- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
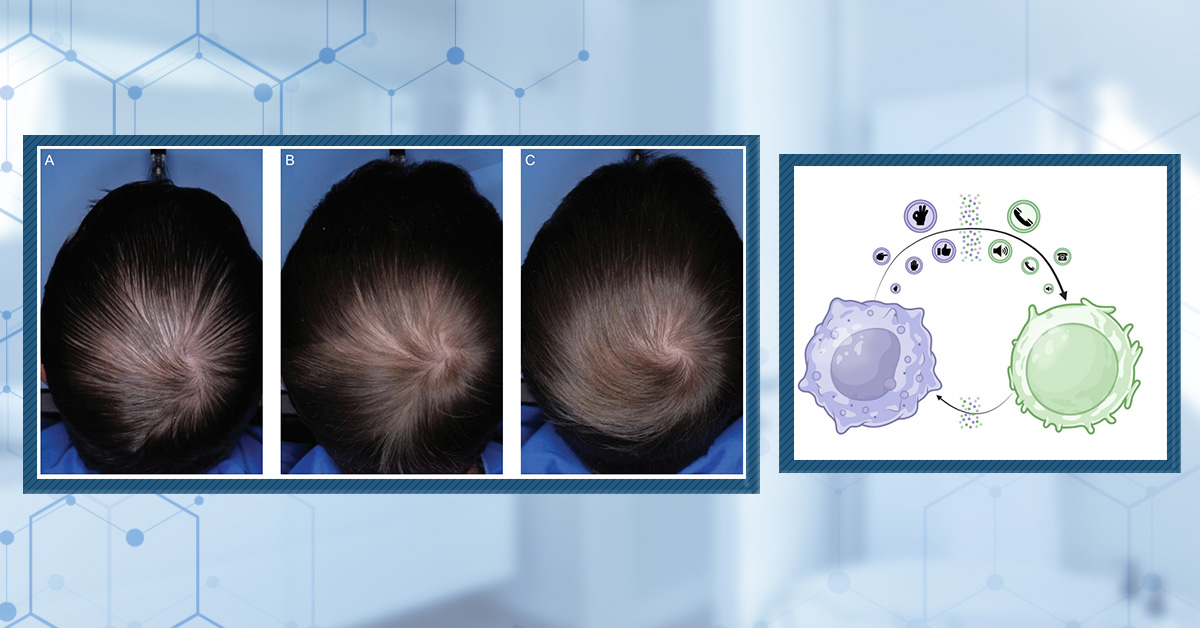
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
Scroll Down
Popular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Free CalculatorTopical Finasteride Calculator
- Free Interactive GuideInteractive Guide: What Causes Hair Loss?
- Free ResourceFree Guide: Standardized Scalp Massages
- Free Course7-Day Hair Loss Email Course
- Free DatabaseIngredients Database
- Free Interactive GuideInteractive Guide: Hair Loss Disorders
- Free DatabaseTreatment Guides
- Free Lab TestsProduct Lab Tests: Purity & Potency
- Free Video & Write-upEvidence Quality Masterclass
- Free Interactive GuideDermatology Appointment Guide
More
Articles100+ free articles.
-
Hims Hair Growth Reviews: The Pros, Cons, and Real Results
-
Topical Finasteride Before and After: Real Case Studies
-
How to Reduce the Risk of Finasteride Side Effects
-
10 Best DHT-Blocking Shampoos
-
Best Minoxidil for Men: Top Picks for 2026
-
7 Best Oils for Hair Growth
-
Switching From Finasteride to Dutasteride
-
Best Minoxidil for Women: Top 6 Brands of 2026
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
Before-Afters- Transformation Photos
Our library of before-after photos.
- Client Testimonials
Read the experiences of members
Before-Afters/ Client Testimonials- Popular Treatments
-
Articles
Pyrilutamide, also known as KX826, is an anti-androgenic drug with a mechanism of action similar to that of flutamide, albeit with potentially fewer side effects. Developed as a treatment for both androgenic alopecia and acne vulgaris, pyrilutamide is currently in phase III clinical trials in China and phase II clinical trials in the US. KX-826 is also included as the core ingredient of an anti-hair loss “cosmetic”, which is now being sold globally. In this ultimate guide, we’ll examine the available data on pyrilutamide: what it is, how it works, what the clinical studies show, and whom it might benefit.
Key Takeaways
- Drug. Pyrilutamide is an androgen receptor antagonist developed for treating androgenic alopecia and acne vulgaris. Topical pyrilutamide has completed phase III trials in China and phase II trials in the US and has recently gained approval for a trial using pyrilutamide in combination with minoxidil in China.
- Clinical Data. There have been five as yet unpublished trials that were conducted in either China or the US. We only have information about these trials from press releases or conference poster presentations. The key information we do have is bulleted below:
- A 24-week trial with 160 women with female pattern hair loss was conducted in China. The participants were randomized to six treatment groups (0.25% pyrilutamide applied once daily, 0.25% applied twice daily, 0.5% applied once daily, 0.5% applied twice daily, or two placebo groups – once daily and twice daily treatments). The 0.5% once-daily treatment appeared to perform the best, with an increase of 11.39 hairs per cm2 from the baseline compared to the placebo groups.
- A 24-week trial with 120 men with male-pattern hair loss was conducted in China. During the trial, the participants were randomized to four treatment groups (0.25% pyrilutamide applied twice daily, 0.5% applied once daily, 0.5% applied twice daily, or a placebo). This time, the 0.5% twice-daily treatment appeared to perform the best by the end of the 24 weeks, with an increase of 15.34 hairs per cm2 from the baseline compared to the placebo groups.
- A 24-week phase 1 trial investigating the safety, tolerability, and pharmacokinetics of pyrilutamide was conducted in the US. 40 men aged 18-60 with male-pattern hair loss were treated with ascending dose treatments of pyrilutamide (0.3%, 1.2%, 4.8%, and 9.6%). The study showed that the only reported adverse effects were mild contact dermatitis. Furthermore, pyrilutamide treatment was found to have a low risk of systemic effects, with low concentrations found in the blood after treatment.
- A 24-week phase 2 trial investigating the efficacy and safety of pyrilutamide was conducted in the US. 123 male patients with male-pattern hair loss were treated with either 0.25% once daily, 0.5% once daily, or 0.5% twice daily. The study showed that pyrilutamide improved hair counts by 10 hairs per cm2; however, no significant improvement was observed compared to the placebo.
- A 24-week phase 3 trial investigating the efficacy and safety of pyrilutamide was conducted in China. The participants were treated with either 0.5% pyrilutamide or a placebo. Similar to the phase 2 trial above, the study showed that pyrilutamide significantly improved hair counts compared to the baseline, however, no significant improvement was observed compared to the placebo.
- Evidence Quality. Pyrilutamide scored 37/100 for evidence quality by our metrics.
- Safety. Based on the information available, topical pyrilutamide treatment appears to be well-tolerated. However, none of the studies have been published, and there is the possibility that important information might have been omitted from the data that is available.
- Best Practices. From the limited data available, a concentration of 0.5% pyrilutamide (once daily for women and twice daily for men) appears to be the most effective pyrilutamide treatment regimen. It appears to be a well-tolerated treatment for androgenic alopecia.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is Pyrilutamide?
Pyrilutamide (also known as KX-826) is a topical nonsteroidal antiandrogen (NSAA) drug developed by Kintor Pharmaceuticals. It was developed as a treatment for androgenic alopecia and acne vulgaris, and the drug is currently undergoing phase III trials in China and phase II trials in the US.
Figure 1: Pyrilutamide molecular structure. Adapted from:[1]Pubchem, (no date). Pyrilutamide. NIH. Available at: https://pubchem.ncbi.nlm.nih.gov/substance/469676781 (Accessed: 04 May 2023)
What is the Link Between Pyrilutamide and Pattern Hair Loss?
Testosterone and dihydrotestosterone (or DHT) are androgens that have been implicated in pattern hair loss. To exert their effects, androgens must bind to the androgen receptor, and although the exact mechanisms are unknown, activating the androgen receptor in certain types of hair follicles appears to cause them to undergo miniaturization and eventually cause total hair loss.[2]Trueb, R.M., (2021). Understanding pattern hair loss-hair biology impacted by genes, androgens, prostaglandins, and epigenetic factors. Indian Journal of Plastic Surgery, 54(4). 385-392. Available … Continue reading Because pyrilutamide binds to and blocks the androgen receptor, in theory, it should help to prevent the negative effects of androgens on hair follicles.
How Does Pyrilutamide Work?
Pyrilutamide works in a different way than other anti-androgenic drugs, such as finasteride or dutasteride. Instead of inhibiting the enzyme 5α-reductase that catalyzes the conversion of testosterone to dihydrotestosterone, it competitively binds to the androgen receptor. This stops dihydrotestosterone and testosterone from binding to the receptor and exerting their effects.[3]Kintor, (2021), Kintor Pharmaceuticals Announced Successful Dosing of the First Batch of Patients for Acne Vulgaris Phase I/II Clinical Trial of Pyrilutamide. News Center. Available at: … Continue reading
Does Pyrilutamide Work to Regrow Hair?
There are currently no published data demonstrating the effects of pyrilutamide on hair loss; however, Kintor Pharmaceuticals has made some press announcements where they mention results from their clinical trials.
Study 1
The first study, looking at female androgenic alopecia, was a 24-week, multi-center, randomized, double-blind, placebo-controlled phase II trial conducted in China.[4]Cision PR Newswire, (2022), Kintor Pharma Announced the Primary Endpoint of Phase II Clinical Study for KX-826’s Treatment of Female Androgenetic Alopecia in China was Met. Available at: … Continue reading 160 female participants were randomly assigned to six treatment groups, including 0.25% pyrilutamide applied once daily, 0.25% applied twice daily, 0.5% applied once daily, and 0.5% applied twice daily, or placebo groups (one group for once daily, and one group for twice daily). The primary measured outcome was the change in hair growth, as measured by target area non-vellus hair count (TAHC). Essentially, the researchers were counting the number of thick, pigmented hairs (or ‘terminal’ hairs) in a given area, as opposed to the number of fine, unpigmented (vellus) hairs.
The researchers determined that the recommended dose for their phase III trial in China is 0.5% once daily, as it increased hairs by 11.39 counts per cm2 from baseline, compared to the placebo group. Furthermore, the researchers said that efficacy was seen as early as the end of week 12 of treatment. When it came to safety, the researchers mentioned that it was well tolerated, with mild adverse events seen that were similar to the placebo. Unfortunately, they do not mention what these adverse effects were.
Study 2
Another 24-week, randomized, double-blind, placebo-controlled, multi-regional study was conducted to evaluate the efficacy and safety of pyrilutamide in 120 men with androgenic alopecia.[5]Cision PR Newswire, (2023), Kintor Pharma Announces Completion of Subject Enrollment in Phase III Clinical Trial of KX-826 for Treatment of Male Androgenetic Alopecia in China. Available at: … Continue reading For this study, the researchers presented a poster at the 6th National Hair Academic Conference in China and it has since been translated to English online.
The participants were randomized into four groups:
- 0.25% pyrilutamide applied twice daily
- 0.5% pyrilutamide applied once daily
- 0.5% pyrilutamide twice daily
- Placebo (most likely treatment with just the cream or emollient that pyrilutamide is suspended in).
The researchers found that the participants that used 0.5% pyrilutamide twice daily showed improvement in total hair count at the end of the 24 weeks, with an increase of 15.34 hairs per cm2 compared to the placebo-treated groups (Figure 2).[6]Kintor Pharmaceutical Limited, (2022). Interim Results Announcement for the six months ended 30 June 2022. Kintor Pharmaceutical. 1-50. Available at: … Continue reading
It’s worth noting that the study reports that all the treatment groups demonstrated significant improvement compared to the placebo groups, but it does not provide details on statistical testing or variability in each group.
Figure 2: Mean change from the baseline in the number of non-vellus hairs in the target area (TAHC) after 24 weeks of treatment. * = p<0.05 compared to the baseline. QD = once daily, BID = twice daily. Adapted from:[7]Follicle Thought, (2022). Kintor Pharmaceutical KX-826 Phase 2 Results with Poster. Follicle Thought Hair Growth Treatment News. Available at: … Continue reading
According to the researchers, the safety profile was good in all dose groups with:
- 5.9% of participants reported pruritus (itchy skin)
- 2.5% of participants reported contact dermatitis
- 2 patients showing hypertriglyceridemia (high volume of fats in the blood)
Study 3
A randomized, double-blind, placebo-controlled, dose-escalation phase 1 trial was completed in the US over 24 weeks to evaluate the safety, tolerability, and pharmacokinetics of different concentrations of pyrilutamide.[8]Kintor Pharmaceuticals, (2020), Results of Kintor’s Phase 1b Clinical Trials of Pyrilutamide in America. News Center. Available at: https://en.kintor.com.cn/news/129.html (Accessed: 03 May 2023) The participants included 40 healthy male patients, 18-60 years old with androgenic alopecia, who were treated with multiple ascending dose applications of 0.3%, 1.2%, 4.8%, and 9.6% pyrilutamide.[9]Clinical Trials, (2019), Safety, tolerability, and pharmacokinetics of KX826 in healthy male subjects with androgenetic alopecia following topical single ascending dose administration. NIH. Available … Continue reading
The study showed no “severe” adverse drug events, with all adverse events relating to the drug application being mild contact dermatitis that healed in a short time.[10]Kintor Pharma, (no date), Developing Novel Drugs and Commercialization Platform. Available at: https://docs.publicnow.com/viewDoc?hash_primary=BFD6444A4669BD4BE0683A8BCC8B5E80F3D7E430 (Accessed: 03 … Continue reading Unfortunately, the amount of time taken to heal was not given.
Furthermore, the researchers measured the concentration of the drug in the blood to measure the risk of any systemic effects. While we do not have the specific numbers, the researchers do mention that the concentration of pyrilutamide in the blood was low, indicating that the topical concentrations used were not enough to cause a systemic accumulation (i.e., it may not lead to effects around the rest of the body after being topically applied, at these concentrations and frequency).
Study 4
A subsequent phase 2 study was next conducted in the US, with results announced in May 2023. The randomized, double-blind, placebo-controlled, and parallel-group clinical study was conducted in 123 male AGA patients who were classified as stage III vertex, IV, or V using the Hamilton-Norwood scale. 93 patients were randomly assigned to either 0.25% once daily (“QD”), 0.5% QD, and 0.5% twice daily (“BID”) pyrilutamide. 30 patients were randomly assigned to placebo groups for each dose.[11]Kintor Pharma, (2023). Voluntary Announcement. Successful Completion of Phase II Clinical Trial of KX-826 for Treatment of AGA in the United States. Available at: … Continue reading
According to Kintor, the 0.5% BID KX-826 group hair count increased by around 10 hairs per cm2 compared to the baseline after 24 weeks, which was statistically significant. An improvement was seen over the placebo. However, this was not found to be statistically significant. Similar to Study 3, a favorable safety profile was observed, with the only adverse events being mild and local scalp sensitivity.
Study 5
After a number of promising results, the next study showed a missed primary endpoint for a phase 3 study. This was a multicenter, randomized, double-blind, placebo-controlled study to evaluate the twice-daily use of 0.5% KX-826 in men with AGA in China.[12]Kintor Pharma, (2023). Results of KX-826 Phase III Clinical Trial for Treatment of Male AGA in China. Available at: … Continue reading Unfortunately, Kintor did not mention the number of participants in this study.
Pyrilutamide was found to be safe, with no serious adverse events reported. After 24 weeks, the total area hair count was statistically improved compared to the baseline (although no numbers were given), but once again, there was no significant change compared to the placebo.
A few months later, Kintor announced that the NMPA in China had approved a trial for the combination treatment of pyrilutamide and minoxidil in male AGA patients. We will have to wait and see whether combination treatment leads to better results.
UPDATE SEPTEMBER 2024:
Kintor Pivoted to Selling KX826 as a CosmeticDespite not achieving the primary endpoint in their most recently completed trial, Kintor announced in July of 2024 that cosmetic products containing KX-826 were to be launched for sale.[13]Kintor Pharma, (2024). Cosmetics with KX-826 as the core ingredient launched for sale. News Center. Available at: https://en.kintor.com.cn/news_details/3.html (Accessed: 09 September 2024)
Through Koshine, a subsidiary of Kintor, which was established in 2009, they have released the first of these cosmetics – Koshine 826 Anti Hair Loss Solution. It appears to have been listed on Amazon.com by Koshine Biomedica, although there has not yet been confirmation from Kintor or Koshine that this is the official product.[14]Amazon, (no date). KX-826 DHT Blocker Hair Thickening,3 Days Oil Control 1-2 Weeks Hair Loss Reduction 4-6 Weeks New Hair Visible, Hair Regrowth Spray for Men and Women -1 Month Supply 60ml. … Continue reading
Figure 3: KOSHINE 826, the cosmetic version of KX-826 currently being sold.
Koshine 826 is on sale for $69, which buys you a 60ml bottle for a ‘one-month supply’. 1 ml of solution is to be applied each morning and evening, constituting approximately 6-8 sprays from the bottle. The solution should be sprayed onto the exposed scalp within the region of hair loss, followed by a 3-minute scalp massage. Unfortunately, the concentration of KX-826 contained within the product is not stated, so it is not possible to predict how well this product may perform based on clinical studies. However, the product information claims that customers can expect oil control after 3 days of use, reduced hair loss after 1-2 weeks, and visible hair growth after 4-6 weeks.
So, how has Kintor gone from failing the primary endpoint for their most recent study to selling a product containing its KX-826? It all appears to be in the terminology.
To sell a drug in the USA – “articles intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease” – a company must demonstrate that the product is safe and effective, amongst other factors. This information is generally provided through several rounds of successful clinical trials. However, to sell a cosmetic – “articles intended to be rubbed, poured, sprinkled, or sprayed on, introduced into, or otherwise applied to the human body…for cleansing, beautifying, promoting attractiveness, or altering the appearance” – there is no requirement for FDA approval.[15]U.S. Food & Drug Administration, (2024). Cosmetics & U.S. Law. Available at: https://www.fda.gov/cosmetics/cosmetics-laws-regulations/cosmetics-us-law (Accessed: 09 September 2024)
In other words, cosmetics need not have proven efficacy because they are not used for ‘treating’ anything. Manufacturers don’t even need to prove the safety of a cosmetic before selling it, with action only taken if the FDA receives reliable information that suggests the product may be unsafe.[16]U.S. Food & Drug Administration, (2022). Cosmetic Products. Available at: https://www.fda.gov/cosmetics/cosmetic-products-ingredients/cosmetic-products (Accessed: 09 September 2024)
As Koshine 826 is being marketed as a cosmetic, it can be sold despite clinical trials not (yet) showing sufficient evidence to gain FDA approval. This situation will only change if the product is deemed to be unsafe or the FDA believes that Koshine 826 should also be defined as a drug, which would create the need for FDA approval. Only the FDA can truly define which products are cosmetics and which are drugs, and Kintor must be careful with their wording to ensure that Koshine 826 is not also being marketed as a drug. For now, though, Koshine 826 can be sold without the need for FDA approval.
UPDATE MARCH 2025
Kintor Announces Most Recent Phase 3 Trial Has Met its Primary Endpoint
Kintor Pharma has continued to conduct clinical trials even since launching the product as a cosmetic. The latest? A 16 center open-label trial in China including men and women with AGA.[17]Kintor Pharma. (2025). Long-Term Safety Phase III Clinical Trial Of KX-826 For The Treatment Of AGA Reached Primary Endpoint. Available at: https://en.kintor.com.cn/news_details/9.html (Accessed: … Continue reading
The primary endpoint was safety (incidence of treatment-emergent adverse events). Secondary endpoints included change in target non-vellus hair counts (TAHC), change in target non-vellus hair width (TAHW) and hair growth assessment (HGA) score.
Participants used 0.5% KX-826 twice daily for 52 weeks.
According to the press release, KX-826 showed good safety and tolerability in a clinical trial, with a low incidence of adverse effects, and no drug-related sexual dysfunction adverse events.
TAHC – At 52 weeks, 46% of patients showed ≥10 hairs/cm2 change from the baseline and 20% showed ≥20 hairs/cm2 change from the baseline.
TAHW – Showed a statistically significant increase from the baseline.
HGA – 53% of male participants and 48.4% of female participants showed an HGA score of ≥1.
Press Releases vs. Peer Reviewed Data, Can We Trust Kintor’s Results?
Kintor has conducted multiple studies to explore the efficacy and safety of KX-826, presenting promising results in press releases. However, none of these findings have been published in peer-reviewed journals, which limits the ability to independently verify the data. Peer-reviewed publications are essential for ensuring transparency, as they subject research to rigorous scrutiny by independent experts. Without this process, the information provided by Kintor reflects only what the company has chosen to disclose, raising concerns about potential biases or omitted data.
In contrast, certain natural supplements have published data, albeit often of limited quality. Even when evidence for supplements is weak, peer-reviewed studies provide a more complete picture by detailing methodologies, statistical analyses, and limitations. This transparency allows readers to critically assess claims and understand their clinical significance. For example, if a supplement claims to improve health outcomes, published studies might reveal whether these improvements are substantial or merely marginal.
Non-peer-reviewed data, such as press releases from pharmaceutical companies like Kintor, should be interpreted with caution for several reasons:
-
Lack of Independent Verification: Peer review ensures that findings are evaluated by unbiased experts who can identify flaws or inconsistencies. Without this step, data may be selectively presented to emphasize positive outcomes while downplaying adverse effects or inconclusive results.
-
Conflict of Interest Risks: Companies have a vested interest in promoting their products and may prioritize marketing over scientific integrity. This can lead to exaggerated claims or omission of unfavorable data.
-
Limited Methodological Transparency: Press releases often lack detailed information about study design, statistical analyses, and participant demographics, making it difficult to assess the robustness of the findings.
While natural supplements are not without issues—such as inconsistent ingredient quality or weak regulatory oversight—they often benefit from published studies that allow for critical evaluation. Until Kintor publishes its findings in reputable journals, it remains challenging to fully trust the reported efficacy and safety of KX-826. Independent peer-reviewed research is important for determining whether the claims made in press releases translate into meaningful clinical benefits.
