature (where applicable), the outcomes of the research, and what potential issues might arise with each given treatment.
Drug-based treatments
Topical, intralesional, and oral corticosteroids:
- Best candidates: Most forms of scarring alopecia, patients with CCCA not related to traumatic hair styling.
- Dosages: 10mg/mL for intralesional injections every 6-8 weeks; 25-40mg per day for 2-4 months with oral corticosteroids (1).
- Outcomes: Corticosteroid treatment, in any form of administration is mostly limited to halting the progression of disease as it doesn’t address the scarring that impedes hair follicle regeneration. Can promote regrowth in some patients with dissecting cellulitis (12).
- Problems: Oral corticosteroids are limited to severe/rapidly progressing disease; topical corticosteroid treatment can result in skin atrophy, a.k.a thinning of the skin.
Hydroxychloroquine:
- Best candidates: Patients with frontal fibrosing alopecia, lichen planopilaris, and chronic cutaneous lupus erythematosus.
- Dosages: Below 7.5/mg/kg for lichen planopilaris and frontal fibrosing alopecia, 400mg daily during summer months with chronic cutaneous lupus erythematosus and smaller doses during winter (1).
- Outcomes: Effective at decreasing signs and symptoms of lichen planopilaris and frontal fibrosing alopecia and preventing further hair loss, effectively resolve lesions related to chronic cutaneous lupus erythematosus (13), full hair regrowth has been observed with hydroxychloroquine in at least one case of lupus-related alopecia (7).
- Problems: Studies are often too short to estimate the true incidence of retinopathy at dosages used for these conditions.
Antibiotics (Minocycline, rifampicin, fusidic acid):
- Best candidates: Patients with folliculitis decalvans.
- Dosages: 300mg rifampicin 2x daily (should not be used as a monotherapy, which can promote antibiotic resistance), combination of 300mg rifampicin, 300mg clindamycin, and fusidic acid along with topical corticosteroid lotion for 3 months has been used with success, topical clindamycin or benzoyl peroxide can control mild cases, oral antibiotics are needed for more severe cases (1).
- Outcomes: Effective at addressing the infection that leads to folliculitis decalvans, but not restoring the hair lost.
- Problems: Rifampicin is the preferred antibiotic because it is highly lipid-soluble (the scalp environment is very lipidic) and accumulates in high quantities in the hair follicle, however, antibiotic resistance is a major issue with its use.
Topical metformin:
- Best candidates: Who topical metformin might be best for is still unclear, as research is preliminary, but case studies have demonstrated success in CCCA patients (6).
- Dosages: 10% topical metformin with the potential for higher concentrations if the patient responds well to the treatment.
- Outcomes: Although research is preliminary, there have been two cases of partial regrowth in CCCA – traditionally believed to be irreversible (and notoriously difficult to treat) (6).
- Problems: Preliminary research suggests there is little to no systemic side effects. Instead, side effects are usually superficial and limited to scalp dryness and irritation.
Oral Isotretinoin (Accutane®):
- Best candidates: Patients with dissecting cellulitis and cases of chronic cutaneous lupus erythematosus resistant to antimalarial therapies like hydroxychloroquine.
- Dosages: 0.5-1mg/kg daily for dissecting cellulitis (1).
- Outcomes: Usually produces rapid results in chronic cutaneous lupus erythematosus, treatment for 6-11 months in dissecting cellulitis shrinks lesions and can even induce periods of long remission.
- Problems: Oral isotretinoin can cause large quantities of hair follicles to prematurely enter the telogen phase, which can lead to diffuse shedding (1). The risk of disease progression should be weighed carefully against the potential risk of increased shedding.
Finasteride:
- Best candidates: Patients with frontal fibrosing alopecia.
- Dosages: 2.5mg daily (14).
- Outcomes: Some studies suggest finasteride is the most effective therapy for treating frontal fibrosing alopecia. Patients with this condition can expect a response rate of about 50% with finasteride alone (14). At least one case report demonstrated marked regrowth and a reversal of skin atrophy (i.e., skin thinning) (8).