What’s In the Future For KX-826?
Based on the July press release, Koshine 826 may be the first of many products to use KX-826. Kintor stated that they will continue exploring the use of KX-826 for androgenic alopecia and acne.
In their most recent press release, posted in August 2024, Kintor provided further details regarding the upcoming phase II/III clinical trial of KX-826 in the treatment of androgenic alopecia. Dermatology teams from more than 20 domestic hospitals are set to be involved, with over 750 participants expected to be enrolled. Enrollment will commence in early 2025. The trial itself will treat participants with 1% KX-826, which Kintor claims to have performed significantly better in preclinical studies than 0.5% KX-826. This would be the largest KX-826 trial to date, and if the 1% solution does significantly outperform the 0.5% solution, the results could be one to keep an eye on.[18]Kintor Pharma. (2024). Starting Again! Pioneer Pharmaceuticals KX-826 Tincture Registrational Clinical Trial Investigators Meeting Successfully Held. Kintor Pharma. Available at: … Continue reading
What are the Side Effects of Pyrilutamide?
As mentioned above, pyrilutamide treatment does not appear to lead to any serious side effects, with mild contact dermatitis being the only adverse event reported by the researchers. However, because we do not have the full study details or outcomes, we do not know if any other side effects were omitted.
If this is the only side effect, however, pyrilutamide may present an alternative to oral androgen receptor antagonists like flutamide (which you can read about here) that have limited safety profiles in both men and women. Furthermore, because pyrilutamide is a topical treatment instead of an oral treatment this may reduce the risk of systemic effects.
However, as yet, we have no information on whether pyrilutamide can build up in the body and potentially cause systemic effects. Pyrilutamide is an anti-androgen, and therefore it is not unreasonable to hypothesize that, if present at a high enough concentration, pyrilutamide will be associated with side effects like those of other anti-androgens (like erectile dysfunction and loss of sexual interest).
Is Pyrilutamide Right for Me?
You may want to experiment with pyrilutamide if:
- You accept the risk of potential side effects associated with the use of anti-androgen drugs
- You suffer from male or female pattern hair loss
- Are ok buying a product with no published (in peer-reviewed journals) data available for it
- Want to try a topical androgen receptor antagonist
Where Can I Get Pyrilutamide?
Although this product is still in its clinical trial phase, you can buy it online at certain retailers. However, if you do decide to try it, it will set you back around $100 – $110 for a 2 FL OZ bottle.
It is also the core ingredient within Koshine 826, a cosmetic product that has recently begun global sales. A one-month supply, 60ml, costs $69.
Final Thoughts
At a dose of 0.5% once daily in women and twice daily in men, topical pyrilutamide appears to be well-tolerated and may lead to an increase in hair number compared to the baseline. However, few of the studies that used a placebo found any statistically significant differences between the two groups. At this point in time, we would recommend not buying this product until more information from the currently ongoing trials is published.
References[+]
References ↑1 Pubchem, (no date). Pyrilutamide. NIH. Available at: https://pubchem.ncbi.nlm.nih.gov/substance/469676781 (Accessed: 04 May 2023) ↑2 Trueb, R.M., (2021). Understanding pattern hair loss-hair biology impacted by genes, androgens, prostaglandins, and epigenetic factors. Indian Journal of Plastic Surgery, 54(4). 385-392. Available at: https://doi.org/10.1055/s-0041-1739252 ↑3 Kintor, (2021), Kintor Pharmaceuticals Announced Successful Dosing of the First Batch of Patients for Acne Vulgaris Phase I/II Clinical Trial of Pyrilutamide. News Center. Available at: https://en.kintor.com.cn/news/172.html (Accessed: 03 May 2023) ↑4 Cision PR Newswire, (2022), Kintor Pharma Announced the Primary Endpoint of Phase II Clinical Study for KX-826’s Treatment of Female Androgenetic Alopecia in China was Met. Available at: https://www.prnewswire.com/news-releases/kintor-pharma-announced-the-primary-endpoint-of-phase-ii-clinical-study-for-kx-826s-treatment-of-female-androgenetic-alopecia-in-china-was-met-301691321.html (Accessed: 02 May 2023) ↑5 Cision PR Newswire, (2023), Kintor Pharma Announces Completion of Subject Enrollment in Phase III Clinical Trial of KX-826 for Treatment of Male Androgenetic Alopecia in China. Available at: https://www.prnewswire.com/news-releases/kintor-pharma-announces-completion-of-subject-enrollment-in-phase-iii-clinical-trial-of-kx-826-for-treatment-of-male-androgenetic-alopecia-in-china-301783455.html (Accessed: 03 May 2023) ↑6 Kintor Pharmaceutical Limited, (2022). Interim Results Announcement for the six months ended 30 June 2022. Kintor Pharmaceutical. 1-50. Available at: https://www1.hkexnews.hk/listedco/listconews/sehk/2022/0829/2022082902004.pdf (Accessed: 03 May 2023) ↑7 Follicle Thought, (2022). Kintor Pharmaceutical KX-826 Phase 2 Results with Poster. Follicle Thought Hair Growth Treatment News. Available at: https://folliclethought.com/kintor-pharmaceutical-kx-826-phase-2-results-with-poster/ (Accessed: 04 May 2023) ↑8 Kintor Pharmaceuticals, (2020), Results of Kintor’s Phase 1b Clinical Trials of Pyrilutamide in America. News Center. Available at: https://en.kintor.com.cn/news/129.html (Accessed: 03 May 2023) ↑9 Clinical Trials, (2019), Safety, tolerability, and pharmacokinetics of KX826 in healthy male subjects with androgenetic alopecia following topical single ascending dose administration. NIH. Available at: https://clinicaltrials.gov/ct2/show/NCT04984707 (Accessed: 03 May 2023) ↑10 Kintor Pharma, (no date), Developing Novel Drugs and Commercialization Platform. Available at: https://docs.publicnow.com/viewDoc?hash_primary=BFD6444A4669BD4BE0683A8BCC8B5E80F3D7E430 (Accessed: 03 May 2023) ↑11 Kintor Pharma, (2023). Voluntary Announcement. Successful Completion of Phase II Clinical Trial of KX-826 for Treatment of AGA in the United States. Available at: https://staticpacific.blob.core.windows.net/press-releases-attachments/1520008/HKEX-EPS_20230511_10734339_0.PDF (Accessed: 09 May 2024) ↑12 Kintor Pharma, (2023). Results of KX-826 Phase III Clinical Trial for Treatment of Male AGA in China. Available at: https://staticpacific.blob.core.windows.net/press-releases-attachments/1591631/HKEX-EPS_20231127_10979479_0.PDF (Accessed: 09 May 2024) ↑13 Kintor Pharma, (2024). Cosmetics with KX-826 as the core ingredient launched for sale. News Center. Available at: https://en.kintor.com.cn/news_details/3.html (Accessed: 09 September 2024) ↑14 Amazon, (no date). KX-826 DHT Blocker Hair Thickening,3 Days Oil Control 1-2 Weeks Hair Loss Reduction 4-6 Weeks New Hair Visible, Hair Regrowth Spray for Men and Women -1 Month Supply 60ml. Available at: https://www.amazon.com/Blocker-Thickening-Control-Reduction-Regrowth/dp/B0D97LT6MY (Accessed: 09 September 2024) ↑15 U.S. Food & Drug Administration, (2024). Cosmetics & U.S. Law. Available at: https://www.fda.gov/cosmetics/cosmetics-laws-regulations/cosmetics-us-law (Accessed: 09 September 2024) ↑16 U.S. Food & Drug Administration, (2022). Cosmetic Products. Available at: https://www.fda.gov/cosmetics/cosmetic-products-ingredients/cosmetic-products (Accessed: 09 September 2024) ↑17 Kintor Pharma. (2025). Long-Term Safety Phase III Clinical Trial Of KX-826 For The Treatment Of AGA Reached Primary Endpoint. Available at: https://en.kintor.com.cn/news_details/9.html (Accessed: March 2025) ↑18 Kintor Pharma. (2024). Starting Again! Pioneer Pharmaceuticals KX-826 Tincture Registrational Clinical Trial Investigators Meeting Successfully Held. Kintor Pharma. Available at: https://en.kintor.com.cn/news_details/4.html (Accessed: September 2024) In a recent milestone, a drug called ritlecitinib (brand name Litfulo™) has been approved for treating alopecia areata (AA) in adolescents and adults. Ritlecitinib is a type of drug classified as a kinase inhibitor.[1]Pfizer, (2023), FDA Approves Pfizer’s LITFULO™ (Ritlecitinib) for Adults and Adolescents with Severe Alopecia Areata. Pfizer. Available at: … Continue reading In this article, we are going to explore how ritlecitinib works, its safety and efficacy, and its implications for treating hair loss.
Key Takeaways
- Drug. The small molecule ritlecitinib is an inhibitor of Janus-associated kinase 3 (JAK3) recently approved for treating alopecia areata (AA).
- Clinical Data. Clinical trials have demonstrated that ritlecitinib can effectively promote hair regrowth in patients with AA.
- In a phase 2a study conducted on 142 patients (98 women and 44 men), ritlecitinib treatments resulted in improved hair growth in a substantial number of patients – 25% of patients showed 90% or more regrowth by the end of the study and 50% of patients showing 30% or more regrowth by the end of this study.[2]King, B., Guttman-Yassky, E., Peeva, E., Banerjee, A., Sinclair, R., Pavel, A.B., Zhu, L., Cox, L.A., Craiglow, B., Chen, L., Banfield, C., Page, K., Zhang, W., Vincent, M.S. (2021). A phase 2a … Continue reading
- A phase 2b/3 study conducted on 718 patients (446 women and 272 men), further supported the efficacy of ritlecitinib, with patients who received the 30 mg or 50 mg doses responding to a greater extent than controls.[3]King, B., Zhang, X., Harcha, W.G., Szepietowski, J.C., Shapiro, J., Lynde, C., Mesinkovska, N.A., Zwillich, S.H., Napatalung, L., Wasjsbrot, D., Fayyad, R., Freyman, A., Mitra, D., Purohit, V., … Continue reading
- In a sub-study conducted within these clinical trials, ritlecitinib also reduced the expression of several biomarkers associated with alopecia areata, which correlated with the improvement in disease severity as assessed by SALT scores.[4]Guttman-Yasky, E., Pavel, A.B., Diaz, A., Zhang, N., Duca, E.D., Estrada, Y., King, B., Banarjee, A., Banfield, C., Cox, L.A., Dowty, M.E., Page, K., Vincent, M.S., Zhang, W., Zhu, L., Peeva, E. … Continue reading
- Safety. Ritlecitinib is FDA-approved for prescription use, so it should be safe if your doctor recommends it. However, some mild side effects are associated with its use, including upper respiratory tract infections, nasopharyngitis, and headaches. Serious side effects were rare in the clinical trials described above. However, there were instances of breast cancer and shingles during the clinical trials (2 out of 718 patients each).
- Evidence Quality: Ritlecitinib scored 76/100 for evidence quality by our metrics.
- Best Practices. Ritlectinib is specifically indicated for severe alopecia areata and is not suitable for other types of hair loss. According to the patient information leaflet, ritlecitinib should be given at dosages of 50 mg once daily. [5]LITFULO, (2023). Highlights of prescribing information. LITFULO. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215830s000lbl.pdf (Accessed: 18 September 2023)
What is Ritlecitinib?
Ritlecitinib is a small-molecule inhibitor of the enzyme janus-associated kinase (JAK) that was approved in the US in June 2023. [6]Ramirez-Marin & Tosti (2022), Evaluating the Therapeutic Potential of Ritlecitinib for the Treatment of Alopecia Areata. Drug Design, Development and Therapy. 16. 363-374. Available at: … Continue reading Over a year ago, another JAK inhibitor, baricitinib, was approved last year for severe AA. Now, there’s a second FDA-approved drug for this hair loss disorder, and of a similar class for its mechanisms of action.
The recommended dose of ritlecitinib is 50 mg orally once a day with or without food.[7]{Pfizer, (no date), LITFULO Medical Information. Pfizer. Available at: https://www.pfizermedicalinformation.com/en-us/litfulo/boxed-warning (Accessed: 14 September 2023)
Figure 1: Chemical structure of ritlecitinib.[8]Selleckchem (no date), Ritlecitinib. Selleckchem. Available at: https://www.selleckchem.com/products/pf-06651600.html (Accessed: 15 September 2023)
How Does Ritlecitinib Work?
Ritlecitinib comes under a class of drugs called Janus kinase (JAK) inhibitors. This is because it selectively inhibits a specific enzyme in the JAK family called JAK3. JAK3 is part of a cell signaling pathway called the JAK/STAT pathway, which transmits signals from outside the cell to the nucleus to regulate the expression of genes. This pathway is involved in the control of processes such as the maintenance of stem cells, the formation of new blood cells, and the inflammatory response.[9]Thomas, S.J., Snowden, J.A., Zeidler, M.P., and Danson, S.J. (2015), The role of JAK/STAT signaling in the pathogenesis, prognosis and treatment of solid tumors. British Journal of Cancer. 113. … Continue reading
The JAK/STAT pathway is activated by a range of growth factors and other signaling molecules, including a group of substances called cytokines. Cytokines are proteins that can modulate the immune system in different ways, depending onthe context.[10]Broussard, G., Damania, B. (2020), KSHV: Immune Modulation and Immunotherapy. Frontiers in Immunology. 10. 1-8. Available at: https://doi.org/10.3389/fimmu.2019.03084
In our article on baricitinib, we talk about the JAK/STAT pathway and how cytokine receptors can be described as transmembrane receptors – the receptors cross the cell membrane and have sections that can be found inside and outside the cell. The binding of the cytokine to the receptor on the outside of the cell causes a protein called JAK to bind to the inside portion of the receptor, leading it to undergo a process called trans-phosphorylation, in which a phosphate group is transferred from the receptor to the JAK protein(Figure 2).[11]Harrison, J.A. (2012), The JAK/STAT Pathway. Cold Spring Harbor Perspectives in Biology. 4(3). 1-3. Available at: https://doi.org/10.1101/cshperspect.a011205
Figure 2: Diagram showing the process of activation of STAT by JAK phosphorylation.[12]Luo, W., Li, Y.W., Jiang, L.J., Chen, Q., Wang, T., Ye, D.W. (2020). Targeting JAK-STAT signaling to Control Cytokine Release Syndrome in COVID-19. Trends in Pharmacological Sciences. 8. 531-543. … Continue reading
These JAK proteins, in turn, activate other pathways by phosphorylating proteins like the STATs (signal transducer and activator of protein transcription). When activated by JAK phosphorylation, STAT proteins undergo a change in shape, which allows them to move to the nucleus (called translocation), where they can then activate or deactivate specific genes involved in several cellular processes.[13]Awasthi, N., Liongue, C., Ward, A.C. (2021), STAT proteins: a kaleidoscope of canonical and non-canonical functions in immunity and cancer. Journal of Hematology & Oncology. 14(198). 1-17. … Continue reading
The response to JAK/STAT pathway activation can be different across different types of cells and tissue, depending on the specific type of proteins that make up the pathway and what other signaling pathways are operating in that cell. This provides a contextual element to JAK/STAT signaling.[14]Harrison, D.A., The JAK/STAT Pathway. Cold Spring Harbor Perspectives in Biology. 4(3). A011205. Available at: https://doi.org/10.1101/cshperspect.a011205
How does JAK/STAT signaling relate to AA?
The short answer: activation of the JAK/STAT pathway leads to hair loss caused by immune system activation.
How does AA develop? Let’s recap. Our hair follicles have something called ‘immune privilege’ – they are less subject to the immune response than most of the other areas of the body. This is thought to be in place to protect the stem-cell-containing area of the hair follicle, known as the bulge, which is required for new hair follicle growth in the hair cycle.[15]Azzawi, S., Penzi, L.R., Senna, M.M. (2018), Immune Privilege Collapse and Alopecia Development: Is Stress a Factor. Skin Appendage Disorders. 4(4).236-244. Available at: … Continue reading In AA, something triggers a breakdown of the immune privilege of the hair follicle. The exact cause of this breakdown is not fully understood, but it may involve genetic factors, environmental triggers, or a combination of both.
When the immune privilege is compromised, a group of immune cells called T cells begin to attack the hair follicle. As mentioned earlier, the JAK/STAT pathway plays a critical role in transmitting signals within cells. When the immune system attacks hair follicles, the JAK/STAT pathway is activated, sending signals instructing cells to participate in the attack. As a result, the cells around the hair follicles respond to these signals by causing inflammation and damaging the hair follicle. This disrupts the normal hair growth cycle and leads to hair loss in the affected areas (Figure 3).[16]Kumar, N., Kuang, L., Villa, R., Kumar, P., Mishra, J. (2021), Mucosal Epithelial Jak Kinases in Health and Diseases. Mediators of Inflammation. 1-17. https://doi.org/10.1155/2021/6618924
Figure 3: The collapse of immune privilege in the anagen hair follicle during AA.[17]Lensin, M., Jabbari, A. (2022), An Overview of JAK/STAT Pathways and JAK Inhibition in Alopecia Areata. Frontiers in Immunology. 13. 1-17. Available at: https://doi.org/10.3389/fimmu.2022.955035
Why target JAK3 specifically?
JAK3 is particularly important in the development and function of T cells.[18]Sohn, S.J., Forbush, K.A., Nguyen, N., Witthuhn, B., Nosaka, T., Ihie, J.N., Perimutter, R.M. (1998). Requirement for JAK3 in mature T cells: Its role in regulation of T cell homeostasis. The Journal … Continue reading By targeting JAK3, ritlecitinib may help inhibit T cell activity without affecting other immune cells as strongly. This targeted approach may help to reduce the autoimmune response while preserving some aspects of the immune system’s ability to fight infections.[19]Dai, Z., Sezin, T., Chang, Y., Lee, E.Y., Wang, E.H.C., Christiano, A.M. (2022), Induction of T cell exhaustion by JAK1/3 inhibition in the treatment of alopecia areata. Frontiers in Immunology. 13. … Continue reading
Furthermore, Targeting JAK3 may provide a more precise therapeutic approach for AA. Since JAK3 is primarily involved in immune responses mediated by certain subsets of T cells, it could potentially lead to fewer off-target effects on other immune system functions. Of course, this precision is desirable to avoid compromising the immune system’s ability to protect against infections. Inhibiting JAK1/2 may have broader effects on the immune system, potentially leading to more significant side effects. For example, JAK1/2 inhibitors might interfere with the body’s response to infections or impact other physiological processes.[20]Sardana, K., Bathula, S., Khurana, A. (2023), Which is the Ideal JAK Inhibitor for Alopecia Areata – Baricitinib, Tofacitinib, Ritlecitinib, or Ifidancitinib – Revisiting the … Continue reading By specifically targeting JAK3, the goal is to minimize unwanted side effects while still addressing the autoimmune component of the AA disease mechanism.
Is Ritlecitinib Effective at Treating Alopecia Areata?
Several clinical trials have either already been carried out using ritlecitinib or are ongoing. These trials have been conducted in adults, adolescents, and children, either with AA or cicatricial alopecia (which is similar to AA in terms of disease mechanism, although there are important differences). In total, we could find 2 completed clinical trials with a total number of patients included being 789. We will also cover one of the studies that were conducted at the same time as these trials with the same patients.
The first study was a phase 2a randomized, placebo-controlled study to evaluate the efficacy and safety of ritlecitinib and a similar drug, brepocitinib, in AA.[21]King, B., Guttman-Yassky, E., Peeva, E., Banerjee, A., Sinclair, R., Pavel, A.B., Zhu, L., Cox, L.A., Craiglow, B., Chen, L., Banfield, C., Page, K., Zhang, W., Vincent, M.S. (2021). A phase 2a … Continue reading 142 participants took part (98 female and 44 male) with an average age of 36. Participants were treated with 200 mg of ritlecitinib or 60 mg of baricitinib once daily for four weeks. Then, they were treated with a maintenance dose of 50 mg (ritlecitinib) or 30 mg (baricitinib) for the next 20 weeks. The results were promising for patients with AA who started the study with over 50% of scalp hair loss. Both medications resulted in significant hair regrowth, with 25% (ritlecitinib group) and 34% (baricitinib group) of patients achieving near-complete hair regrowth as measured by Severity of Alopecia Tool (SALT90) scores compared to the placebo group (Figure 4).
The SALT tool is validated for measuring the extent of hair loss in AA with 0% meaning no hair loss, and 100% meaning complete hair loss (with several grades in between).[22]Wyrwich, K.W., Kitchen, H., Knight, S., Aldhouse, N.V.J., Macey, J., Nunes, F.P., Dutronc, Y., Mesinkovska, N., Ko, J.M., King, B.A. (2020). The Alopecia Areata Investigator Global Assessment Scale: … Continue reading The SALT90 score, however, measures the percentage of people who achieved at least 90% of hair regrowth.
Figure 4: Effect of Brepocitinib, Ritlectinib, or a placebo on SALT scores in patients with alopecia areata over 24 weeks. SALT30 = % of patients who showed a SALT score over 30%. SALT90 = % of patients who showed a SALT score over 90%.[23]King, B., Guttman-Yassky, E., Peeva, E., Banerjee, A., Sinclair, R., Pavel, A.B., Zhu, L., Cox, L.A., Craiglow, B., Chen, L., Banfield, C., Page, K., Zhang, W., Vincent, M.S. (2021). A phase 2a … Continue reading
Adverse events were reported in all three treatment groups, with common events including upper respiratory tract infection, nasopharyngitis, headache, acne, and nausea. Serious adverse events were only noted in the brepocitinib group, which could indicate that it may induce more hair regrowth than ritlecitinib but may not be as safe to use.
So, to summarize, although brepocitinib performed better, ritlecitinib also improved hair regrowth scores in patients with AA and appeared to be better tolerated than brepocitinib.
This particular clinical trial also contained a further sub-study to further evaluate the efficacy and safety of ritlecitinib and brepocitinib.[24]Guttman-Yasky, E., Pavel, A.B., Diaz, A., Zhang, N., Duca, E.D., Estrada, Y., King, B., Banarjee, A., Banfield, C., Cox, L.A., Dowty, M.E., Page, K., Vincent, M.S., Zhang, W., Zhu, L., Peeva, E. … Continue reading The study involved taking scalp biopsy samples from patients with AA at baseline and analyzing changes in specific biomarkers between baseline and weeks 12 and 24 of treatment.
Ritlecitinib significantly shifted gene expression in the scalp towards an improved, non-lesional profile. This improvement exceeded 100% of baseline at week 24, indicating a strong positive response to the treatment. Furthermore, the treatment led to a downregulation of inflammatory markers associated with T cells, T cell activation, and other immune response markers. These changes also correlated with an improvement in the SALT score (Figure 5).
Figure 5: Overall percentage improvement in the lesional scalp for each treatment group at weeks 12 and 24. P=<0.001 at weeks 12 and 24 comparisons with placebo and comparisons between treatment groups.[25]Guttman-Yasky, E., Pavel, A.B., Diaz, A., Zhang, N., Duca, E.D., Estrada, Y., King, B., Banarjee, A., Banfield, C., Cox, L.A., Dowty, M.E., Page, K., Vincent, M.S., Zhang, W., Zhu, L., Peeva, E. … Continue reading
However, the most recent study (just prior to ritlecitinib becoming FDA approved) was a 48-week phase 2b/3 randomized, double-blind, placebo-controlled clinical trial.[26]King, B., Zhang, X., Harcha, W.G>, Szepietowski, J.C., Shapiro, J., Lynde, C., Mesinkovska, N.A., Zwillich, S.H., Napatalung, L., Wajsbrot, D., Fayyad, R., Freyman, A., Mitra, D., Purohit, V., … Continue reading The trial was conducted across118 sites in 18 countries, with 718 patients (446 women, 272 men) aged 12 years and older with alopecia areata and at least 50% scalp hair loss – as measured by SALT severity scores.
The patients were assigned to either an oral ritlecitinib or placebo treatment, given once daily for 24 weeks. Several doses of ritlecitinib were tested, along with a variable 4-week loading dose and were followed by a 24-week extension period, during which the ritlecitinib group continued their treatment, and the placebo-treated group switched to ritlecitinib (Figure 6).
Figure 6: The clinical trial study design.[27]King, B., Zhang, X., Harcha, W.G., Szepietowski, J.C., Shapiro, J., Lynde, C., Mesinkovska, N.A., Zwillich, S.H., Napatalung, L., Wasjsbrot, D., Fayyad, R., Freyman, A., Mitra, D., Purohit, V., … Continue reading
The researchers found that patients on the 30 mg or 50 mg doses of ritlecitinib exhibited the highest regrowth scores, and including a loading dose resulted in further improvement. Response rates based on a SALT score of 20% or less at week 24 were significantly higher in ritlecitinib groups compared to the placebo (Figure 7A):
- 29.1% difference for 200 mg + 50 mg
- 20.8% difference for 200 mg + 30 mg
- 21.9% difference for 50 mg
- 12.8% difference for 30 mg
The response rates, based on a SALT score of 10 or less at week 24, were also significantly higher in ritlecitinib groups compared to the placebo (Figure 7B). Furthermore, the proportion of patients with a Patient Global Impression of Change (PGI-C) response of moderately or greatly improved was greater with ritlecitinib treatment compared to placebo at week 24 (Figure 7C). The PGI-C reflects a patient’s belief about the efficacy of a treatment.[28]Ferguson, L., Scheman, J. (2009). Patient global impression of change scores within the chronic pain rehabilitation program. The Journal of Pain. 10(4). S73. Available at: … Continue reading Regrowth of eyelashes and eyebrows was also observed with ritlecitinib treatment (Figures 7D/7E), with responses continuing up to week 48 in all ritlecitinib groups.
Figure 7: Efficacy of ritlecitinib treatment with or without loading doses and compared to placebo groups. (A): Response based on a SALT score of 20 or less. (B) Response based on a SALT score of 10 or less. (C): PGI-C response. (D): Eyebrow response. (E): Eyelash response. (F): Representative photo of a patient at baseline and week 24 with significant growth observed.[29]King, B., Zhang, X., Harcha, W.G., Szepietowski, J.C., Shapiro, J., Lynde, C., Mesinkovska, N.A., Zwillich, S.H., Napatalung, L., Wasjsbrot, D., Fayyad, R., Freyman, A., Mitra, D., Purohit, V., … Continue reading
So, to summarize, ritlecitinib was effective in promoting hair regrowth and was generally well tolerated (more on that below) in patients with alopecia areata. There is a longer-term efficacy study currently ongoing called ALLEGRO-LT, which aims to evaluate the safety and efficacy of ritlecitinib over a period of 60 months (5 years).[30]Clinical Trials (2023) Long-term PF-06651600 for the Treatment of Alopecia Areata (ALLEGRO-LT). NIH. Available at: … Continue reading This trial is due to finish in 2026 and will hopefully provide the long-term efficacy and safety data that is needed.
Is Ritlecitinib Safe?
The overall safety profile was observed throughout the study, and it was determined that ritlecitinib was generally well-tolerated across all doses and showed a favorable safety profile. The most common adverse effects (occurring in at least 10% of patients in any treatment group) included:
- Upper respiratory tract infection – 8.01% of all patients who took ritlecitinib.
- Nasopharyngitis – 13.01% of all patients who took ritlecitinib.
- Headache – 10.96% of all patients who took ritlecitinib
A total of 16 more serious adverse events were reported in 14 patients. These included:
- Infections (Five serious infections were reported. Notably, one patient experienced empyema (fluid between the lungs) and sepsis, while two cases of shingles occurred.
- Malignancies: Two cases of breast cancer were reported, one of which was deemed related to the treatment by an investigator.
- Other serious events were appendicitis, diverticulitis, and pulmonary embolism.
Treatment with ritlecitinib also led to changes in hematological parameters, including:
- Decrease in hemoglobin levels.
- Transient decrease in platelet count.
- Early decrease in absolute lymphocyte levels, particularly in groups with the 200 mg loading dose.
- Early decreases in natural killer cell counts, most apparent in groups with a 200 mg loading dose.
So 14/718 patients experienced a more serious adverse effect – so roughly 2% of patients, or 1 in 50. While you may consider these ‘good odds’, it is important to consider these potential adverse effects when making a treatment decision and always consult a physician.
Is Ritlecitinib for Me?
Ritlecitinib is an exciting new treatment; however, it is important to remember that it is for the treatment of severe alopecia areata only and will not work for other hair loss types like androgenetic alopecia, as the mechanisms of hair loss are very different. You may want to try this treatment if:
- You have severe alopecia areata.
- You have tried other treatments with no success.
- You have spoken to your physician, and they have suggested it based on your alopecia severity.
References[+]
References ↑1 Pfizer, (2023), FDA Approves Pfizer’s LITFULO™ (Ritlecitinib) for Adults and Adolescents with Severe Alopecia Areata. Pfizer. Available at: https://www.pfizer.com/news/press-release/press-release-detail/fda-approves-pfizers-litfulotm-ritlecitinib-adults-and (Accessed: 14 September 2023) ↑2, ↑23 King, B., Guttman-Yassky, E., Peeva, E., Banerjee, A., Sinclair, R., Pavel, A.B., Zhu, L., Cox, L.A., Craiglow, B., Chen, L., Banfield, C., Page, K., Zhang, W., Vincent, M.S. (2021). A phase 2a randomized, placebo-controlled study to evaluate the efficacy and safety of the oral janus kinase inhibitors ritlecitinib and brepocitinib in alopecia areata: 24-week results. Journal of the American Academy of Dermatology. 85(2). 379-387. Available at: https://doi.10.1016/j.jaad.2021.03.050 ↑3 King, B., Zhang, X., Harcha, W.G., Szepietowski, J.C., Shapiro, J., Lynde, C., Mesinkovska, N.A., Zwillich, S.H., Napatalung, L., Wasjsbrot, D., Fayyad, R., Freyman, A., Mitra, D., Purohit, V., Sinclair, R., Wolk, R. (2023). Efficacy and Safety of Ritlecitinib in adults and adolescents with alopecia areata: a randomized, double-blind, multicentre, phase 2b-3 trial. The Lancet. 401. 1518-1529. Available at: https://doi.org/10.1016/S0140-6736(23)00222-2 ↑4, ↑24, ↑25 Guttman-Yasky, E., Pavel, A.B., Diaz, A., Zhang, N., Duca, E.D., Estrada, Y., King, B., Banarjee, A., Banfield, C., Cox, L.A., Dowty, M.E., Page, K., Vincent, M.S., Zhang, W., Zhu, L., Peeva, E. (2022), Ritlecitinib and brepocitinib demonstrate significant improvement in scalp alopecia areata biomarkers. Atopic Dermatitis and Inflammatory Skin Disease. 149(4). P1318-1328. Available at: https://doi.org/10.1016/j.jaci.2021.10.036 ↑5 LITFULO, (2023). Highlights of prescribing information. LITFULO. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215830s000lbl.pdf (Accessed: 18 September 2023) ↑6 Ramirez-Marin & Tosti (2022), Evaluating the Therapeutic Potential of Ritlecitinib for the Treatment of Alopecia Areata. Drug Design, Development and Therapy. 16. 363-374. Available at: https://doi.org/10.2147/DDDT.S334727 ↑7 {Pfizer, (no date), LITFULO Medical Information. Pfizer. Available at: https://www.pfizermedicalinformation.com/en-us/litfulo/boxed-warning (Accessed: 14 September 2023) ↑8 Selleckchem (no date), Ritlecitinib. Selleckchem. Available at: https://www.selleckchem.com/products/pf-06651600.html (Accessed: 15 September 2023) ↑9 Thomas, S.J., Snowden, J.A., Zeidler, M.P., and Danson, S.J. (2015), The role of JAK/STAT signaling in the pathogenesis, prognosis and treatment of solid tumors. British Journal of Cancer. 113. 365-371. Available at: https://doi.org/10.1038/bjc.2015.233 ↑10 Broussard, G., Damania, B. (2020), KSHV: Immune Modulation and Immunotherapy. Frontiers in Immunology. 10. 1-8. Available at: https://doi.org/10.3389/fimmu.2019.03084 ↑11 Harrison, J.A. (2012), The JAK/STAT Pathway. Cold Spring Harbor Perspectives in Biology. 4(3). 1-3. Available at: https://doi.org/10.1101/cshperspect.a011205 ↑12 Luo, W., Li, Y.W., Jiang, L.J., Chen, Q., Wang, T., Ye, D.W. (2020). Targeting JAK-STAT signaling to Control Cytokine Release Syndrome in COVID-19. Trends in Pharmacological Sciences. 8. 531-543. Available at: https://doi.org/10.1016/kj.tips.2020.06.007 ↑13 Awasthi, N., Liongue, C., Ward, A.C. (2021), STAT proteins: a kaleidoscope of canonical and non-canonical functions in immunity and cancer. Journal of Hematology & Oncology. 14(198). 1-17. https://doi.org/10.1186/s13045-021-01214-y ↑14 Harrison, D.A., The JAK/STAT Pathway. Cold Spring Harbor Perspectives in Biology. 4(3). A011205. Available at: https://doi.org/10.1101/cshperspect.a011205 ↑15 Azzawi, S., Penzi, L.R., Senna, M.M. (2018), Immune Privilege Collapse and Alopecia Development: Is Stress a Factor. Skin Appendage Disorders. 4(4).236-244. Available at: https://doi.org/10.1159/0000485080 ↑16 Kumar, N., Kuang, L., Villa, R., Kumar, P., Mishra, J. (2021), Mucosal Epithelial Jak Kinases in Health and Diseases. Mediators of Inflammation. 1-17. https://doi.org/10.1155/2021/6618924 ↑17 Lensin, M., Jabbari, A. (2022), An Overview of JAK/STAT Pathways and JAK Inhibition in Alopecia Areata. Frontiers in Immunology. 13. 1-17. Available at: https://doi.org/10.3389/fimmu.2022.955035 ↑18 Sohn, S.J., Forbush, K.A., Nguyen, N., Witthuhn, B., Nosaka, T., Ihie, J.N., Perimutter, R.M. (1998). Requirement for JAK3 in mature T cells: Its role in regulation of T cell homeostasis. The Journal of Immunology. 160(5). 2130-2138. Available at: https://doi.org/10.4049/jimmunol.160.5.2130 ↑19 Dai, Z., Sezin, T., Chang, Y., Lee, E.Y., Wang, E.H.C., Christiano, A.M. (2022), Induction of T cell exhaustion by JAK1/3 inhibition in the treatment of alopecia areata. Frontiers in Immunology. 13. 1-14. Available at: https://doi.org/10.3389/fimmu.2022.955038 ↑20 Sardana, K., Bathula, S., Khurana, A. (2023), Which is the Ideal JAK Inhibitor for Alopecia Areata – Baricitinib, Tofacitinib, Ritlecitinib, or Ifidancitinib – Revisiting the Immunomechanisms of the JAK Pathway. Indian Dermatology Online Journal. 14. 465-474. Available at: https://doi.org/10.4103/idoj.idoj_452_22 ↑21 King, B., Guttman-Yassky, E., Peeva, E., Banerjee, A., Sinclair, R., Pavel, A.B., Zhu, L., Cox, L.A., Craiglow, B., Chen, L., Banfield, C., Page, K., Zhang, W., Vincent, M.S. (2021). A phase 2a randomized, placebo-controlled study to evaluate the efficacy and safety of the oral janus kinase inhibitors ritlecitinib and brepocitinib in alopecia areata: 24-week results. Journal of the American Academy of Dermatology. 85(2). 379-387. Available at: https://doi.org/10.1016/j.jaad.2021.03.050 ↑22 Wyrwich, K.W., Kitchen, H., Knight, S., Aldhouse, N.V.J., Macey, J., Nunes, F.P., Dutronc, Y., Mesinkovska, N., Ko, J.M., King, B.A. (2020). The Alopecia Areata Investigator Global Assessment Scale: A Measure for Evaluating Clinically Meaningful Success in Clinical Trials. 183(4). 702-709. Available at: https://doi.org/10.1111/bjd.18883 ↑26 King, B., Zhang, X., Harcha, W.G>, Szepietowski, J.C., Shapiro, J., Lynde, C., Mesinkovska, N.A., Zwillich, S.H., Napatalung, L., Wajsbrot, D., Fayyad, R., Freyman, A., Mitra, D., Purohit, V., Sinclair, R., Wolk, R. (2023). Efficacy and safety of ritlecitinib in adults and adolescents with alopecia areata: a randomized, double-blind, multicentre, phase 2b-3 trial. The Lancet. 401(10387). 1518-1529. Available at: https://doi.org/10.1016/S0140-6736(23)002222-2 ↑27, ↑29 King, B., Zhang, X., Harcha, W.G., Szepietowski, J.C., Shapiro, J., Lynde, C., Mesinkovska, N.A., Zwillich, S.H., Napatalung, L., Wasjsbrot, D., Fayyad, R., Freyman, A., Mitra, D., Purohit, V., Sinclair, R., Wolk, R. (2023). Efficacy and Safety of Ritlecitinib in Adults and Adolescents with Alopecia Areata: a Randomized, Double-Blind, Multicentre, Phase 2b-3 Trial. The Lancet. 401. 1518-1529. Available at: https://doi.org/10.1016/S0140-6736(23)00222-2 ↑28 Ferguson, L., Scheman, J. (2009). Patient global impression of change scores within the chronic pain rehabilitation program. The Journal of Pain. 10(4). S73. Available at: https://doi.org/10.1016/j.pain.2009.01.258 ↑30 Clinical Trials (2023) Long-term PF-06651600 for the Treatment of Alopecia Areata (ALLEGRO-LT). NIH. Available at: https://clinicaltrials.gov/study/NCT04006457?term=ALLEGRO-LT&checkSpell=false&rank=1 (Accessed: 18 September 2023) Ketoconazole is a versatile antifungal drug with widespread applications. It is commonly employed to address dandruff issues. It is also utilized off-label as a remedy for hair loss in both men and women, specifically targeting conditions like androgenic alopecia and telogen effluvium that result from an overgrowth of microorganisms on the scalp.
In this guide, we’ll delve into why you might be shedding after using ketoconazole, the difference between normal and abnormal shedding, solutions, and recommendations for those experiencing hair shedding.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

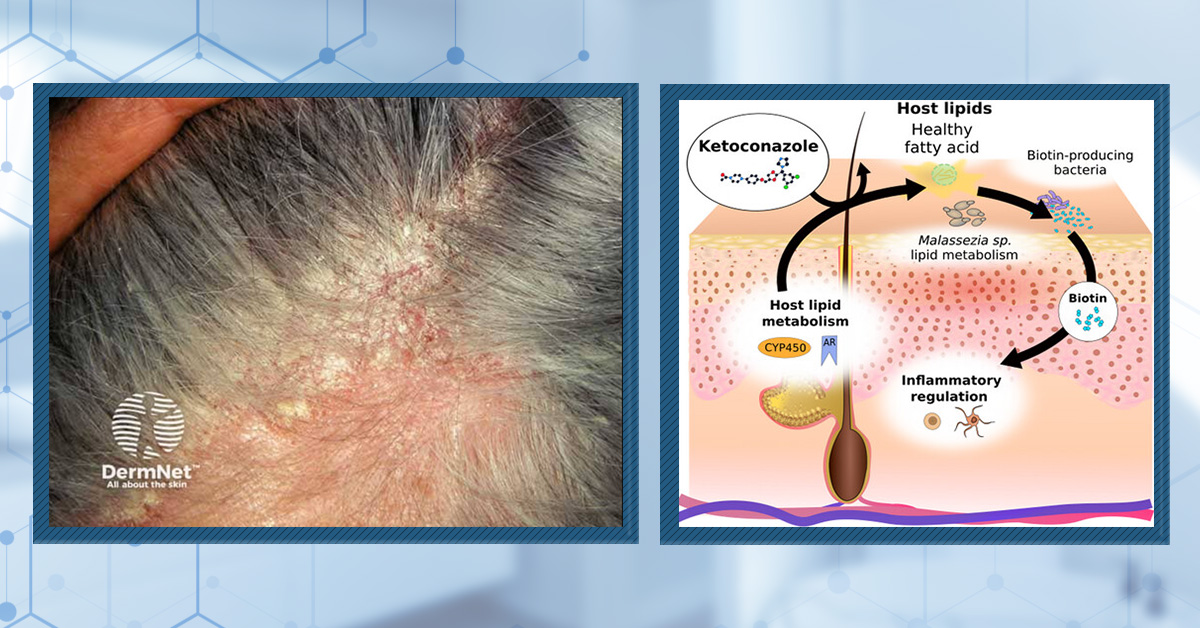
What is Ketoconazole?
Ketoconazole is an antifungal medication that is typically used to treat a variety of fungal infections in the body; however, it is also used in the treatment of hair loss conditions like androgenic alopecia (AGA) and telogen effluvium (TE) in the form of topicals and shampoos. Some ketoconazole-based products formulated for hair loss are available over-the-counter (OTC), such as 1% ketoconazole shampoos. In some instances, healthcare professionals may recommend or prescribe stronger ketoconazole treatments.
How Does Ketoconazole Work?
Ketoconazole works as an antifungal agent by disrupting the cell membranes of fungi, inhibiting their growth and replication. The antifungal properties of ketoconazole can help to alleviate these scalp conditions by reducing fungal activity and inflammation. The potential benefit for hair loss conditions such as AGA and TE is that a healthier, less inflamed scalp can create a more favorable environment for hair growth.
Further research suggests that ketoconazole shampoo can reduce dihydrotestosterone (DHT) levels by inhibiting 5 alpha-reductase. Combined usage with finasteride may lead to a more complete treatment.[1]Perez, B.S.H. (2004). Ketoconazole as an adjunct to finasteride in the treatment of androgenetic alopecia in men. Medical Hypotheses. 62(1). 112-115. Available at: … Continue reading
What are the Possible Causes of Hair Shedding After Ketoconazole Use?
Hair shedding after ketoconazole treatment can be disconcerting, but it’s important to understand the potential reasons behind this phenomenon.
Initial Ketoconazole Use
If you have been using ketoconazole for 1-3 months and are experiencing shedding, it may be because the scalp is still adjusting (and responding) to new treatments. Therefore, it’s possible that some of your shedding is due to a positive treatment response.
Ketoconazole Side Effect
According to Nizoral, in rare cases, ketoconazole may cause “inflamed hair follicles, hair loss, or changes in hair texture”.[2]Nizoral, (no date). Nizoral Anti-Dandruff Shampoo Ketoconazole. Nizoral. Available at: https://www.medicines.org.uk/emc/files/pil.6456.pdf (Accessed: 25 October 2023) You can find out if the hair shedding experienced is due to ketoconazole if you are also experiencing scalp dryness, hair dryness, and itchiness. Furthermore, if scalp redness is also experienced, you may be experiencing an allergic reaction to the product.
Seasonal Shedding
Toward the middle and end of the summer, humans undergo a temporary uptick in shedding due to hair cycle seasonality. While this shedding is primarily unavoidable, it also shouldn’t interfere with the success of any long-term hair loss treatments. So, your current bout of shedding might relate more to seasonality than anything else.
Other Hair Loss Products
Sometimes, the shedding might not be from ketoconazole but rather from other recently added treatments. Treatments like minoxidil shorten the non-growing (telogen) phase, which induces the shedding of club telogen hairs, leading to an increase in hair shedding.[3]Shadi, Z. (2023). Compliance to Topical Minoxidil and Reasons for Discontinuation among Patients with Androgenetic Alopecia. Dermatology and Therapy (Heidelb). 13(5). 1157-1169. Available at: … Continue reading
Ketoconazole Overuse
Overusing ketoconazole can lead to irritation, scalp dryness, and hair loss. Therefore, when using a product such as this, you should use it only as often as recommended by the brand or your doctor.
The Difference between Normal Hair Shedding and Abnormal Hair Loss
Normal hair shedding and abnormal hair loss are distinct processes that can affect the health and appearance of your hair. Understanding their differences is crucial for maintaining good hair care and addressing potential issues.