- Problems: In women with already low or normal androgen levels, finasteride could produce sexual/mental side effects.
Non-drug treatments
Microneedling + platelet-rich plasma:
- Best candidates: Unknown.
- Methods: 20 sessions spaced 2 weeks apart.
- Outcomes: Clinical improvement in one case of general scarring alopecia – the details of this clinical improvement aren’t specified (i.e., improvement of inflammatory lesions vs. actual hair regrowth)
- Problems: Likely cannot be used to treat some forms of scarring alopecia like folliculitus decalvans, at least in their active infection phase, due to the bacterial nature of the condition.
Low level light/laser therapy (LLLT):
- Best candidates: Patients with lichen planopilaris.
- Methods: 272 pulsed laser diode cap with 1360 mW total output
- Outcomes: Case reports suggest lichen planopilaris patients may be able to achieve hair regrowth with the use of LLLT (15).
Excimer laser (UV-B light)
- Best candidates: Patients with lichen planopilaris and some cases of frontal fibrosing alopecia.
- Methods: Sessions as frequent as twice weekly with an average of 10 sessions reported in the literature.
- Outcomes: Studies have demonstrated a decrease in inflammation, as well as some instances of hair regrowth (16).
Hair Transplants
We know from the literature that there are some cases of scarring alopecia that are reversible. But, what if your hair doesn’t grow all the way back, even with the best-of-the-best treatment?
This is where hair transplants might be useful.
Hair transplants in scarring alopecias are different than hair transplants for non-scarring hair loss disorders. While grafts in non-scarring alopecias have a 90% survival rate, scarring alopecias may only have an average 50% survival rate.
But, transplants don’t have to be a stab in the dark. We can usually predict whether or not a transplant is going to be successful by (1) understanding what kind of scarring alopecia you have, and (2) performing a pre-surgery transplant test.
We’ve compiled the types of scarring alopecias that are more likely to see success from a transplant vs. those that might not:
|
Scarring alopecias more likely to receive transplants successfully |
Scarring alopecias where hair transplants are less likely to survive |
| Central centrifugal cicatrial alopecia (CCCA) | Lichen planopilaris |
| Discoid lupus erythematosus | Frontal fibrosing alopecia |
| Pseudopelade brocq | |
| Folliculitis decalvans |
However, the safest way to estimate your individual tolerance to a hair transplant is to have a dermatologist perform a pre-surgery transplant test.
But, what if your chances of hair transplant survival end up being low? Or what if hair transplants are too expensive? Or too invasive? What are the options, then?
In these cases, there is one additional option.
Artificial hair integrations
For treatment-resistant and/or transplant-intolerant cases or for those who aren’t comfortable with the price or the procedure, the next best option is artificial hair integrations.
The good news is that these are inexpensive and readily accessible – and something you can begin to use right away. But, you’ll want to be absolutely sure that these integrations aren’t putting any additional strain on existing hair, as this can do more harm than good. In some cases, it may trigger a case of traction alopecia or, worse, a new case of scarring alopecia.
So, to recap, here’s a sequential approach you should consider for treatment:
- Make a dermatologist appointment to identify what kind of scarring alopecia you might have (if any).
- Identify and remove any potential triggers.
- Based on what type of scarring alopecia you have, explore some treatment avenues provided and discuss them with your dermatologist.
- If you aren’t able to achieve full recovery, explore hair transplants. Performing a pre-surgery transplant test can help you gauge whether or not a transplant will survive on your scalp.
- If you are intolerant to transplants and/or aren’t comfortable with the price or the procedure itself, artificial hair integrations are relatively inexpensive and very accessible.
Summary
Scarring alopecias are relatively uncommon; they constitute just 7% of hair loss diagnoses in hair loss clinics. Having said that, they’re characterized by aggressive scarring. This scarring leads to the destruction of skin tissue surrounding hair follicles, as well as the destruction of stem cell bulges which make hair follicles and the hair follicles themselves. Consequently, many researchers have historically considered that scarring alopecias are irreversible.