Normal Shedding
We all shed scalp hair; it’s a normal part of the hair follicle cycle, with the average number of hairs shed daily ranging from 50-100 hairs.[4]American Academy of Dermatology, (no date). Do you have hair loss or hair shedding? American Academy of Dermatology. Available at: … Continue reading These hairs typically fall out with no discomfort or noticeable changes in hair density and do not result in visible thinning or bald spots.
Abnormal Shedding
In contrast, abnormal hair loss, alopecia, involves excessive or sudden hair loss beyond normal shedding. It can be caused by various factors, such as genetics, medical conditions, stress, hormonal changes, medication, or an improper diet.[5]Alessandrini, A., Bruni, F., Piraccini, B.M., Starace, M. (2021). Common causes of hair loss – clinical manifestations, trichoscopy, and therapy. JEADV. 35. 629-640. Available at: … Continue reading Abnormal hair loss often leads to noticeable thinning, receding hairlines, or bald patches. Recognizing and addressing the underlying cause of abnormal hair loss is essential for effective treatment and management.
Solutions and Recommendations for Those Experiencing Hair Shedding Due to Ketoconazole
If the ketoconazole shampoo is causing hair shedding with or without scalp irritation, you do not necessarily have to stop usage. The following solutions may help to reduce symptoms:
- Switch from 2% to 1% ketoconazole. This should reduce the “power” of ketoconazole and, thereby, its effect on the hair.
- Reduce ketoconazole’s usage frequency and/or scalp contact time. While ketoconazole shampoo is typically used 2-3 times weekly and left on the scalp for up to 15 minutes, these usage parameters can irritate many people’s scalps. The simplest way to troubleshoot this is to reduce your use. Opt for 1-2 times weekly ketoconazole shampooing and/or only leave in the shampoo for 2-5 minutes.
- Add in a conditioner. After shampooing with ketoconazole, add in a conditioner. This should help moisturize the scalp and hair, reducing any hair texture changes caused by scalp/hair dryness.
If you decide to make any of the above changes, it’s important to give it time to see if the shedding stops or reduces. Assessing the effects of any change in hair care products or routines typically takes several weeks.
If this does not resolve the hair shedding, consider stopping the shampoo and/or seeking help from our community.
References[+]
References ↑1 Perez, B.S.H. (2004). Ketoconazole as an adjunct to finasteride in the treatment of androgenetic alopecia in men. Medical Hypotheses. 62(1). 112-115. Available at: https://doi.org/10.1016/s0306-9877(03)00264-0 ↑2 Nizoral, (no date). Nizoral Anti-Dandruff Shampoo Ketoconazole. Nizoral. Available at: https://www.medicines.org.uk/emc/files/pil.6456.pdf (Accessed: 25 October 2023) ↑3 Shadi, Z. (2023). Compliance to Topical Minoxidil and Reasons for Discontinuation among Patients with Androgenetic Alopecia. Dermatology and Therapy (Heidelb). 13(5). 1157-1169. Available at: https://doi.org/10.1007/s13555-023-00919-x ↑4 American Academy of Dermatology, (no date). Do you have hair loss or hair shedding? American Academy of Dermatology. Available at: https://www.aad.org/public/diseases/hair-loss/insider/shedding#:~:text=It ‘s%20normal%20to%20shed%20between,this%20condition%20is%20telogen%20effluvium. (Accessed: 25 October 2023) ↑5 Alessandrini, A., Bruni, F., Piraccini, B.M., Starace, M. (2021). Common causes of hair loss – clinical manifestations, trichoscopy, and therapy. JEADV. 35. 629-640. Available at: https://doi.org/10.1111/jdv.17079 When selecting hair loss treatments, it’s critical to understand how fast your hair loss is progressing, and why the speed your hair loss should influence your treatment choices – particularly for those with rapidly-progressing androgenic alopecia.
In this article, we’ll uncover:
- The average speed of hair loss progression (per year)
- How to estimate your own speed of hair loss (at home)
- Why people with faster hair loss face bigger stakes for treatment failures
- How to minimize these failures by understanding evidence quality
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

If we have androgenic alopecia, how quickly will we lose hair?
Clinical studies suggest that men with androgenic alopecia will lose 5% hair volume per year. At this rate, it typically takes 15-25 years for a man to go fully bald.[1]Rushton DH, Ramsay ID, Norris MJ, Gilkes JJ. Natural progression of male pattern baldness in young men. Clin Exp Dermatol. 1991 May;16(3):188-92. doi: 10.1111/j.1365-2230.1991.tb00343.x. PMID: … Continue reading[2]Sinclair R. Male pattern androgenetic alopecia. BMJ. 1998 Sep 26;317(7162):865-9. doi: 10.1136/bmj.317.7162.865. PMID: 9748188; PMCID: PMC1113949.
However, it’s important to remember that 5% is just the average rate of hair loss.
In other words, 5% is just the mid-point on a bellcurve. Some people will lose hair at a much slower rate than 5% yearly; others will lose hair much faster.
Why should we care about how fast (or slow) we’re losing hair?
Because men & women with faster hair loss face a bigger opportunity cost for failed treatments. For these individuals, the cost of failure is much, much higher. Consider the following hypothetical:
Person A is losing hair slowly. They try a nutraceutical product, which is supported by low-quality evidence. It doesn’t work. After 12 months, they quit. They now have 1% less hair compared to a year ago. Their hair basically looks the same.
Person B is losing hair rapidly. They try the same nutraceutical product. It doesn’t work. After 12 months, they quit. They now have 25% less hair compared to a year ago. Their hair loss has significantly advanced.
Clinical studies overwhelmingly suggest it’s easier to stop hair loss than it is to regrow significant amounts of lost hair.[3]Sinclair R, Torkamani N, Jones L. Androgenetic alopecia: new insights into the pathogenesis and mechanism of hair loss. F1000Res. 2015 Aug 19;4(F1000 Faculty Rev):585. doi: … Continue reading
Therefore, when choosing treatments, time is of the essence. This is especially true for people with rapid-onset hair loss. So if we want to make fully-informed treatment choices, we should know how quickly our hair loss is advancing.
How can we estimate how fast we’re losing hair?
Ask yourself the following question:
In the last 6 months, have you experienced a visual loss in hair density? In other words, during this time, do you feel your hair loss has gotten cosmetically worse?
If no, you’re probably losing hair more slowly. If yes, you’re probably losing hair faster than 5% yearly.
After all, researchers have calibrated mens’ hair density changes with self-perception data, and they concluded: (3)
“…a deterioration in hair density > 15% was required before subjective awareness became evident.”Long-story short: if you’re weighing your treatment options, do a quick assessment of how fast you’re losing hair.
The slower your hair loss, the more wiggle room you have to experiment. Why? Because the cost of failure might only equate to a 5% loss in hair density.
The faster your hair loss, the more imperative it is to seek treatments with the highest levels of clinical support. Why? Because these treatments tend to maximize your chances of success, and your magnitude of hair regrowth.
We rank some of these treatment options in this video. Moreover, we dive into what constitutes a good study in this article. It’s a deep-dive into how hair loss companies cheat their clinical trials.
Evidence quality example: saw palmetto vs. finasteride
Compare two potential hair loss interventions: saw palmetto and finasteride. One is natural; the other is a drug. Both substances have clinical support for hair growth, particularly for androgenic alopecia. Both substances also work similarly: they help lower the hormone dihydrotestosterone (DHT) in balding regions.
Similar substances. Similar mechanisms. Both clinically supported. But are these truly equal interventions for hair growth? A deeper dive into the evidence on both interventions paints a more nuanced (and dramatically different) picture than what is suggested at face-value.
Saw Palmetto for Hair Loss: 2022 Meta-Analysis
Over nine studies totaling 381 people have shown that saw palmetto might help improve androgenic alopecia.[4]Evron E, Juhasz M, Babadjouni A, Mesinkovska NA. Natural Hair Supplement: Friend or Foe? Saw Palmetto, a Systematic Review in Alopecia. Skin Appendage Disord. 2020 Nov;6(6):329-337. doi: … Continue reading At face value, this sounds great. But looking closer, many of these studies are what we would call lower quality: most of them lacked a placebo group, some were funded by companies selling saw palmetto, and all had small sample sizes.
This means that, for each study, there’s a higher risk of false-positive results: results due to statistical noise that would’ve washed out with a larger sample size.
This phenomenon happens all the time: early studies on an intervention showing promise, followed by larger, more robust studies showing no effect for that same intervention.
In fact, this happened once before for this same supplement – saw palmetto – but for the indication of prostate enlargement.
In the 1990s, several small studies suggested that saw palmetto extract might help reduce symptoms of an enlarged prostate.[5]Descotes, J., Rambeaud, J., Deschaseaux, P. et al. Placebo-Controlled Evaluation of the Efficacy and Tolerability of Permixon® in Benign Prostatic Hyperplasia after Exclusion of Placebo … Continue reading These studies inspired better-controlled clinical trials with hundreds of participants over extended periods, in which saw palmetto showed little-to-no effect.[6]Suzuki M, Ito Y, Fujino T, Abe M, Umegaki K, Onoue S, Noguchi H, Yamada S. Pharmacological effects of saw palmetto extract in the lower urinary tract. Acta Pharmacol Sin. 2009 Mar;30(3):227-81. doi: … Continue reading
Again, study quality, results replication, and sample sizes all inform evidence quality. The lower the evidence quality, the more variance researchers will find between “study results” and “real-world results”. The higher the evidence quality, the less variance between “study” and “real-world” results. In the case of saw palmetto’s effects on prostate enlargement, low-quality data suggested benefit… until higher-quality data came long that brought into question that benefit.
Saw Palmetto Versus Finasteride: Clinical Evidence
When comparing the hair regrowth data on saw palmetto to that of finasteride, the totality of evidence and quality of evidence differ significantly. For instance, finasteride has been studied for 30+ years, in over 30,000 patients, across hundreds of research groups, with dozens of randomized clinical trials – nearly all of which showed significant hair density and hair count increases.
In fact, if you just looked at the treatment arm of one of the randomized, blinded, placebo-controlled studies on oral finasteride, you’d see that the number of participants in a portion of this single study outnumber all participants across all hair growth studies evaluating saw palmetto by a factor of four.[7]Kaufman KD, Olsen EA, Whiting D, Savin R, DeVillez R, Bergfeld W, Price VH, Van Neste D, Roberts JL, Hordinsky M, Shapiro J, Binkowitz B, Gormley GJ. Finasteride in the treatment of men with … Continue reading[8]Evron E, Juhasz M, Babadjouni A, Mesinkovska NA. Natural Hair Supplement: Friend or Foe? Saw Palmetto, a Systematic Review in Alopecia. Skin Appendage Disord. 2020 Nov;6(6):329-337. doi: … Continue reading
When it comes to evidence quality and totality, combining all participants across all saw palmetto studies cannot even add up to a single treatment arm of one placebo-controlled finasteride study.[9]Kaufman KD, Olsen EA, Whiting D, Savin R, DeVillez R, Bergfeld W, Price VH, Van Neste D, Roberts JL, Hordinsky M, Shapiro J, Binkowitz B, Gormley GJ. Finasteride in the treatment of men with … Continue reading[10]Evron E, Juhasz M, Babadjouni A, Mesinkovska NA. Natural Hair Supplement: Friend or Foe? Saw Palmetto, a Systematic Review in Alopecia. Skin Appendage Disord. 2020 Nov;6(6):329-337. doi: … Continue reading
With this visual, we can really see the relative differences in evidence quality across saw palmetto and finasteride. And this is just one of the dozens of finasteride studies available.
Hierarchy of Evidence & Totality of Evidence
These comparisons illustrate two concepts: the hierarchy of evidence – which evaluates how well studies are designed – and the totality of evidence – which evaluates how much research has been done on any one intervention. The higher the hierarchy of evidence and totality of the evidence, the more likely it is that those study results reflect the real-world experience of people trying it.
We capture these concepts inside our Treatment Metrics: a standardized tool we use to help hair loss sufferers evaluate the science supporting (or not supporting) any hair loss intervention at-a-glance.
Again, for a deep-dive into these concepts, see this article.
This is important because people can use the hierarchy and totality of evidence to rank how hair loss interventions might compare to one another. At the top of the list, there are pharmaceutical options. Toward the bottom of the list, there are natural interventions – which absolutely work for some people. But again, the hierarchy and totality of evidence supporting them are more limited, which means that in real life, there will be higher variability in clinical results versus real-world results.
An example hierarchy of evidence for FDA-approved and experimental hair loss interventions.
Here’s how not understanding this can become a problem.
If you’re fighting hair loss, and you’re hit with an advertisement for a product that claims, “clinically proven to regrow hair”, it’s possible this claim is true. But if that claim is also based on a single, small-scale study funded by the company selling you that product, then it’s also true that the evidence supporting that product is not very robust and subject to bias, and that it has a lower likelihood of getting you the hair gains you desire.
In other words, that product probably ranks lower on the hierarchy of evidence and totality of the evidence. So if someone tries it, there are higher odds that the results from that single clinical study won’t reflect their real-world experience.
How Does This All Relate to Hair Loss Speeds?
If you have faster-onsetting hair loss, your opportunity costs for failed treatments are high. In a single year of failed experimentation, you might not lose 5% hair volume; you might lose 20% of your hair or more. There’s a good chance this will be cosmetically significant, which means that people with quickly-progressing hair loss don’t have the same time-freedom as people with slowly-progressing hair loss to play around with interventions that are poorly supported.
So, when considering treatments, one must remember how fast they’re losing hair.
The slower it’s progressing, the better a candidate you are for more experimental, lesser-supported interventions. The faster your hair loss, the more you should consider FDA-approved treatments that rank strongly on the hierarchy and totality of evidence.
Long story short: when fighting hair loss, time is of the essence. The speed of hair loss should always inform candidacy for novel therapies. The slower the hair loss, the better position someone is in to experiment. The faster the hair loss, the more aggressively hair loss should be treated.
References[+]
References ↑1 Rushton DH, Ramsay ID, Norris MJ, Gilkes JJ. Natural progression of male pattern baldness in young men. Clin Exp Dermatol. 1991 May;16(3):188-92. doi: 10.1111/j.1365-2230.1991.tb00343.x. PMID: 1934570. ↑2 Sinclair R. Male pattern androgenetic alopecia. BMJ. 1998 Sep 26;317(7162):865-9. doi: 10.1136/bmj.317.7162.865. PMID: 9748188; PMCID: PMC1113949. ↑3 Sinclair R, Torkamani N, Jones L. Androgenetic alopecia: new insights into the pathogenesis and mechanism of hair loss. F1000Res. 2015 Aug 19;4(F1000 Faculty Rev):585. doi: 10.12688/f1000research.6401.1. PMID: 26339482; PMCID: PMC4544386. ↑4, ↑8, ↑10 Evron E, Juhasz M, Babadjouni A, Mesinkovska NA. Natural Hair Supplement: Friend or Foe? Saw Palmetto, a Systematic Review in Alopecia. Skin Appendage Disord. 2020 Nov;6(6):329-337. doi: 10.1159/000509905. Epub 2020 Aug 23. PMID: 33313047; PMCID: PMC7706486. ↑5 Descotes, J., Rambeaud, J., Deschaseaux, P. et al. Placebo-Controlled Evaluation of the Efficacy and Tolerability of Permixon® in Benign Prostatic Hyperplasia after Exclusion of Placebo Responders. Clinical Drug Investigation 9, 291–297 (1995). https://doi.org/10.2165/00044011-199509050-00007 ↑6 Suzuki M, Ito Y, Fujino T, Abe M, Umegaki K, Onoue S, Noguchi H, Yamada S. Pharmacological effects of saw palmetto extract in the lower urinary tract. Acta Pharmacol Sin. 2009 Mar;30(3):227-81. doi: 10.1038/aps.2009.1. PMID: 19262550; PMCID: PMC4002402. ↑7, ↑9 Kaufman KD, Olsen EA, Whiting D, Savin R, DeVillez R, Bergfeld W, Price VH, Van Neste D, Roberts JL, Hordinsky M, Shapiro J, Binkowitz B, Gormley GJ. Finasteride in the treatment of men with androgenetic alopecia. Finasteride Male Pattern Hair Loss Study Group. J Am Acad Dermatol. 1998 Oct;39(4 Pt 1):578-89. doi: 10.1016/s0190-9622(98)70007-6. PMID: 9777765. Reparex Against Grey Hair is a product that claims to “restore hair color naturally from the inside out, unlike hair dyes”.[1]Reparex, (no date), Reparex Against Grey Hair. Available at: https://reparexshop.com/usa/reparex-against-grey-hair (Accessed: 30 January 2023 Reparex is owned by a company called BOOS Labs – established in 1991 – which makes many different cosmetic products.
Reparex Against Grey Hair doesn’t have any clinical efficacy and safety data associated with it and there are some inconsistencies in the information provided on their website (more on that below). However, let’s take a look at what mechanistic data might be available for this product (if any) and determine if it is a product that is worth your time and money.
Key Takeaways
- Branding. Reparex markets Against Gray Hair products as topically applied alternatives to commercially available hair dyes. Their branding is marketed towards both men and women.
- What makes it unique? Reparex attempts to differentiate itself from other hair colorant products by claiming that its product uses a unique mechanism. They state that “Reparex removes Oxygen from oxidized colorless melanin using the enzyme g-reductase which binds with silver nitrate. This results in the restoration of melanin’s natural color”.[2]Reparex, (no date), How does it work? Available at: https://reparexshop.com/usa/reparex-against-grey-hair (Accessed: 30 January 2023
- Clinical Support. Currently, no clinical data is available to show us the efficacy and safety of this product.
- Concerns.
- The major concern for this product is that there is no mechanistic, efficacy, or safety data (and the explanation they do provide doesn’t make a lot of sense). Basically, this means that we don’t know if this product actually works or whether it’s safe to use for any length of time.
- The websites and documents associated with this product include conflicting and sometimes incorrect information. This makes it confusing to navigate or really understand how the product works.
- The before-and-after photos shown on the website appear to show the same photo for both the before and after shots. Also, in some photos, it is impossible to actually tell if the after photo is of the same person as the before photo (examples below).
- Recommendations to Reparex. In order to improve their service and reassure potential customers, we would recommend that Reparex do the following:
- Take a close look at the information they are providing to customers on their websites and correct inconsistencies and mistakes where possible.
- Conduct long-term, pre-registered, placebo-controlled trials to determine the efficacy and safety of Reparex as a product that can reverse hair graying.
- Be transparent with their before-and-after photos and encourage people to take multiple photos of different angles of the face so that it is possible to identify them as the same person.
- Provide mechanistic data so we can understand exactly how Reparex works (in other words, what is the biological mechanism that their product supposedly affects?).
- Our Current Thoughts. Due to the points mentioned above, we cannot recommend Reparex as a product for reversing gray hair. The onus is on Reparex to provide clear information and clinical data to convince us that this product works.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is Reparex?
Reparex is a brand owned by a company called BOOS Labs that was established in 1991. They create multiple products including the Against Grey Hair product range. Reparex state that Against Grey Hair “Restores your own hair color, bringing back that natural look”.[3]Reparex, (no date), Reparex Against Grey Hair. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 29 January 2023
Figure 1: Example of the Reparex Against Grey Hair products. Adapted from:[4]Reparex, (no date), Reparex Against Grey Hair. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 29 January 2023
Reparex says that their product “is an outcome of life-long research made by a well-known biochemist and doctor Oto Sova, M.D, PhD. He developed and created a unique enzymatic formula which fits all people and is 100% safe for the human body”.[5]Boos Labs, (no date). How it works. Available at: https://forgreyhair.com/how-it-works (Accessed: 30 January 2023
Oto Sova has, according to the website “studied in several scientific centers in Europe and was a student of several Nobel Prize winners”.[6]For Grey Hair, (no date), For Grey Hair. Available at: https://forgreyhair.au/blog.html (Accessed: 29 January 2023
Who is their target consumer?
Reparex has products aimed at treating gray hair for both men and women. The case studies on their website include 11 men and 6 women.
What products do Reparex offer?
The Reparex range, including prices and volumes, is tabulated below.
Product Size Price Reparex Against Grey Hair for Men 150ml $54.95 Reparex Against Grey Hair for Women 150ml $54.95 Reparex Against Gray Hair for Beard and Mustache 150ml $54.95 Table 1: Prices of Reparex products. Adapted from:[7]Reparex, (no date), Reparex Shop. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 27 January 2023
Reparex also offers anti-dandruff lotions, shampoos, and skin ointments aimed at psoriasis sufferers.[8]Reparex, (no date), Reparex Shop. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 27 January 2023 These however are not part of the Against Grey Hair Range.
How do they claim these offerings are unique?
Reparex claims that their product is not a hair dye as, according to their definition, “hair dye colors your hair from the outside, but Reparex changes the hair color from the inside. It restores the original hair color, just as your hair was before it became gray”.[9]Reparex, (no date), FAQ. Available at: https://reparexshop.com/usa/faq/ (Accessed: 27 January 2023
Quite what they mean by ‘’…changes hair color from the inside.’’ isn’t clear, and the data to support their claim to this mechanism (not to mention evidence that the product actually changes hair color) is lacking. This makes it difficult to determine whether this product is actually unique.
What is their pricing?
As can be seen above, you’re looking at spending $54.95 a bottle for the specific product you want in the Against Grey Hair series, which should last you around a month.[10]Reparex, (no date), Reparex Shop. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 27 January 2023
As there don’t appear to be other products that claim to do what Reparex does, there is not much to compare the price to. But, compared to standard hair dyes, which can be very cheap at around $10, this is perhaps on the pricier side.
Product Science: Deep Dive
Firstly, let’s give a brief overview of how melanin is formed and cover some reasons why hair might turn gray.
Melanin is a type of material in your hair that gives it its color. There are two types of melanin (eumelanin and pheomelanin) and these are both created by special types of cells called melanocytes. Melanocytes are present in both the skin and hair whose primary job is to create melanin. Eumelanin is a darker pigment and is responsible for darker hair color, and pheomelanin is responsible for lighter hair color. An individual person’s hair color will be based upon a specific amount of each type of melanin and their genetics.[11]Slominski, A., Wortsman, J., Plonka, P.M., Schallreuter, K.U., Paus, R., Tobin D. (2005). Hair Follicle Pigmentation. Journal of Investigative Dermatology. 124(1), 13-21. Available at: … Continue reading
In the hair follicle, melanocytes undergo a cycle of growth (proliferation) and rest, in tandem with the hair follicle’s own growth (anagen) and non-growing (telogen) cycles. Specialized stem cells called melanocyte stem cells are located in the bulge of the hair follicle, are activated at the start of the hair follicle growing phase, and supply melanocytes to the core part (the matrix) of the hair follicle. Melanocytes then undergo multiple divisions so that there is a continuous store of melanocytes (and therefore melanin) in the bulb of the hair follicle.[12]Nishimura, E.K. (2011). Melanocyte stem cells: a melanocyte reservoir in hair follicles for hair and skin pigmentation. Pigment Cell & Melanoma Research. 24(3), 401-410. Available at: … Continue reading
Melanin is then packaged into a small ‘packet’ called a vesicle (or a melanosome) which is then transferred into the cells that make the actual substance of the hair follicle (matrix keratinocytes).[13]Schlessinger, D.I., Anoruo, M.D., Schlessinger, J. (2022). Biochemistry, Melanin, In: StatPearls, Treasure Island (FL). StatPearls publishing. Available at: … Continue reading Matrix keratinocytes are cells found in the matrix of the hair follicle, where they are highly proliferative (actively undergo cell division) to form the hair shaft you eventually see as your hair.
The synthesis of melanin involves specific biochemical reactions (called redox reactions) which are made possible by a couple of enzymes called tyrosinase and tyrosinase-related protein (TRP). These enzymes are involved at each step of the production of reactive oxygen species (ROS), such as hydrogen peroxide (H2O2) or O2- as can be seen in Figure 2. Redox reactions are chemical reactions in which a compound can either lose an electron (oxidized) or gain an electron (reduced).[14]Denat, A., Kadekaro, A.L., Marrot, L., Leachman, S, Abdel-Malek, Z.A. (2014). Melanocytes as Instigators and Victims of Oxidative Stress. Journal of Investigative Dermatology. 134(6). 1512-1518 … Continue reading
ROS are chemical compounds that contain oxygen and are therefore highly reactive, so they readily interact with the environment around them. These can cause an environment called oxidative stress which, among other things, can cause damage to melanocytes and other cells in the hair follicle.[15]NIH, (no date), Reactive oxygen species. Available at: https://cancer.gov/publications/dictionaries/cancer-terms/def/reactie-oxygen-species (Accessed: 30 January 2023
Figure 2. The synthesis of eumelanin and pheomelanin. Adapted from:[16]Denat, A., Kadekaro, A.L., Marrot, L., Leachman, S, Abdel-Malek, Z.A. (2014). Melanocytes as Instigators and Victims of Oxidative Stress. Journal of Investigative Dermatology. 134(6). 1512-1518 … Continue reading
However, the hair follicle has a natural defense against ROS -an enzyme called catalase. Catalase breaks down hydrogen peroxide over a series of chemical reactions (also redox reactions), resulting in the production of water and oxygen, and providing protection against oxidative stress.[17]Goyal, M.M., Basak, A. (2010). Human Catalase: Looking for Complete Identity. Protein & Cell. 1(10). 888-897. Available at: https://doi.org/10.1007/is13238-010-0113-z
While there are in-built mechanisms in place for reducing oxidative stress, these can be dysregulated by old age, radiation, inflammation, and psychological/emotional stress. It has been found that there is an increase in oxidative stress and death (apoptosis) of melanin-producing cells (melanocytes) in individuals with gray hairs, as well as a reduction of key protectors against oxidative stress, such as Bcl-2 (and catalase which we will go into further below) and growth factors involved in melanocyte growth such as c-Kit. This reduction in melanocytes subsequently leads to less melanin in hair shafts, giving hair a gray appearance (Figure 3).[18]Arck, P.C., Overall, R., Spatz, K., Liezman, C., Handjiski, B., Klapp, B.F., Birch-Madin, M.A., Peters, E.M.J. (2006). Towards a “free radical theory of graying”: melanocyte apoptosis in the … Continue reading
Figure 3. Hypothesized mechanisms of oxidative stress in the human hair follicle. Adapted from:[19]Arck, P.C., Overall, R., Spatz, K., Liezman, C., Handjiski, B., Klapp, B.F., Birch-Madin, M.A., Peters, E.M.J. (2006). Towards a “free radical theory of graying”: melanocyte apoptosis in the … Continue reading
A further study compared isolated growing hair follicles, dermal papilla cells (DPCs), and other specialized hair follicle cells from gray- and brown-haired donors.[20]Wood, J.M., Decker, H., Hartmann, H., Chavan, B., Rokos, H., Spencer, J.D., Hasse, S., Thornton, S.J., Shalbaf. M., Paus, R., Schallreuter, K.U. (2009). Senile hair graying: H2O2-mediated oxidative … Continue reading The researchers showed that catalase and other enzymes responsible for maintaining a healthy redox balance within the hair follicle are reduced in graying hair, leading to a negative cycle of imbalance and subsequent oxidative stress. In addition to this, hydrogen peroxide was also found to be present in the graying hair follicle whereas it was not present in the brown hair follicle. Furthermore, the researchers found that tyrosinase activity, the enzyme essential for facilitating the synthesis of melanin, was reduced after melanocytes were incubated with increasing doses of hydrogen peroxide (Figure 4).
Figure 4: Tyrosinase activity (as measured by the formation of dopachrome which tyrosinase facilitates) after increasing hydrogen peroxide treatments. Adapted from:[21]Wood, J.M., Decker, H., Hartmann, H., Chavan, B., Rokos, H., Spencer, J.D., Hasse, S., Thornton, S.J., Shalbaf. M., Paus, R., Schallreuter, K.U. (2009). Senile hair graying: H2O2-mediated oxidative … Continue reading
So, it is generally thought that oxidative stress can build up through different stressors in addition to the reactive oxygen species naturally produced through the synthesis of melanin. When oxidative stress builds up, it can reduce the activity of melanocytes and even induce them to die. In these circumstances as there is no longer enough melanin produced to provide keratinocytes with the natural pigment and hairs become gray.
But what does all this have to do with Reparex?
Reparex states that “as we get older hair turns gray due to a natural build-up of hydrogen peroxide in the hair follicles, which causes oxidative stress which oxidizes melanin and consecutively causes graying”. Then they claim that “Reparex removes Oxygen from oxidized colorless melanin using the enzyme g-reductase which binds with silver nitrate. This results in restoration of melanin’s natural color”.[22]Reparex, (no date), How does it work? Available at: https://reparexshop.com/usa/reparex-against-grey-hair (Accessed: 29 January 2023
While the statement above is an attempt to explain the mechanism of action of the Against Grey Hair products, it does not seem to fit with the current theories that state that we lose melanin rather than have colorless melanin within our hair. Additionally, the information on their website is quite confusing and inconsistent, so the only thing we can do is try to break the product down and see how it might work.
The two main ingredients in Reparex’s Against Grey Hair products are silver acetate and glucuronate reductase. Reparex claims that “glucuronate reductase…was able to remove the oxygen from hair melanine [sic] and gives it to silver nitrate”.[23]Boos Labs, (no date), Product Information File. Available at: https://www.forgreyhair.co.uk/wp-content/uploads/sites/12/2022/09/PIF-FGH.pdf (Accessed: 27 January 2023
So, let’s see what these ingredients might do…
Silver acetate…or is it silver nitrate?
Reparex uses the terms silver acetate and silver nitrate interchangeably throughout its website. While they are superficially similar chemical names, they are certainly not the same chemical. In their reasoning for including these chemicals, Reparex state that when they just used the glucuronate reductase by itself it “…took away the oxygen and the hair darkened, but after a while, the hair turned gray again, because the enzymes had no place to transfer the taken oxygen and so they put it back in the hair…therefore it was necessary to engage some ‘oxygen scavenger’ and thus the addition of a minimum amount of silver acetate. As a result, For Grey Hair has become fully functional and usable”.[24]Boos Labs, (no date), The single best treatment for gray hair invented by Oto Sova. Available at: https://forgreyhair.com.au/httpswwwforgreyhaircombest-treatment-for-grey-hair.c128.html (Accessed: 30 … Continue reading
However, with regard to silver acetate, we weren’t able to find any evidence to suggest that it can bind to oxygen or react with oxygen. Furthermore, there does not appear to be any precedence for using silver acetate in hair products.
Silver nitrate, however, can react with oxygen. Furthermore, it has been used as a hair colorant. used daily, it slowly darkens or lightens the hair. So, perhaps there is some rationale for including silver nitrate [25]Guerra-Tapia, A., Gonzalez-Guerra, E. (2014). Hair Cosmetics: Dyes. Actas Dermo-Sifiliográficas (English Edition). 105(9), 833-839. https://doi.org/10.1016j.adengl.2014.02.003
Glucuronate Reductase
Glucuronate reductase is an enzyme that belongs to a family of oxidoreductases. Oxidoreductases are enzymes that facilitate redox reactions.[26]Legesse, H.B., Assefa, B.E. (2021). Biological Application and Disease of Oxidoreductase Enzymes. Oxidoreductase. Available at: https://doi.org/10.5772/intechopen.93328 With regard to Reparex, we can hypothesize that it might work by facilitating a redox reaction in which hydrogen peroxide present in graying hair gets broken down, therefore clearing it from the hair. Perhaps this would reduce oxidative stress and prevent damage to melanocytes. Even if this was the case, would this mechanism still work to replenish already lost melanocytes? Perhaps not.
In any case, as there is no actual mechanistic data, all we can do is speculate and hypothesize, but is there any clinical information about whether this product actually works?
Does Reparex work as a hair treatment?
Unfortunately, there is no clinical data associated with this product that can tell us whether it actually works. There are some case study before-and-after photos presented on the Reparex website; however, some of these appear to actually be just the same photo twice, and it’s impossible to tell if some of the before-and-after photos are the same person, even if there are some notable changes.
Additionally, Reparex offers “2 Free Reparex products of your choice for and before and after photos from our customers”.[27]Reparex, (no date), Reparex Against Grey Hair. Available at: https://reparexshop.com/usa/reparex-against-grey-hair (Accessed: 30 January 2023 The problem with only having before-and-after photos and an incentive to provide them, is that it’s more likely that only people who have positive responses to the treatment will post their results. Furthermore, it’s possible that there are a number of people who saw no improvement, that Reparex may have chosen not to show. This can be avoided with pre-registered clinical trials with disclosed patient numbers, as they will need to show details for all the participants regardless of whether they show a response to the treatment or not.
Figure 5: Before and after photos that appear to be the same photo. Adapted from:[28]Reparex, (no date), Our Satisfied Customers. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 29 January 2023
Figure 6: Before and after photos where you cannot tell if the results are for the same person. Adapted from [29]Reparex, (no date), Our Satisfied Customers. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 29 January 2023
So, there is no clinical data and no mechanism of action data, meaning that if we did want to use it, we have to trust Reparex and its unconvincing before-and-after photos. But can we actually trust them?
Other than the confusing information on the website about their own product, Reparex also has some somewhat shaky information in their FAQs which leads us to question their overall knowledge about hair. An example is:
“Q: Does REPAREX reduce hair loss?
A: According to latest scientific research, hair loss is caused by a lack of elements such as nickel and iron. We cannot say which one of these is particularly missing for each individual therefore REPAREX cannot help your hair to grow again but we can assure you that it will not cause hair loss to start nor make it worse if you are already suffering from hair loss. Our product has no effect on hair loss.”[30]Reparex, (no date), FAQs. Available at: https://reparexshop.com/usa/faq/ (Accessed: 29 January 2023
While vitamin and mineral deficiency can certainly contribute towards hair loss, in reality, it’s not the only way that hair loss can develop.[31]Almohanna, H.M., Ahmed, A.A., Tsatalis, J.P. (2019). The Role of Vitamins and Minerals in Hair Loss: A Review. Dermatology and Therapy. 9, 51-70. Available at: … Continue reading For example, androgenetic alopecia (AGA) can be caused by an overproduction or oversensitivity to androgens (such as dihydrotestosterone); telogen effluvium can be caused by multiple triggering events, including pregnancy; alopecia areata can be caused as a function of autoimmune dysregulation (to name a few).[32]Alessandrini, A., Bruni, F., Piraccini, B.M., Starace, M. (2020). Common causes of hair loss – clinical manifestations, trichoscopy and therapy. Journal of the European Academy of Dermatology and … Continue reading
Is Reparex Against Grey Hair safe?
Reparex states that “REPAREX has been carefully tested according to the latest EC regulations for cosmetic products; this includes testing for heavy metal content, skin irritation, and any general harm. It has also been evaluated by independent Cosmetic Product Safety Assessors. Furthermore, REPAREX has also been registered at the Central Registration of Cosmetic Products in Brussels and according to its status as harmless it was released to the EU market as harmless and 100% legal.”[33]Reparex, (no date) FAQ. Available at: https://reparexshop.com/usa/faq/ (Accessed: 29 January 2023
However, to our knowledge, there has been no published efficacy or safety data for this product, so we cannot say with certainty that this product is safe to use long-term. It’s also worth noting there are dozens of examples whereby short-term (i.e., 1-2 year) data suggested that a natural substance might be safe, only for long-term (i.e., 5-10+ year) data to show the exact opposite. One example: the effects of vitamin E and selenium supplements on prostate cancer. Short-term data suggested benefit, while long-term data showed these supplements doubled the rates of prostate cancer in men with already-adequate vitamin E and selenium levels.
Should I use Reparex?
You may consider trying out this product if:
- You are unhappy with your gray hair
- You do not want to use other hair dyes
- You are happy using products that have no efficacy or safety data
- You are ok buying a product from a company that has confusing and incorrect information on their website
You may be better placed however to just use a standard hair dye, which you can buy for a fraction of the price.
Recommendations to the company
We would recommend that Reparex look at the information that they are showing on their websites and make sure that it is consistent with (1) the actual ingredients in the product and (2) current scientific data. Furthermore, we recommend that Reparex conduct some mechanistic and long-term pre-registered clinical trials to determine the efficacy and safety of Reparex as a product that can reverse hair graying. Additionally, Reparex should address the issues with their before-and-after photos and make sure that they are not the same photos, and that people can be clearly identified as the same person.
Final thoughts
If you are comfortable trying products with zero published clinical or mechanistic data, and you do not want to use hair dyes, then Reparex might be something you could consider experimenting with. Otherwise, we do not recommend using this product in its current state.
References[+]
References ↑1, ↑27 Reparex, (no date), Reparex Against Grey Hair. Available at: https://reparexshop.com/usa/reparex-against-grey-hair (Accessed: 30 January 2023 ↑2 Reparex, (no date), How does it work? Available at: https://reparexshop.com/usa/reparex-against-grey-hair (Accessed: 30 January 2023 ↑3, ↑4 Reparex, (no date), Reparex Against Grey Hair. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 29 January 2023 ↑5 Boos Labs, (no date). How it works. Available at: https://forgreyhair.com/how-it-works (Accessed: 30 January 2023 ↑6 For Grey Hair, (no date), For Grey Hair. Available at: https://forgreyhair.au/blog.html (Accessed: 29 January 2023 ↑7, ↑8, ↑10 Reparex, (no date), Reparex Shop. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 27 January 2023 ↑9 Reparex, (no date), FAQ. Available at: https://reparexshop.com/usa/faq/ (Accessed: 27 January 2023 ↑11 Slominski, A., Wortsman, J., Plonka, P.M., Schallreuter, K.U., Paus, R., Tobin D. (2005). Hair Follicle Pigmentation. Journal of Investigative Dermatology. 124(1), 13-21. Available at: https://doi.org/10.1111/j.0022-202X.2004.23528.x ↑12 Nishimura, E.K. (2011). Melanocyte stem cells: a melanocyte reservoir in hair follicles for hair and skin pigmentation. Pigment Cell & Melanoma Research. 24(3), 401-410. Available at: https://doi.org/10.1111/j.1755-148X.2011.00855.x ↑13 Schlessinger, D.I., Anoruo, M.D., Schlessinger, J. (2022). Biochemistry, Melanin, In: StatPearls, Treasure Island (FL). StatPearls publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459156/ (Accessed: 30 January 2023 ↑14, ↑16 Denat, A., Kadekaro, A.L., Marrot, L., Leachman, S, Abdel-Malek, Z.A. (2014). Melanocytes as Instigators and Victims of Oxidative Stress. Journal of Investigative Dermatology. 134(6). 1512-1518 Available at: https://doi.org/10.1038/jid.2014.65 ↑15 NIH, (no date), Reactive oxygen species. Available at: https://cancer.gov/publications/dictionaries/cancer-terms/def/reactie-oxygen-species (Accessed: 30 January 2023 ↑17 Goyal, M.M., Basak, A. (2010). Human Catalase: Looking for Complete Identity. Protein & Cell. 1(10). 888-897. Available at: https://doi.org/10.1007/is13238-010-0113-z ↑18 Arck, P.C., Overall, R., Spatz, K., Liezman, C., Handjiski, B., Klapp, B.F., Birch-Madin, M.A., Peters, E.M.J. (2006). Towards a “free radical theory of graying”: melanocyte apoptosis in the aging human hair follicle is an indicator of oxidative stress induced tissue damage. The FASEB Journal. 20(9), 1567-1569. Available at: https://doi.org/10.1096/fj.05-04039fje ↑19 Arck, P.C., Overall, R., Spatz, K., Liezman, C., Handjiski, B., Klapp, B.F., Birch-Madin, M.A., Peters, E.M.J. (2006). Towards a “free radical theory of graying”: melanocyte apoptosis in the aging human hair follicle is an indicator of oxidative stress induced tissue damage. The FASEB Journal. 20(9), 1567-1569. Available at: https://doi.org/10.1096/fj.05-04039fje ↑20 Wood, J.M., Decker, H., Hartmann, H., Chavan, B., Rokos, H., Spencer, J.D., Hasse, S., Thornton, S.J., Shalbaf. M., Paus, R., Schallreuter, K.U. (2009). Senile hair graying: H2O2-mediated oxidative stress affects human hair color by blunting methionine and sulfoxide repair. The FASEB Journal. 23(7), 2015-2336. Available at: https://doi.org/10.1096/fj.08-125435 ↑21 Wood, J.M., Decker, H., Hartmann, H., Chavan, B., Rokos, H., Spencer, J.D., Hasse, S., Thornton, S.J., Shalbaf. M., Paus, R., Schallreuter, K.U. (2009). Senile hair graying: H2O2-mediated oxidative stress affects human hair color by blunting methionine and sulfoxide repair. The FASEB Journal. 23(7), 2015-2336. Available at: https://doi.org/10.1096/fj.08-125435 ↑22 Reparex, (no date), How does it work? Available at: https://reparexshop.com/usa/reparex-against-grey-hair (Accessed: 29 January 2023 ↑23 Boos Labs, (no date), Product Information File. Available at: https://www.forgreyhair.co.uk/wp-content/uploads/sites/12/2022/09/PIF-FGH.pdf (Accessed: 27 January 2023 ↑24 Boos Labs, (no date), The single best treatment for gray hair invented by Oto Sova. Available at: https://forgreyhair.com.au/httpswwwforgreyhaircombest-treatment-for-grey-hair.c128.html (Accessed: 30 January 2023 ↑25 Guerra-Tapia, A., Gonzalez-Guerra, E. (2014). Hair Cosmetics: Dyes. Actas Dermo-Sifiliográficas (English Edition). 105(9), 833-839. https://doi.org/10.1016j.adengl.2014.02.003 ↑26 Legesse, H.B., Assefa, B.E. (2021). Biological Application and Disease of Oxidoreductase Enzymes. Oxidoreductase. Available at: https://doi.org/10.5772/intechopen.93328 ↑28, ↑29 Reparex, (no date), Our Satisfied Customers. Available at: https://reparexshop.com/usa/reparex-against-grey-hair/ (Accessed: 29 January 2023 ↑30 Reparex, (no date), FAQs. Available at: https://reparexshop.com/usa/faq/ (Accessed: 29 January 2023 ↑31 Almohanna, H.M., Ahmed, A.A., Tsatalis, J.P. (2019). The Role of Vitamins and Minerals in Hair Loss: A Review. Dermatology and Therapy. 9, 51-70. Available at: https://doi.org/10.1007/s13555-018-0278-6 ↑32 Alessandrini, A., Bruni, F., Piraccini, B.M., Starace, M. (2020). Common causes of hair loss – clinical manifestations, trichoscopy and therapy. Journal of the European Academy of Dermatology and Venereology. 35, 629-640. Available at: https://doi.org/10.1111/jdv.17079 ↑33 Reparex, (no date) FAQ. Available at: https://reparexshop.com/usa/faq/ (Accessed: 29 January 2023 Ketoconazole is used off-label to treat androgenic alopecia and telogen effluvium. While it is well-studied in men, there is a significant lack of clinical data showing its efficacy in women. In this guide, we will explore the evidence supporting the use of ketoconazole in androgenic alopecia, as well as answer whether it is suitable for use in women.
What is Ketoconazole?
Ketoconazole, primarily an antifungal drug, is commonly employed to combat diverse fungal infections within the body. Interestingly, it also finds application in addressing hair loss issues, including androgenic alopecia (AGA) and telogen effluvium (TE), typically through topical formulations and shampoos. Certain products containing ketoconazole for hair loss are accessible without a prescription, like shampoos containing 1% ketoconazole. Medical practitioners might advise or provide more potent ketoconazole treatments in specific cases.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

How Does Ketoconazole Work?
Ketoconazole functions as an antifungal agent by disrupting the cell membranes of fungi, impeding their growth and replication. Its antifungal properties are beneficial for addressing scalp conditions by reducing fungal activity and inflammation. In hair loss conditions like AGA and TE, ketoconazole contributes to a healthier and less inflamed scalp, creating a more conducive environment for growth.
Moreover, recent studies have suggested that ketoconazole shampoo may lower dihydrotestosterone (DHT) levels by inhibiting five alpha-reductases. Combined with treatments like finasteride, this can offer a more comprehensive approach to addressing these conditions.[1]Perez, B.S.H. (2004). Ketoconazole as an adjunct to finasteride in treating androgenetic alopecia in men. Medical Hypotheses. 62(1). 112-115. Available at: … Continue reading
What Evidence is there for Ketoconazole in Hair Loss?