This is no longer the case. Case reports of full hair recoveries from scarring alopecias, alongside evidence that healthy hair follicles and unhealthy hair follicles can actually communicate with each other, now leads researchers to believe that scarring alopecias are reversible… we just don’t know how to do it consistently (yet).
Because scarring alopecias are less common, there are still many questions researchers have yet to answer:
- Why are some cases of scarring alopecias reversible, if all scarring alopecias are believed to result in a loss of the stem cell bulge?
- If there are at least some scarring alopecias that happen to retain stem cells, could there be an overlap in treatments with AGA? In other words, could some scarring alopecia patients benefit from AGA treatments that address fibrosis?
- If stem cells aren’t retained, is there some other regenerative process, like follicle-to-follicle communication, at play?
As researchers attempt to answer these questions, there are still some great treatments out there for scarring alopecia patients – both drug-based and drug-free, that have shown clear benefit. While most are limited to improving symptoms and slowing or halting the progression of hair loss, some patients are seeing partial and/or full recoveries.
For those who find their hair loss is treatment-resistant or want to restore hair lost to scarring alopecia, hair transplants are a decent option. However, they can be a hit or miss, being that the transplant survival rate is around 50% (vs. 90% for other hair loss types). You can maximize your chances of survival by identifying what kind of scarring alopecia you’re dealing with as well as performing a pre-surgery transplant test.
Artificial hair integrations are also a great option — and one much cheaper and more accessible than hair transplants. However, it is of the utmost importance that these are applied correctly to avoid undue strain on healthy hair (which may trigger the onset of new hair loss).
Have any questions about the new treatments for or emerging research on scarring alopecia? Please let us know in the comments section below.

Rob English is a researcher, medical editor, and the founder of perfecthairhealth.com. He acts as a peer reviewer for scholarly journals and has published five peer-reviewed papers on androgenic alopecia. He writes regularly about the science behind hair loss (and hair growth). Feel free to browse his long-form articles and publications throughout this site.







Rob, have a question to ask you, I am keloid constitution, can you use massage micro needle this method, if you can reply, thank you very much
Hey Wang,
Thank you for reaching out. Those who tend to experience keloid scars are, in general, advised against trying stimulation-based therapies like microneedling, massaging, platelet-rich plasma, etc. The reason why is because these therapies leverage acute inflammation generation, which for highly sensitive individuals, may increase scarring rather than prevent it (the opposite intended effect). Even still, there are a lot of other options out there for you – DHT reducers, minoxidil, etc. So I wouldn’t feel too disappointed about having a contraindication that prevents you from these therapies alone.
Best,
Rob
Thank you rob, my personal information has been sent to your email, I am a keloid patient, but I want to restore my hair, please reply me when you are free.
Hi, thanks for this great article about these fascinating mechanisms! One question – you mention at some point that inflammation in AGA can be caused by accelerated hair cycling. Do you have any article about that, and what is causing the accelerated hair cycling then?
Hey RMousquetaire,
Thanks for the kind words. And yes! We’ve got an article about AGA that touches upon accelerations to hair cycling. You can read it here.
Otherwise, we’ve got an article about the hair cycle and its relationship to different hair loss disorders – which we’ll be releasing soon. It’s still going through our informal peer-review process.
Best,
Rob
Thank you for writing this article.
If you say that frontal alopecia is a result of scarring just like androgenic alopecia, then why is detumescence therapy not also a viable solution? Also do you think that scalp massages can somehow control DHT levels in the scalp since it is evident that it can regrow hair?
Hi Rob thanks for the great insights. In your rosemary article, you stated that is reduce fibrosis, so would it help to use rosemary oil for scarring alopecia? Would it be safe to microneedle on scaring alopecia bald spot?
Also, what are you thought on trichodynia or scalp dysthetia? Thanks rob.