The effectiveness of ketoconazole in treating hair loss, particularly in conditions such as AGA and TE is supported by various clinical studies. These studies have explored the impact of ketoconazole not only as a standalone treatment but also in combination with other hair loss therapies.
Study One
This study involved 39 male participants exclusively with androgenic alopecia (AGA); the effects of 2% ketoconazole shampoo were compared to those of regular shampoo over 21 months. 27 men used the ketoconazole shampoo, while 12 used a regular shampoo. Additionally, 22 individuals without AGA served as controls, half using ketoconazole and the other half using regular shampoo. The results revealed a significant difference between the two groups.
Results
Among the non-AGA control participants, the choice of shampoo had no discernable impact on their AGA pilary index (defined as the product of the percentage of hairs in the growth (anagen) phase and average diameter (in micrometers) of the hair shaft).
Conversely, among the participants with AGA who used an unmedicated shampoo, there was a gradual linear decline in their AGA pilary index over time. In contrast, the group using the ketoconazole shampoo exhibited a progressive increase in their AGA pilary index, and this effect became noticeable after six months. The increase seemed to plateau after approximately 15 months of using the ketoconazole shampoo.[2]Piérard-Franchimont, C., De Doncker, P., Cauwenbergh, G., Piérard, G.E. (1998). Ketoconazole shampoo: effect of long-term use in androgenic alopecia. Dermatology. 196(4). 474-477. Available at: … Continue reading
Study Two
Another study involved 150 male participants experiencing TE-related to AGA with associated dandruff. During the study, 150 male participants were split into three groups, and each group was given a different shampoo to use. One group used a shampoo containing 1% ketoconazole, another group used a shampoo with 1% piroctone olamine, and the third group used a shampoo with 1% zinc pyrithione.
The researchers measured hair shedding, hair density, the percentage of anagen (growth phase) hair, the average diameter of proximal hair shafts, and sebum excretion rates to evaluate the effectiveness of each shampoo.
Results
The study results indicated that all three shampoo formulations promptly addressed pruritus (itching) and dandruff symptoms, leading to rapid clearance. No significant changes were observed in any of the three shampoo groups regarding hair density.
However, there was a noteworthy reduction in all three groups regarding hair shedding. The ketoconazole group experienced a 17.3% decrease, the piroctone olamine group saw a 16.5% reduction, and the zinc pyrithione group had a 10.1% decrease in hair shedding.
Furthermore, the percentage of anagen hair increased in all three shampoo groups. The ketoconazole group exhibited a 4.9% rise, the piroctone olamine group showed a 7.9% increase, and the zinc pyrithione group demonstrated a 6.8% increase.
All groups showed a decrease in sebum secretion rates, with the ketoconazole group experiencing a 4.8% reduction, the piroctone olamine group showing a 2.9% decrease, and the zinc pyrithione group recording a 5.5% decline.[3]Piérard-Franchimont, C., Goffin, V., Henry, F., Uhoda, I., Braham, C., Piérard, G.E. (2002). Nudging hair shedding by antidandruff shampoos. A comparison of 1% ketoconazole, 1% piroctone olamine, … Continue reading
Other Studies
Two other studies evaluated the efficacy of ketoconazole in combination with other hair loss treatments like finasteride and minoxidil in men with AGA. They found it works well as a combination therapy and can even improve AGA in men with atopic and/or seborrheic dermatitis.
So, clinical evidence shows that ketoconazole can improve hair loss outcomes. However, all these studies suffer from a significant limitation; they have only included male subjects. Let’s find out if there is evidence for using ketoconazole in women.
Clinical Evidence for Ketoconazole for Women
There is currently no published evidence for using ketoconazole shampoo in women. However, one study did compare the efficacy of a 2% ketoconazole solution to 2% minoxidil in female pattern hair loss. The study involved 40 female pattern hair loss patients. 20 were in Group A using 2% topical minoxidil, and 20 were in Group B treated with 2% topical ketoconazole. Both groups received treatment for six months, with changes to the Ludwig scale and trichoscopic (magnified images of the scalp, typically used for counting hairs) outcomes evaluated.
Results
The results showed that both groups experienced improved hair growth (Figure 1 & 2), but the minoxidil group responded faster. In contrast, the ketoconazole group had a delayed response, which became significant at the 6-month. Side effects were also less common in the ketoconazole group (10% vs. 55% in the minoxidil group), and patient satisfaction did not significantly differ between the two groups.[4]El-Garf, A., Mohie, M., Salah, E. (2019). Trichogenic effect of topical ketoconazole versus minoxidil 2% in female pattern hair loss: a clinical and trichoscopic evaluation. Biomed Dermatol. 3(8). … Continue reading
Figure 1: Example of the effect of topical ketoconazole on hair growth at baseline (a,e), after 2 months (b,f), after 4 months (c,g), and after 6 months (d, h).[5]El-Garf, A., Mohie, M., Salah, E. (2019). Trichogenic effect of topical ketoconazole versus minoxidil 2% in female pattern hair loss: a clinical and trichoscopic evaluation. Biomed Dermatol. 3(8). … Continue reading
Figure 2: Example of the effect of topical minoxidil at baseline (a,e), after 2 months (b,f), after 4 months (c,g), and after 6 months (d, h).[6]El-Garf, A., Mohie, M., Salah, E. (2019). Trichogenic effect of topical ketoconazole versus minoxidil 2% in female pattern hair loss: a clinical and trichoscopic evaluation. Biomed Dermatol. 3(8). … Continue reading
The study indicates that applying ketoconazole topically can facilitate hair regrowth in women with fewer side effects than minoxidil. Ketoconazole is probably as effective for women as it is for men. However, additional research is necessary to obtain a more comprehensive understanding of its efficacy and safety.
Can I Use Ketoconazole If I am Pregnant or Breastfeeding?
We always recommend a trip to the doctor before using any product if you are pregnant or breastfeeding. While certain patient informational leaflets suggest ketoconazole shampoo can be used during pregnancy and breastfeeding, the ketoconazole dilutions in those leaflets only reference products with 20 mg per gram of ketoconazole.[7]Nizoral, (no date). Nizoral Anti-Dandruff Shampoo Ketoconazole. Nizoral. Available at: https://www.medicines.org.uk/emc/files/pil.6456.pdf (Accessed: 03 November 2023) Be sure to check with your doctor to confirm your dilution of ketoconazole shampoo matches that of 20 mg/gram, and that your doctor also agrees with these recommendations.
Can I Use Ketoconazole Alongside Other Hair Loss Medications?
Researchers have observed that combining ketoconazole with other treatments works best in treating AGA in humans. This is because ketoconazole has different mechanisms of action than minoxidil, microneedling, and finasteride. Targeting multiple mechanisms generally leads to better results. If you’re interested in seeing a real-life example of hair regrowth achieved using ketoconazole in combination with other treatments, you can find it here.
References[+]
References ↑1 Perez, B.S.H. (2004). Ketoconazole as an adjunct to finasteride in treating androgenetic alopecia in men. Medical Hypotheses. 62(1). 112-115. Available at: https://doi.org/10.1016/s0306-9877(03)00264-0 ↑2 Piérard-Franchimont, C., De Doncker, P., Cauwenbergh, G., Piérard, G.E. (1998). Ketoconazole shampoo: effect of long-term use in androgenic alopecia. Dermatology. 196(4). 474-477. Available at: https://doi.org/10.1159/000017954 ↑3 Piérard-Franchimont, C., Goffin, V., Henry, F., Uhoda, I., Braham, C., Piérard, G.E. (2002). Nudging hair shedding by antidandruff shampoos. A comparison of 1% ketoconazole, 1% piroctone olamine, and 1% zinc pyrithione formulations. International Journal of Cosmetic Science. 24(5). 249-256. Available at: https://doi.org/10.1046/j.1467-2494.2002.00145.x ↑4, ↑5, ↑6 El-Garf, A., Mohie, M., Salah, E. (2019). Trichogenic effect of topical ketoconazole versus minoxidil 2% in female pattern hair loss: a clinical and trichoscopic evaluation. Biomed Dermatol. 3(8). Available at: https://doi.org/10.1186/s41702-019-0046-y ↑7 Nizoral, (no date). Nizoral Anti-Dandruff Shampoo Ketoconazole. Nizoral. Available at: https://www.medicines.org.uk/emc/files/pil.6456.pdf (Accessed: 03 November 2023) What is Ketoconazole?
Ketoconazole is an antifungal medication frequently used to treat various fungal infections around the body, including the scalp. It has also proven effective in managing hair loss problems, such as androgenic alopecia (AGA) and telogen effluvium (TE), typically through topical forms like shampoos.
One of the advantages of using ketoconazole for hair loss is that it has a low risk of causing side effects in most people. Some products with ketoconazole, like 1% ketoconazole shampoos, are also available over the counter without a prescription. Healthcare professionals may recommend or prescribe stronger ketoconazole treatments for specific cases in certain situations – with 2% ketoconazole shampoos showing clinical effectiveness in treating androgenic alopecia.
With that said, a portion of people do experience side effects from ketoconazole. With no roadmap to resolve these side effects, these users will often discontinue the medication – thereby forfeiting the hair gains they could’ve experienced had they found a way to resolve those adverse events.
In this article, we’ll explore what these side effects are, and how most of these side effects can be mitigated, minimized, and even resolved with proper troubleshooting.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What are the Common Side Effects of Ketoconazole Shampoo?
While oral ketoconazole has notable risks associated with side effects, the use of 1-2% ketoconazole shampoo appears to have minimal, if any, side effects due to its limited exposure time and low absorption into the bloodstream compared to the oral form. Nevertheless, there are instances where individuals using ketoconazole shampoo may encounter adverse effects. These occurrences could include:[1]Drugs.com (2023). Nizoral Shampoo Side Effects. Available at: https://www.drugs.com/sfx/nizoral-shampoo-side-effects.html (Accessed: 26 October 2023)
- Skin irritation
- Itching
- Stinging or burning
- Blistering
- Dry skin
- Increased hair shedding
In very rare cases, some people also report hair discoloration.[2]Kuibicki, S.L., Damanpour, S., Mann, R. (2020). Ketoconazole shampoo-induced hair discoloration. International Journal of Women’s Dermatology. 6(2). 121-122. Available at: … Continue reading
What Should I Do to Combat These Side Effects?
If you’ve begun to experience side effects from using ketoconazole shampoo, it’s crucial to take proactive steps to mitigate these effects so you can still benefit from the treatment. Understanding how to manage these side effects can make a significant difference in your comfort and the effectiveness of the shampoo. It’s important to remember that while most side effects are mild and manageable, they are still noteworthy and require appropriate action to ensure they don’t escalate or adversely affect your hair and scalp health.
Scalp Dryness, Hair Dryness, Dandruff, and/or Itchiness
If you experience abnormal hair texture, scalp or hair dryness, dandruff, and/or itchiness, you should consider the following:
- Switch from 2% to 1% ketoconazole. This should reduce the “power” of ketoconazole and, thereby, its drying effect on the hair.
- Reduce ketoconazole’s usage frequency and/or scalp contact time. While ketoconazole shampoo is typically used 2-4 times weekly and left on the scalp for 5-15 minutes, these usage parameters can irritate many peoples’ scalps. The simplest way to troubleshoot this is to reduce your use. Opt for 1-2 times weekly ketoconazole shampooing and/or only leave in the shampoo for 2-5 minutes.
- Add in a conditioner. After shampooing with ketoconazole, add in a conditioner. This should help moisturize the scalp and hair, reducing hair texture changes caused by scalp/hair dryness.
Hair Shedding
Understanding the reasons behind hair shedding is important when using ketoconazole shampoo, as it helps in distinguishing between normal hair loss and the potential side effects of the treatments. Various factors can influence hair shedding, and it’s important to identify whether this shedding is (1) a positive shed in response to starting ketoconazole, (2) a reaction to the ketoconazole itself, and/or (3) if this hair shedding is actually coincidental to your introduction of ketoconazole, and is instead caused by other factors: seasonal hair cycling, the introduction or withdrawal of other hair loss treatments, and/or telogen effluvium sheds.
Medical and legal consensus – with any treatment-related side effect – is to stop that treatment and consult with your doctor immediately. Nonetheless, we’ll go through a few of these situations below, along with potential troubleshooting advice for resolution:
Scalp Issues
If your hair shedding is accompanied by scalp dryness, hair dryness, and/or itchiness, then this might be a reaction from the ketoconazole shampoo, and you can follow the above-mentioned measures to mitigate the side effects.
If your hair shedding is accompanied by scalp redness, then there is a slight possibility that you are having a very rare allergic reaction to the shampoo. In cases like this, we recommend stopping the ketoconazole and seeing a doctor or dermatologist who can further assess your tolerability. While allergic reactions to ketoconazole are rare, it is usually best to err on the side of caution – especially as ketoconazole tends to be a lower-leverage treatment option (meaning that it often does not produce vast amounts of hair regrowth).
Scalp Adjustment to Treatment
If any other side effects do not accompany your hair shedding and you have just started ketoconazole in the last 3 months, then it may just be that your scalp is still adjusting (and responding) to new treatments. Therefore, it might be that some of your shedding is due to a positive treatment response. We’ll have more articles about this soon.
Seasonal Shedding
Sometimes, increases to hair shedding have nothing to do with your hair loss treatments and, instead, are simply a function of seasonal hair shedding.
Humans undergo a temporary uptick in shedding due to hair cycle seasonality. In the northern hemisphere, these upticks typically occur in July and August, then settle into lower shedding rates in winter. While this shedding is mostly unavoidable, there’s also good news: it doesn’t really interfere with the success of your long-term hair loss treatments. So, if you’re within peak windows of time for seasonal hair shedding, you may want to consider that at least some of this shedding might not be due to ketoconazole, but instead, due to seasonality.
Recent Introduction/Withdrawal of Other Treatments
It may also be that the hair shedding might not be related to ketoconazole use. If you have withdrawn from or introduced other hair loss treatments within the last three months, these changes may also explain recent upticks to hair shedding.
Skin Burning, Peeling, or Redness
As mentioned above, scalp redness has a slight possibility of being a rare allergic reaction to the shampoo. We recommend stopping using the shampoo and seeing your doctor or dermatologist for advice.
Hair Discoloration
Hair discoloration is a rarer side effect of ketoconazole shampoo, but a few long-term treatment users have reported it. Under these circumstances, we recommend you stop using ketoconazole shampoo and instead switch to other shampoos with anti-dandruff and antifungal properties, but that work through different mechanisms and thus may not evoke the same effect. Consider shampoos with the following active ingredients: selenium sulfide and/or zinc pyrithione.
Shampoos with these ingredients are widely sold over the counter and are specifically formulated to reduce dandruff and skin flaking. There’s also some evidence that they may support hair growth in those with androgenic alopecia, female pattern hair loss, and/or telogen effluvium associated with microorganism overgrowths.[3]Trueb, R.M., Henry, J.P., Davis, M.G., Schwartz, J.R. (2018). Scalp Condition Impacts Hair Growth and Retention via Oxidative Stress. International Journal of Trichology. 10(6), 262-270. Available … Continue reading,[4]McGinley, K.J., Leyden, J.J. (1982). Antifungal activity of dermatological shampoos. Archives of Dermatological Research. 272(3-4). 339-342. Available at: https://doi.org/10.1007/BF00509065
Other Side Effects
If you experience any other side effects and want advice from the community, feel free to make a forum post describing your growth regimen, ketoconazole shampoo routine, and specific side effects. Our team and community will chime in with resources and strategies to help you resolve this. You can post your questions here.
References[+]
References ↑1 Drugs.com (2023). Nizoral Shampoo Side Effects. Available at: https://www.drugs.com/sfx/nizoral-shampoo-side-effects.html (Accessed: 26 October 2023) ↑2 Kuibicki, S.L., Damanpour, S., Mann, R. (2020). Ketoconazole shampoo-induced hair discoloration. International Journal of Women’s Dermatology. 6(2). 121-122. Available at: https://doi.org/10.1016/j.ijwd.2019.10.010 ↑3 Trueb, R.M., Henry, J.P., Davis, M.G., Schwartz, J.R. (2018). Scalp Condition Impacts Hair Growth and Retention via Oxidative Stress. International Journal of Trichology. 10(6), 262-270. Available at: https://doi.org/10.4103/ijt.ijt_57_18 ↑4 McGinley, K.J., Leyden, J.J. (1982). Antifungal activity of dermatological shampoos. Archives of Dermatological Research. 272(3-4). 339-342. Available at: https://doi.org/10.1007/BF00509065 Is hair loss treatment lifelong? It can be daunting to think that’s the case, as it seems quite a commitment. But while it’s true for most cases of androgenic alopecia, lifelong hair loss treatment may not be as scary as it seems. In this article, we will delve into the effects of stopping hair loss treatments and how a shift in perspective can improve how we feel about “lifelong” hair loss treatments.
Is Hair Loss Treatment Lifelong?
The short answer is yes: hair loss treatments must be continued, or results gained will be lost. This is at least true for most cases of androgenic alopecia (more on this below). The longer answer is that:
- This isn’t true for all hair loss cases. There are plenty of situations where hair loss treatments are only temporary, as the hair regrowth sustains even after quitting. It depends on the type(s) of hair loss.
- “Lifelong” treatments aren’t as scary as they seem. The fact that some treatments might require a lifelong commitment should never be a reason not to try that same treatment, at least today.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Let’s first look at what we know about what happens when you quit a hair loss treatment.
What Happens if I Quit a Hair Loss Treatment?
Luckily, some studies explain what happens when you quit traditional hair loss treatments like minoxidil and finasteride. There is even a study looking at what happens if you stop microneedling.
What Happens if I Quit Minoxidil?
In 1999, a study explored the implications of discontinuing minoxidil after long-term use. The study yielded intriguing results, as the group that ceased minoxidil treatment observed a period of increased hair shedding and a temporary drop in hair counts, falling below their pre-treatment levels.
Four groups of 9 men with AGA were followed over two years, with each group receiving either 2% minoxidil, 5% minoxidil, a placebo, or no treatment. The 2% and 5% minoxidil groups displayed a notable increase in hair counts after three months, which reached a plateau but remained higher than those observed in the placebo and control groups.
Approximately two years into the study, at the 96-week mark, the individuals in the 2% and 5% minoxidil groups stopped their treatments. This discontinuation is evident in the data related to hair weights, which began to decline shortly afterward (see Figure 1). Three months later, around week 108, their hair loss had fallen well below the levels seen in the placebo group, even dipping below their initial hair counts. However, by week 120, three months later, the 2% and 5% minoxidil groups had rebounded and returned to a level comparable to their baseline hair counts before the study began.
Figure 1: Changes in hair weight and hair count in men with androgenetic alopecia after application of 5% and 2% topical minoxidil, placebo, or no treatment. The line at 96 weeks shows the time when minoxidil treatment was stopped.[1]Price, V.H., Menefee, E., Strauss, P.C., (1999). Changes in hair weight and hair count in men with androgenetic alopecia after application of 5% and 2% topical minoxidil, placebo, or no treatment. … Continue reading
It should be noted that any excess hair shedding experienced during this transition phase is usually not a permanent condition. With time, the hair adjusts to a new equilibrium without the presence of the drug, and excessive shedding should subside, returning to pre-treatment levels.
What Happens if I Quit Finasteride?
The informational insert for Propecia, a finasteride brand, indicates that hair loss typically resumes within 3 to 12 months after stopping the medication, and hair counts may revert to pre-treatment levels. This conclusion is grounded in the results from Phase II and III clinical trials, which were crucial for the FDA’s approval of finasteride for treating androgenic alopecia.
In these trials, a subset of participants received finasteride for an entire year. Subsequently, they were unknowingly switched to a group that received a placebo (a sugar pill) during the second year, corresponding to months 12-24 of the study. The researchers closely monitored and documented changes in hair counts for these participants from the start (month 0) throughout 24 months. They then compared these changes with those who continued using finasteride throughout the study and those who consistently received the placebo.[2]Kaufman, K.D., Olsen, E.A., Whiting, D., Savin, R., DeVillez, R., Bergfeld, W., Price, V.H., van Neste, D., Roberts, J.L., Hordinsky, M., Shapiro, J., Binkowitz, B., Gormley, G.J. (1998). Finasteride … Continue reading
What the Findings Say
The study revealed that ceasing finasteride and switching to placebo resulted in hair counts falling back to their initial levels, or even slightly below, within 12 months after stopping the medication (Figure 2).
Figure 2: Hair count mean change from baseline. Fin – Pbo = the group who initially took finasteride and then were unknowingly switched to placebo.[3]Kaufman, K.D., Olsen, E.A., Whiting, D., Savin, R., DeVillez, R., Bergfeld, W., Price, V.H., van Neste, D., Roberts, J.L., Hordinsky, M., Shapiro, J., Binkowitz, B., Gormley, G.J. (1998). Finasteride … Continue reading
However, there are also interesting studies that can provide information about taking a break from finasteride.
Biological Effects of Finasteride After Quitting
Because finasteride has a terminal half-life of 5-7 hours, and it takes about 4-5 days for the drug to fully dissociate from tissues, its biological effects on hormone profiles can persist for approximately 30 days after discontinuation.
In practical terms, this means finasteride can continue to have a therapeutic impact in reducing scalp levels of dihydrotestosterone (DHT) even several weeks after discontinuing the medication (see Figure 3).
Figure 3: Serum DHT concentration before and after quitting finasteride treatment.[4]Clark, R.V., Hermann, D.J., Cunningham, G.R., Wilson, T.H., Morrill, B.B., Hobbs, S. (2004). Marked Suppression of Dihydrotestosterone in Men with Benign Prostatic Hyperplasia by Dutasteride, a Dual … Continue reading
Exploring Alternative Finasteride Dosing Schedules
A study investigated whether a daily dose of 1 mg was necessary to maintain hair regrowth. Initially, a group of men was placed on a daily 1 mg finasteride regimen for a year. In the second year, the men were divided into two groups: one continued to take finasteride daily, while the other group adopted a 30-days-on, 30-days-off dosing schedule.[5]Kim, K.H., Park, S.M., Lee, Y.J., Sim, W.Y., Lew, B.L. (2020). Similar efficacy of maintenance treatment of finasteride 1 mg every other month compared with finasteride 1 mg daily in Korean men with … Continue reading
The second group used finasteride for only half the time (i.e., 6 months as opposed to 12 months), yet both groups experienced similar improvements in hair parameters during the second year.
The underlying hypothesis for this result was that finasteride’s pharmacokinetics might allow for dosing schedules that alternate monthly. This approach could potentially accommodate those who wish to reduce their drug exposure or take breaks from the medication without significantly compromising their hair gains.
What If I Need To Stop Taking Finasteride For Any Other Reason?
When pausing finasteride use for an extended period exceeding 30 days, there is a higher risk of hair loss resuming due to the dissipation of the drug’s effects on scalp DHT levels. Both clinical withdrawal studies and anecdotal reports from finasteride users support this phenomenon.
Hair loss may not immediately return for many individuals but might become noticeable around the second or third month after quitting. To maintain the benefits of the drug on hair health, it is advisable to keep the withdrawal period beyond 30 days as short as possible.
If you want to learn more about the pharmacokinetics of finasteride and how you can maximize your treatment usage, you can follow these links:
- Finasteride: How Long Does It Stay In The Bloodstream?
- Finasteride: How Long Does It Stay Active in Scalp Tissue?
- What Happens If I Stop Using Finasteride?
What Happens if I Quit Microneedling?
Currently, there is only one clinical study evaluating the effects of microneedling cessation. This study compared the effects of using minoxidil only, microneedling only, and using both minoxidil and microneedling together.[6]Bao, L., Zong, H., Fang, S., Zheng, L.i, Y. (2022). Randomized trial of electrodynamic microneedling combined with 5% minoxidil topical solution for treating androgenetic alopecia in Chinese males … Continue reading
The study involved 71 male participants with androgenetic alopecia (AGA), divided into three distinct treatment groups:
- 5% minoxidil applied twice daily for 24 weeks (23 participants).
- Microneedling sessions were conducted every 3 weeks, totaling 8 treatments (23 participants).
- A combination of both treatments over 24 weeks (25 participants).
The researchers assessed changes in hair density and diameter at three-week intervals and conducted a six-month follow-up after the final treatment.
What the Findings Say
All groups exhibited significant increases in non-vellus hair density three weeks post-treatment. Notably, the combination group showed the most substantial increase in non-vellus hair density (56.45±7.82 roots per cm²), outperforming the ~28 increase in the minoxidil group and ~32 in the microneedling group.
These findings align with earlier research, particularly a paper by Dhurat et al., highlighting microneedling’s role in enhancing minoxidil’s effectiveness.
Six-Month Follow-Up Insights
Six months after the completion of the treatments, the study revealed intriguing long-term effects:
- In the minoxidil-only group, 90% of participants lost all newly acquired hair within six months post-treatment cessation, a finding consistent with previous minoxidil research.
- Conversely, in both the microneedling-only and the combination groups, 70% of participants retained some new hair, and 20% maintained all new hair growth (referenced in Figure 4).
Figure 4 illustrates the comparative hair regrowth across the three groups during the initial 24 weeks of treatment and the subsequent 24 weeks post-treatment.
Figure 4: The effect of a) minoxidil-only, b) microneedling-only, and c) minoxidil and microneedling on hair regrowth during the initial 24 weeks of treatment, and a further 24 weeks after treatment.[7]Bao, L., Zong, H., Fang, S., Zheng, L.i, Y. (2022). Randomized trial of electrodynamic microneedling combined with 5% minoxidil topical solution for treating androgenetic alopecia in Chinese males … Continue reading
These results suggest that microneedling, alone and in combination with minoxidil, offers more durable effects on hair maintenance, even after treatment discontinuation. The sustained impact in the combination group also indicates that microneedling may enhance minoxidil’s long-term effectiveness.
In summary, while managing hair loss often requires lifelong treatment, there are instances where benefits can continue even after the cessation of certain therapies. Studies have shown that minoxidil and finasteride necessitate ongoing use to maintain hair growth, as discontinuation can reverse benefits. However, treatments such as microneedling, alone or in combination with minoxidil, have demonstrated more enduring effects, offering sustained hair maintenance even after stopping the treatment.
How Can We Change Our Mindset About “Lifelong” Hair Loss Treatments?
Changing our mindset about lifelong hair loss treatment involves embracing it as a part of routine self-care, much like daily exercise or a balanced diet. It’s about viewing these treatments not as burdensome but as an empowering step toward self-confidence and well-being. Recognizing that consistency is key to success, we can integrate these treatments into our daily routines.
Let’s take a look at some ways that we can improve our mindset about long-term treatment.
1. Let hair care become part of a daily self-care routine.
Taking care of our hair is important to our overall health and well-being. We all have a daily skincare routine to maintain our skin’s health and appearance, and we can apply the same principles to our hair care routine.
Hair loss treatments should be viewed as a constructive practice that can help preserve and enhance our natural features. Whether we choose to use topical solutions, medications, or nutritional supplements, these treatments can help us maintain the health and vitality of our hair.
By adopting this mindset, we can reframe hair loss treatment as a positive and nurturing practice that empowers us to take control of our hair’s health, just like how we care for our skin, caring for our hair can be a normal and rewarding part of our daily wellness routine.
Another perspective:
2. Starting treatment today does not mean committing to that treatment forever.
Research shows that when someone quits treatment, their hair loss will resume. Within several months, their hair will return to its state before treatment. As you can see above, minoxidil users typically experience a loss of gains within 3-6 months, with an initial excess shedding period and then a return to baseline. For finasteride users, that timeframe is often 6-12 months (or longer), and quitting microneedling can take over 6 months to lose hair gains.
Importantly, those same studies show people are never worse off after starting and then quitting hair loss treatments.
This is critical because it means there is little risk when trying a hair loss treatment and later withdrawing it. By doing so, hair loss is not accelerated; it simply returns to baseline after quitting. In effect, the time spent on the treatment has slowed the progress of future hair loss.
It’s significantly easier to arrest the progression of hair loss than to regrow hair. That means that when fighting hair loss, time is of the essence. We speak about this in our treatment mistakes video series, which is available for members, particularly in the videos about balding speeds.
As such, trying a treatment today does not require a lifelong commitment to that treatment. Just by giving that treatment a shot, the rate of hair loss potentially slows down. If a decision is made later to quit or taper away from that treatment, the data strongly suggest that your efforts should never make things worse in the long-run.
Do Any Hair Loss Treatments Work Permanently, Even After Quitting Them?
For some cases of telogen effluvium and alopecia areata, yes. There may be conditional situations where this might be true for scarring alopecias.
For cases of androgenic alopecia, the clinical data suggests hair loss treatments need to be lifelong. Some studies have indicated that adding microneedling to minoxidil might enhance the staying power of minoxidil’s hair gains by several months, even 6+ months after quitting both interventions.
We talk about these phenomena in this video. Remember that the data are preliminary, so don’t quit any treatments because of that study.
So, why not take action now and begin a regrowth protocol to put yourself in the best possible future position? Any progress made will, at the very least, slow down the progression of hair loss over time, providing benefits even without a lifelong commitment to treatment.
References[+]
References ↑1 Price, V.H., Menefee, E., Strauss, P.C., (1999). Changes in hair weight and hair count in men with androgenetic alopecia after application of 5% and 2% topical minoxidil, placebo, or no treatment. Journal of American Academy of Dermatology. 41(5.1). 717-721. Available at: https://doi.org/10.1016/s0190-9622(99)70006-x ↑2, ↑3 Kaufman, K.D., Olsen, E.A., Whiting, D., Savin, R., DeVillez, R., Bergfeld, W., Price, V.H., van Neste, D., Roberts, J.L., Hordinsky, M., Shapiro, J., Binkowitz, B., Gormley, G.J. (1998). Finasteride in the treatment of men with androgenetic alopecia. Journal of the American Academy of Dermatology. 39(4.1). 578-589. Available at: https://doi.org/10.1016/S0190-9622(98)70007-6 ↑4 Clark, R.V., Hermann, D.J., Cunningham, G.R., Wilson, T.H., Morrill, B.B., Hobbs, S. (2004). Marked Suppression of Dihydrotestosterone in Men with Benign Prostatic Hyperplasia by Dutasteride, a Dual 5alpha-Reductase Inhibitor. The Journal of Clinical Endocrinology & Metabolism. 89(5). 2179-2184. Available at: https://doi.org/10.1210/jc.2003-030330 ↑5 Kim, K.H., Park, S.M., Lee, Y.J., Sim, W.Y., Lew, B.L. (2020). Similar efficacy of maintenance treatment of finasteride 1 mg every other month compared with finasteride 1 mg daily in Korean men with androgenetic alopecia after taking finasteride 1 mg daily for 1 year. Journal of the American Academy of Dermatology. 83(6). Available at: https://doi.org/10.1016/j.jaad.2020.06.828 ↑6 Bao, L., Zong, H., Fang, S., Zheng, L.i, Y. (2022). Randomized trial of electrodynamic microneedling combined with 5% minoxidil topical solution for treating androgenetic alopecia in Chinese males and molecular mechanistic study of the involvement of the Wnt/β-catenin signaling pathway. Journal of Dermatological Treatment. 33(1). 483-493. Available at: https://doi.org/10.1080/09546634.2020.1770162 ↑7 Bao, L., Zong, H., Fang, S., Zheng, L.i, Y. (2022). Randomized trial of electrodynamic microneedling combined with 5% minoxidil topical solution for treating androgenetic alopecia in Chinese males and molecular mechanistic study of the involvement of the Wnt/B-catenin signaling pathway. Journal of Dermatological Treatment. 33(1). 483-493. Available at: https://doi.org/10.1080/09546634.2020.1770162 When it comes to microneedling vs. platelet-rich plasma, which is better? Dermatologists often recommend platelet-rich plasma therapy (PRP) as a treatment for hair loss. This autologous therapy evokes the body’s natural healing response, as does microneedling. We look at what the research studies say about the effectiveness of these two treatments. Time and cost factors are also important considerations for most people.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is Microneedling?
Microneedling, a minimally invasive cosmetic procedure, has emerged as a promising treatment for various forms of hair loss, including androgenic alopecia (AGA). This technique involves using specialized devices, like rollers of pens, equipped with fine needles to create controlled micro-injuries on the scalp.
A derma roller for at-home microneedling.
These micro-injuries stimulate the body’s natural wound-healing processes, enhancing blood flow and promoting the release of growth factors essential for hair regeneration. This method not only improves hair density and thickness but also increases the efficacy of topical hair growth products by facilitating deeper penetration into the scalp.[1]Dhurat, R., Sukesh, M.S., Avhad, G., Dandale, A., Pal, A., Pund, P. (2013). A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study. International … Continue reading,[2]English, R.S., Ruiz, S., DoAmaral, P. (2021). Microneedling and Its Use in Hair Loss Disorders: A Systematic Review. Dermatology and Therapy. 12. 41-60. Available at: … Continue reading
What is Platelet-Rich Plasma Therapy?
Platelet-rich plasma (PRP) therapy is increasingly recognized as an effective treatment for hair loss, particularly AGA. This procedure involves drawing a patient’s blood, processing it to concentrate platelets and growth factors, and injecting this enriched plasma into the scalp.
PRP therapy stimulates hair follicles, promotes new hair growth, and enhances hair density and thickness. The growth factors and proteins in PRP promote tissue repair and regeneration, making it a promising non-surgical option for hair loss. Clinical studies have also demonstrated the efficacy of PRP in improving hair count and thickness in individuals with hair loss.[3]Gentile, P., Garcovich, S., Bielli, A., Scioli, M.G., Orlandi, A., Cervelli, V. (2015). The Effect of Platelet-Rich Plasma in Hair Regrowth: A Randomized Placebo-Controlled Trial. Stem Cells … Continue reading,[4]Cervantes, J., Perper, M., Wong, L.L., Eber, A. E., Fricke, A.C.V., Wikramanayake, T.C., Jiminez, J.J. (2018). Effectiveness of Platelet-Rich Plasma for Androgenetic Alopecia: A Review of the … Continue reading
Microneedling vs. PRP: Which Is Better?
When hair loss patients visit dermatologists for advice, it’s not uncommon for those physicians to recommend autologous therapies. These hair loss therapies, such as platelet-rich plasma (PRP) therapy, PRP + Acell, adipose-derived stem cells, exosomes, and others, are derived from our tissues. These treatments must be conducted in a clinical setting and administered by a healthcare professional. While there is scientific evidence behind these therapies, it is also a significant cash cow for dermatologists, so it is no surprise that they recommend this treatment.
What these dermatologists won’t tell patients is that there is an alternative to PRP that:
- Can be administered at home
- Leverages the exact same mechanisms of action as PRP
- Costs just a fraction of the price (usually 0.1% of the cost of a single PRP session)
- Might be just as effective as PRP
That alternative is microneedling.
What Does the Clinical Evidence Say?
Two randomized, blinded, controlled clinical trials indicate that microneedling produces the same hair parameter improvements as PRP. Let’s take a closer look at these studies and determine if PRP has any benefits over microneedling.
Study 1 – Split Scalp Study Comparing Microneedling Alone to Microneedling with PRP
This one-year-long study included 30 male patients with varying degrees of androgenic alopecia. Each participant received treatments on different halves of their scalp – one half received microneedling only, and the other half of the scalp received microneedling and PRP together. The treatments were conducted over four months, with a follow-up evaluation three months after the final session. The effectiveness was measured using dermoscopic microphotographs and patient satisfaction scores.[5]Aggarwal K, Gupta S, Jangra RS, Mahendra A, Yadav A, Sharma A. Dermoscopic Assessment of Microneedling Alone versus Microneedling with Platelet-Rich Plasma in Cases of Male Pattern Alopecia: A … Continue reading
The Results
- Hair Thickness and Density: Both treatments significantly improved hair thickness and density. The microneedling-only group nearly doubled the increase in hair thickness compared to the microneedling and PRP groups, though the difference between the groups was not statistically significant (Figure 1).
- Patient Satisfaction: Most patients reported moderate satisfaction with the treatment outcomes, noting reduced hair loss but not necessarily new hair growth.
- Long-Term Effects: A follow-up revealed that some patients experienced a recurrence of hair loss, indicating the need for ongoing or maintenance treatments.
Figure 1: Average hair density before and after treatment for microneedling and microneedling + PRP treated groups. While there were significant improvements in both groups compared to before treatment, there was no significant difference between the two groups.[6]Aggarwal K, Gupta S, Jangra RS, Mahendra A, Yadav A, Sharma A. Dermoscopic Assessment of Microneedling Alone versus Microneedling with Platelet-Rich Plasma in Cases of Male Pattern Alopecia: A … Continue reading
The Conclusion
Both microneedling and PRP can effectively treat androgenic alopecia and improve hair parameters and patient satisfaction. However, adding PRP to microneedling did not show any significant additional benefits over microneedling alone.
Study 2 – PRP Compared to Saline Injection
Another study was conducted with 26 women with female pattern hair loss. The women were randomly assigned to receive either 10 mL of PRP or a normal saline placebo. The study’s primary endpoints were hair count and hair mass index (HMI), measured at baseline and after 26 weeks. Additionally, a patient survey was conducted to gauge personal perceptions of treatment effectiveness.[7]Puig CJ, Reese R, Peters M. Double-Blind, Placebo-Controlled Pilot Study on the Use of Platelet-Rich Plasma in Women With Female Androgenetic Alopecia. Dermatol Surg. 2016 Nov;42(11):1243-1247. Doi: … Continue reading
The Results
- Hair Count and Mass: There was no statistically significant difference between the PRP and placebo groups regarding hair count and HMI after 26 weeks. This suggests that the needle insertion and the subsequent acute inflammation may be the reason for the improvement in hair growth, rather than the injection and the PRP (spoiler alert, you can get the same effect from just microneedling).
- Patient Survey: A small percentage (13.3%) of the treatment group reported substantial improvement in aspects like hair loss rate, hair thickness, and ease of hair management compared to the placebo group. However, these subjective improvements did not align with the objective measurements of hair count and HMI.
The Conclusion
This study, despite being well-designed, did not demonstrate a significant advantage of PRP over placebo in treating female androgenetic alopecia. The findings suggest that further research is needed to fully understand the role of PRP in hair loss treatment, including the possible contribution of the injection process beyond the growth factors in PRP.
So, it’s not looking great for PRP compared to microneedling. But are there any other redeeming qualities?
What About the Cost?
We know that PRP can improve hair loss outcomes, but it does not appear to be any more effective than microneedling. So does the cost make it more appealing?
No.
PRP is several times more expensive than microneedling. Let’s break it down a bit.
Microneedling Cost-Benefit
Let’s start with the costs:
- Initial investment: A microneedling device (roller or pen) can range from $10 – $200 for at-home devices.
- Replacement costs: Needles or cartridges, if applicable.
- Maintenance: Limited to cleaning and sterilizing the device.
Now, let’s see the benefits:
- Effectiveness: Proven to improve hair thickness and density in several studies.
- Convenience: This can be done at home.
- One-time cost: Mostly just the initial investment; very low ongoing costs.
Platelet-Rich Plasma Cost-Benefit
Costs:
- Per Session Cost: Each PRP session can range from $400 – $1300, depending on material quality and where you go.
- Annual cost: $1500 – $10,000 (assuming 3-4 sessions)
- Frequency: Initially, multiple sessions are needed, often 3-4 per year
- Maintenance: Every 6 – 12 months after the initial treatment to maintain hair regrowth.
Benefits:
- Effectiveness: Clinical studies show that it can stimulate hair growth and increase hair density (though microneedling can produce the same results).
- Professional Supervision: Performed by medical professionals, offering expertise and safety.
Based on the above information, it’s safe to say that you get more for your money with microneedling, given its effectiveness and significantly lower costs.
What About the Convenience / Ease of Use?
Several key differences become apparent when comparing the convenience and ease of use between microneedling and PRP.
Microneedling
Microneedling is notably convenient, especially with at-home devices. It allows individuals to perform the treatment at their own pace and in the comfort of their own homes, eliminating the need for frequent clinic visits. Furthermore, these devices are relatively straightforward to use. After an initial learning curve, users can quickly integrate the treatment into their routine. These sessions can also be relatively quick, often taking less than 10 minutes, and can be easily scheduled around personal routines and commitments.
If you want to learn more about integrating microneedling into your routine, look at our Ultimate Guide here.
Platelet-Rich Plasma
PRP therapy, on the other hand, is less convenient compared to microneedling due to the necessity of visiting a clinic or a healthcare provider for each session. This requires scheduling appointments, possibly taking time off work, and traveling to the clinic.
It is also not a self-administered treatment. It requires a skilled medical professional to draw the blood, process it to concentrate the platelets and inject it into the scalp. The process is more complex and clinical compared to miconeedling. Moreover, each PRP session, including preparation and treatment, takes longer than a typical microneedling session (treatment alone can take ~1 hour!), and the need to schedule and attend clinic appointments adds to the time commitment.
Overview Comparing Microneedling and PRP Therapy
Take a look at this overview table that we’ve created to get a quick comparison between the two treatments.
Criteria Microneedling PRP Therapy Effectiveness Similar improvements in hair count and thickness in comparative studies. Cost per Session Relatively low; cost primarily involves the purchasing of a microneedling device. This can range from less than $10 for a derma roller to ~$80+ for a derma pen.
If you want an aesthetician to do it for you, it can cost $50 – $150 per session.Higher. It involves the cost of blood draws, processing, and injections per session. The cost of just one injection can range anywhere from $400 – $1300, depending on the materials’ quality and where you go for treatment. Total Cost for Treatment There is a one-time cost for the device, which can be reused multiple times. Treatments (3-4 rounds) could cost $1500 – $10,000. Session Frequency It can vary; typically, once a week to once every few weeks. Every 4-6 weeks for the first 3-4 months, then maintenance treatments every 6- 12 months. Ease-of-Use/Convenience You can perform it at home but must learn the proper technique. A healthcare professional must perform it in a clinical setting. Recovery Time/Side Effects Minimal; may include temporary redness or irritation. Minimal; may include scalp tenderness, swelling, or mild pain at the injection sites. Longevity of Results Long-term consistent use is required for sustained results – however, some benefits may be retained even after the stoppage of treatment. Periodic maintenance sessions are needed for sustained results. In addition to saving time and money (which can amount to tens of thousands of dollars), it’s important to be cautious when following a dermatologist’s recommendation for PRP or any other autologous hair growth therapy. Instead, when weighing the options between microneedling and PRP, it may be wise to consider the benefits of microneedling.
References[+]
References ↑1 Dhurat, R., Sukesh, M.S., Avhad, G., Dandale, A., Pal, A., Pund, P. (2013). A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study. International Journal of Trichology. 5(1). 6-11. Available at: https://doi.org/10.4103/0974-7753.114700 ↑2 English, R.S., Ruiz, S., DoAmaral, P. (2021). Microneedling and Its Use in Hair Loss Disorders: A Systematic Review. Dermatology and Therapy. 12. 41-60. Available at: https://doi.org/10.1007/s13555-021-00653-2 ↑3 Gentile, P., Garcovich, S., Bielli, A., Scioli, M.G., Orlandi, A., Cervelli, V. (2015). The Effect of Platelet-Rich Plasma in Hair Regrowth: A Randomized Placebo-Controlled Trial. Stem Cells Translational Medicine. 4(11). 131-1323. Available at: https://doi.org/10.5966/sctm.2015-0107 ↑4 Cervantes, J., Perper, M., Wong, L.L., Eber, A. E., Fricke, A.C.V., Wikramanayake, T.C., Jiminez, J.J. (2018). Effectiveness of Platelet-Rich Plasma for Androgenetic Alopecia: A Review of the Literature. Skin Appendage Disorders. 4. 1-11. Available at: https://doi.org/10.1159/000477671 ↑5, ↑6 Aggarwal K, Gupta S, Jangra RS, Mahendra A, Yadav A, Sharma A. Dermoscopic Assessment of Microneedling Alone versus Microneedling with Platelet-Rich Plasma in Cases of Male Pattern Alopecia: A Split-Head Comparative Study. Int J Trichology. 2020 Jul-Aug;12(4):156-163. doi: 10.4103/ijt.ijt_64_20. Epub 2020 Sep 19. PMID: 33376284; PMCID: PMC7759059. ↑7 Puig CJ, Reese R, Peters M. Double-Blind, Placebo-Controlled Pilot Study on the Use of Platelet-Rich Plasma in Women With Female Androgenetic Alopecia. Dermatol Surg. 2016 Nov;42(11):1243-1247. Doi: 10.1097/DSS.0000000000000883 Whether microneedling is done by a dermatologist or at home, how deep do the punctures need to be for the best results? Is bleeding when microneedling necessary, or is it a sign that it’s being done incorrectly? This guide explores how needle depth affects the efficacy of microneedling and whether bleeding needs to be involved in achieving the best results.
What is Microneedling?
Microneedling, a minimally invasive cosmetic procedure, has gained recognition for its potential to enhance outcomes in individuals with androgenic alopecia (AGA). This approach involves specialized devices equipped with fine, tiny needles that create controlled micro-injuries on the scalp’s surface. While intentionally inducing micro-injuries may seem counterintuitive, it triggers the body’s natural wound-healing response, fostering numerous processes that benefit individuals with AGA.
Microneedling can be conducted either in a clinical setting or at home. Various devices are available for this purpose, including needling stamps, manual rollers, and automated pens. Some of these devices may incorporate fractional radiofrequency technology. Regardless of the specific device used and the needling depth, microneedling has proven effective in clinical settings as both a primary treatment and a complementary therapy.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Evidence Supports the Use of Microneedling?
Clinical studies have demonstrated that microneedling can increase hair density, thickness, and count in individuals with AGA. A landmark study was conducted by Rachita Dhurat in 2013 on 100 subjects with AGA, using a 1.5 mm derma roller. The researchers found that over 12 weeks, once weekly microneedling combined with twice daily 5% minoxidil significantly increased hair counts compared to minoxidil treatment alone (Figure 1).[1]Dhurat, R., Sukesh, M.S., Avhad, G., Dandale, A., Pal, A., Pund, P. (2013). A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study. International … Continue reading
Figure 1: Microneedling plus 5% minoxidil for AGA: results over three months (weekly sessions).[2]Dhurat R., Sukesh, M.S., Avhad, G., Dandale, A., Pal, A., Pund, P. (2013). A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study. International … Continue reading
Further research has continued to investigate the mechanism of action of microneedling on hair growth, as well as its effects on hair regrowth.
We have covered many of these studies (and more) in our systematic review on the subject (which was published in Dermatology and Therapy in 2021).[3]English Jr, R.S., Ruiz, S., DoAmarel, P. (2022). Microneedling and its use in hair loss disorders: A systematic review. Dermatology and Therapy. 12. 41-60. Available at: … Continue reading
How Does Microneedling Improve Hair Growth?
Microneedling is not just a superficial treatment; it has the ability to enhance hair growth by stimulating biological responses within the skin’s layers. This process involves the stimulation of the scalp at different depths, which activates a cascade of healing and rejuvenating mechanisms that are crucial for promoting healthier and thicker hair. Microneedling may contribute to hair regrowth by enhancing the effectiveness of topical treatments and stimulating the body’s natural healing processes. Let’s explore in more detail how microneedling can help with hair regrowth.
Enhances Drug Penetration
At shorter needle lengths (0.25 mm to 5 mm), microneedling can enhance the absorption and penetration of topical hair growth products such as minoxidil. By creating microchannels in the scalp, microneedling facilitates the delivery of these products to hair follicles, potentially maximizing their effectiveness. However, these needle lengths likely won’t evoke the growth factors necessary to encourage hair follicle proliferation.
Induces Growth Factor and Protein Secretion
At longer needle depths (1.5 mm to 2.5 mm), microneedling punctures the vascular networks in the dermis, which induces the release of growth factors and proteins. The body perceives these micro-injuries as wounds and activates an acute inflammatory response. Inflammation is a natural defense mechanism that recruits various cells and molecules to the injured site.
As part of this inflammatory wound-healing process, platelets in the blood release growth factors such as platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and fibroblast growth factor (FGF). These growth factors are crucial in signaling nearby cells, including fibroblasts and keratinocytes. They stimulate these cells to migrate to the wounded area and begin tissue repair.
Fibroblasts in the scalp’s dermal layer (more on this below) respond to these growth factors by producing collagen and other proteins. Collagen is essential for the structural support of tissues, and it contributes to the overall health and strength of hair follicles.
Stimulates Bulge Stem Cells
Another aspect of the wound healing response is the activation of bulge stem cells. The bulge is a region located in the outer root sheath of the hair follicle, just below the sebaceous gland (Figure 2). It’s recognized as a niche for adult stem cells, essential for the regeneration and growth of hair follicles. These bulge stem cells can give rise to the various cell types that form the hair shaft and its surrounding structures. Activation of these cells is important for hair cycle progression and repair after injury.
Figure 2: Hair follicle structure and location of the bulge.[4]Pantaleyev, A.A., Jahoda, C.A.B., Christiano, A.M. (2001). Hair follicle predetermination. Journal of Cell Science. 114. 3419-3431. Available at: https://doi.org/10.1242/jcs.114.19.3419
(May) Promote Angiogenesis
Another suspected mechanism of microneedling is tissue remodeling, particularly in the form of angiogenesis: the formation of new blood vessel networks. The micro-injuries sustained during microneedling might stimulate increased blood circulation to the treated area, along with growth factors which, over a number of repeated sessions, might help grow new blood vessels in the microvascular networks supporting thinning hair follicles.. This increase in blood flow might deliver more essential nutrients and oxygen to hair follicles, which might improve their growth.
Note: microneedling-induced angiogenesis has been demonstrated in mouse models. However, it has not (yet) been demonstrated in human scalps – because the studies haven’t yet been conducted.[5]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5064188/ It’s suspected that repeated microneedling would also promote angiogenesis in human scalps. However, confirming this would require invasive and repeated biopsies from humans pre- and post-microneedling, which acts as a deterrent for human study. As more research is published, we’ll update this article.
(May) Reduce Scalp Fibrosis
Another suspected effect from microneedling is the potential reduction of scalp fibrosis or scarring, a common feature in individuals with AGA. Scalp fibrosis can hinder hair follicle function and might even drive aspects of hair follicle miniaturization. Microneedling has shown promise in breaking down scar tissue (for example, in acne patients). It’s not unreasonable to assume a similar histological effect might also occur in the scalp, and potentially promote a healthier scalp environment for hair growth. As is the case with angiogenesis, as research develops, we’ll update this article.
How is Microneedling Applied?
Microneedling is generally done with hundreds of tiny, medical-grade needles ranging from 0.1mm to 5.0mm, determining how far into the skin the needles penetrate.
A derma roller for at-home microneedling.
The skin comprises three main layers: the epidermis, dermis, and hypodermis (Figure 3).
Figure 3: The layers of the skin.[6]Yousef, H., Alhajj, M., Sharma, S. (2022). Anatomy, Skin (Integument), Epidermis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Available from: … Continue reading
Epidermis
The epidermis is the outermost layer of skin, and its thickness can vary from 0.04-0.4 mm in different body areas to serve various functions.[7]Skandalakis, L.J. (2009). Skin, Scalp, and Nail. In: Surgical Anatomy and Technique. Springer, New York, NY. Available at: https://doi.org/10.1007/978-0-387-09515-8_1 On the scalp, the epidermis plays a role in protecting the underlying tissues and structures, including the hair follicles; however, it is usually avascular (meaning that it doesn’t have any blood vessels running through it). The epidermis gets its nutrients and disposes of waste products via diffusion from/to the underlying dermis.[8]Kim, J.Y., Dao, H. (2023). Physiology, Integument. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK554386/ (Accessed: 6 … Continue reading
Dermis
The dermis is the layer of skin located just beneath the epidermis on the scalp. It plays a crucial role in supporting hair growth and overall scalp health.
The primary functions of the scalp dermis include:
- housing hair follicles
- providing nourishment to the hair bulb through blood vessels
- anchoring hair follicles to the underlying structures
The scalp dermis is also responsible for regulating temperature and protecting the hair follicles. In terms of thickness, the dermis is the thickest and can range from 1.5 – 4 mm deep.[9]National Cancer Institute (no date). Layers of the Skin. National Cancer Institute. Available at: https://training.seer.cancer.gov/melanoma/anatomy/layers.html (Accessed: 6 November 2023)
Hypodermis
The scalp hypodermis, or subcutaneous layer, is the deepest layer of the scalp skin. Its role is primarily related to insulation, energy storage, and providing cushioning and protection for the underlying structures, such as the skull and blood vessels. The hypodermis is rich in fat cells, blood vessels, and connective tissue. This layer helps regulate temperature, acts as an insulator, and stores fat as an energy reserve. The thickness of the scalp hypodermis can vary from person to person, but it’s typically a few millimeters deep. Maintaining a healthy scalp hypodermis is crucial for overall scalp function and protection.
Do I Need to Bleed for Microneedling To Work?
The short answer is no; bleeding is not a requirement for effective microneedling. However, pinpoint bleeding from microneedling is not necessarily detrimental, and it can just be wiped away.
Excessive bleeding, however, can be an indication that the needles are penetrating too deeply, which may increase the risk of side effects and is not necessary for the therapeutic benefits of the procedure. Emissary veins are vessels that connect the hypodermis of the scalp to the brain through the skull, functioning in both directions.[10]Klein, B.M., Bordoni, B. (2023). Anatomy, Head and Neck, Emissary Veins. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: … Continue reading Infections in the brain stemming from scalp injuries often result from these veins being compromised, allowing bacteria from the skin to enter the brain, potentially leading to severe consequences or even death.
These veins are not uniformly distributed across the scalp and are typically found deeper than 5 mm, near the lower regions of the hypodermis. There’s no need to risk damaging these veins with microneedling since activating the hair follicle’s stem cell bulge is possible at shallower depths, specifically between 1.5 mm and 2.5 mm.
The existing research on microneedling for hair loss does not involve needles longer than 2.5 mm, so it is advisable to stick within these clinically supported depths and avoid going deeper.
Microneedling: What Depth Of Punctures Will Cause Bleeding?
As mentioned above, our skin is segmented by three primary layers: the epidermis, dermis, and hypodermis. The epidermis is the outermost layer of skin and is relatively avascular (without microcapillary networks). The epidermis of scalp skin is estimated to be 0.4mm deep. So, most wounds at this depth and shallower do not bleed. However, you may not get the full beneficial effect from microneedling at this depth. It is only after this depth that punctures from microneedling might evoke erythema, swelling, or pinpoint bleeding.
What’s the Best Needle Depth?
While penetrating the epidermis may be beneficial for increasing drug penetration, it is avascular. Therefore, to produce an appreciable inflammatory response in scalp skin, penetration past the epidermis is necessary. But how far should we go? Well, not much further, according to one study.
Which Needle Length Is Better: 0.6 mm or 1.2 mm?
One study compared two depths of microneedling, 0.6 mm and 1.2 mm, in 60 participants aged 18-45 with mild-to-moderate alopecia. The participants were divided into three groups. One group was treated with only 5% minoxidil lotion, the second group (group A) received minoxidil plus biweekly microneedling at a depth of 1.2 mm and the third group (group B) received minoxidil plus biweekly microneedling at a depth of 0.6 mm over 12 weeks.[11]Faghihi, G., Nabavinejad, S., Mokhtari, F., Naeini, F.F., Iraji, F. (2020). Microneedling in androgenetic alopecia; comparing two different depths of microneedles. Journal of Cosmetic Dermatology. … Continue reading
Results
Both hair count and thickness significantly increased in all groups compared to the baseline, with group B showing a substantially more significant increase in hair count and thickness than the control group (Figure 4). Additionally, hair regrowth evaluated by investigators was significantly higher in both microneedling groups compared to the minoxidil group, with group B (0.6 mm depth) tending to show more benefit than group A (1.2 mm depth). This improvement was not statistically significant, however, and the 1.2 needle improved hair counts by about 15%, and the 0.6 mm needle improved hair counts by about 19%.
Figure 4: The effect of needle depth on mean hair count (white bar) and thickness (black bar).[12]Faghihi, G., Nabavinejad, S., Mokhtari, F., Naeini, F.F., Iraji, F. (2020). Microneedling in androgenetic alopecia; comparing two different depths of microneedles. Journal of Cosmetic Dermatology. … Continue reading
So, we can see that the 0.6 mm needle length was superior at improving hair counts and thickness, but what other benefits might we see from using the shorter needle length?
Other Benefits
Reduced Pain: According to the study, participants in group A (1.2 mm depth) reported more severe pain than the other groups. Therefore, using a shorter needle may reduce the pain associated with microneedling.
Less Trauma to Hair Follicles: It was speculated in the study that the deeper penetration of needles from group A might have caused some trauma to the hair bulge, thus decreasing its efficacy, indicating that shorter needle length may be more beneficial for overall hair follicle health.
Faster Wound Healing: Because the 0.6 mm needle depth does not penetrate as far, it is likely that wound healing will be faster (although this wasn’t examined in this study).
Other Studies
Interestingly, other studies have suggested that using a derma roller with 1.5 mm-sized needles also might improve hair growth for those with androgenic alopecia.[13]Jha, A.K., Udayan, U.K., Roy, P.K., Amar, A.K.J., Chaudhary, R.K.P. (2018). Original article: Platelet-rich plasma with microneedling in androgenetic alopecia along with dermoscopic pre-and … Continue reading,[14]Dhurat, R., Sukesh, M.S., Avhad, G., Dandale, A., Pal, A., Pund, P. (2013). A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study. International … Continue reading
Furthermore, needle penetration studies show that with microneedling automated pens, needling depths matched penetration depths up to 1.5 mm (meaning that the needle will penetrate to the exact depth).[15]Sasaki GH. (2017). Micro-needling depth penetration, presence of pigment particles, and fluorescein stained platelets: clinical usage for aesthetic concerns. Aesthetic Surgery Journal. 37(1):71–83. … Continue reading
However, when it comes to manual rollers, it’s estimated that due to pressure variability and angle of needle entry, microneedling rollers may only penetrate to skin depths of 50-70% of its needle length.[16]de Andrade Lima, E.V., de Andrade Lima, M. (2013). Microneedling experimental study and classification of the resulting injury. Surgical and Cosmetic Dermatology. 5(2). 110-114.
Therefore, to achieve an optimal depth of around 0.6 – 0.8 mm (based on the available clinical data), an automated pen set to 0.6 -0.8 mm or a manual roller set to 1.00 – 1.5 mm (to account for the loss of penetration) may be the most beneficial.[17]English Jr, R.S., Ruiz, S., DoAmarel, P. (2022). Microneedling and its use in hair loss disorders: A systematic review. Dermatology and Therapy. 12. 41-60. Available at: … Continue reading
Does Bleeding From Microneedling Improve Hair Growth Outcomes?
When looking at the methodologies across microneedling studies, we can see that investigation groups used various methods to denote the endpoint of any microneedling session.[18]English Jr, R.S., Ruiz, S., DoAmarel, P. (2022). Microneedling and its use in hair loss disorders: A systematic review. Dermatology and Therapy. 12. 41-60. Available at: … Continue reading Aside from using different microneedling devices and needle lengths, research groups also tended to vary their session endpoints based on:
- A set number of roller passes in any given area.
- Any number of passes horizontally, vertically, and diagonally until mild erythema (pink skin) occurred
- A set time limit (from just a few minutes to 45 minutes)
- The arrival of pinpoint bleeding
Despite the various methodologies across studies, microneedling led to similar ballpark hair parameter improvements. For these reasons, it’s unclear if pushing harder when microneedling or generating more acute inflammation via pinpoint bleeding induces better outcomes.
Based on the data available, there is nothing to suggest that bleeding when microneedling is necessary and worth the additional pain.
What If I’m Combining Microneedling With Topicals?
Microneedling’s mechanisms of action may change depending on the needle penetration depth.
- At shallower depths (0.5mm and lower), microneedling punctures the scalp’s epidermis. This can significantly enhance the efficacy of minoxidil by increasing both (1) dermal absorption of the drug and (2) sulfotransferase activity. Sulfotransferase is the enzyme required to activate minoxidil.
- At deeper depths (0.5mm-2.0mm), microneedling punctures into the dermis and evokes a stronger acute inflammatory reaction. This can induce growth factors, signaling proteins, and hormones linked to the anagen (growth) stage of the hair cycle.
If using microneedling alongside minoxidil, it’s possible to still benefit from microneedling with shorter needle lengths. Shorter needle lengths still produce the benefits of microneedling via enhancement of topical absorption and activation. Shallow microneedling will also minimize the pain associated with a microneedling session and help avoid bleeding.
So, no, it is not a requirement to bleed when microneedling to get the best results. But if bleeding occurs? Just wipe the blood away with an alcohol swab.
References[+]
References ↑1, ↑14 Dhurat, R., Sukesh, M.S., Avhad, G., Dandale, A., Pal, A., Pund, P. (2013). A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study. International Journal of Trichology. (5)1. 6-11. Available at: https://doi.org/10.4103/0974-7753.114700 ↑2 Dhurat R., Sukesh, M.S., Avhad, G., Dandale, A., Pal, A., Pund, P. (2013). A Randomized Evaluator Blinded Study of Effect of Microneedling in Androgenetic Alopecia: A Pilot Study. International Journal of Trichology. 5(1). 6-11. Available at: https://10.4103/0974-7753.114700 ↑3, ↑17, ↑18 English Jr, R.S., Ruiz, S., DoAmarel, P. (2022). Microneedling and its use in hair loss disorders: A systematic review. Dermatology and Therapy. 12. 41-60. Available at: https://doi.org/10.1007/s13555-021-00653-2 ↑4 Pantaleyev, A.A., Jahoda, C.A.B., Christiano, A.M. (2001). Hair follicle predetermination. Journal of Cell Science. 114. 3419-3431. Available at: https://doi.org/10.1242/jcs.114.19.3419 ↑5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5064188/ ↑6 Yousef, H., Alhajj, M., Sharma, S. (2022). Anatomy, Skin (Integument), Epidermis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Available from: https://www.ncbi.nlm.nih.gov/books/NBK470464/ (Accessed: 7 November 2023) ↑7 Skandalakis, L.J. (2009). Skin, Scalp, and Nail. In: Surgical Anatomy and Technique. Springer, New York, NY. Available at: https://doi.org/10.1007/978-0-387-09515-8_1 ↑8 Kim, J.Y., Dao, H. (2023). Physiology, Integument. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK554386/ (Accessed: 6 November 2023) ↑9 National Cancer Institute (no date). Layers of the Skin. National Cancer Institute. Available at: https://training.seer.cancer.gov/melanoma/anatomy/layers.html (Accessed: 6 November 2023) ↑10 Klein, B.M., Bordoni, B. (2023). Anatomy, Head and Neck, Emissary Veins. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK563196/ (Accessed: 7 November 2023) ↑11, ↑12 Faghihi, G., Nabavinejad, S., Mokhtari, F., Naeini, F.F., Iraji, F. (2020). Microneedling in androgenetic alopecia; comparing two different depths of microneedles. Journal of Cosmetic Dermatology. 20. 1241-1247. Available at: https://doi.org/10.1111/jocd.13714 ↑13 Jha, A.K., Udayan, U.K., Roy, P.K., Amar, A.K.J., Chaudhary, R.K.P. (2018). Original article: Platelet-rich plasma with microneedling in androgenetic alopecia along with dermoscopic pre-and post-treatment evaluation. Journal of Cosmetic Dermatology. 17(3). 313-318. Available at: https://doi.org/10.1111/jocd.12394. ↑15 Sasaki GH. (2017). Micro-needling depth penetration, presence of pigment particles, and fluorescein stained platelets: clinical usage for aesthetic concerns. Aesthetic Surgery Journal. 37(1):71–83. Available at: https://doi.org/10.1093/asj/sjw120 ↑16 de Andrade Lima, E.V., de Andrade Lima, M. (2013). Microneedling experimental study and classification of the resulting injury. Surgical and Cosmetic Dermatology. 5(2). 110-114. CB-03-01, also known as Breezula™ or clascoterone, is a topical medication generating interest as a potential therapy for androgenetic alopecia (AGA). It was developed by Cassiopea (now owned by Cosmo Pharmaceuticals) and is a synthetic androgen receptor antagonist. While it is primarily recognized for its potential in combating hair loss, particularly AGA, CB-03-01 has also exhibited efficacy in treating conditions like acne, hirsutism, polycystic ovary syndrome (PCOS), and seborrheic dermatitis. In this overview, we look at whether CB-03-01 can impact hair follicles and its potential in treating hair loss, and we will also look at CB-03-01’s safety profile and mechanism of action, drawing from clinical trials and research findings.
Key Takeaways
- Drug. CB-03-01, also known as Breezula™ or clascoterone, is a topical synthetic androgen receptor antagonist developed by Cassiopea (now owned by Cosmo Pharmaceuticals). It competes with natural androgens like dihydrotestosterone (DHT) for binding to androgen receptors, making it a promising treatment for hair loss that may be caused by androgen signaling, particularly androgenetic alopecia.
- Clinical Data. Three Phase II trials for CB-03-01 have been conducted – two for male and one for female AGA – the results of one of these trials were not published. The published studies are summarized below:
- Study 1: A study involving 293 women aged 18-55 with AGA. Of various treatments used, a 5% formulation of CB-03-01 was the only treatment that significantly improved, and only in women under 30.[1]Cassiopea Spa, (2021). Cassiopea SpA Announces Topline Results of Phase II Proof of Concept Trial of Clascoterone Solution for the Treatment of Androgenetic Alopecia in Females. Bloomberg. Available … Continue reading
- Study 2: A study involving 400 men aged 18-55 with mild to moderate AGA. A 7.5% concentration of CB-03-01 led to statistically significant improvements in hair length and width in the treated area. All treatment groups showed relative improvement compared to the control.[2]Cassiopea Spa, (2021). Cassiopea Announces Very Positive Phase II Twelve Months Results for Breezula® (Clascoterone) in Treating Androgenetic Alopecia Bloomberg. Available at: … Continue reading
- Phase III trials of CB-03-01 are expected to be completed in January 2025.
- Safety. CB-03-01 has reportedly demonstrated minimal side effects, with common issues being mild skin reactions such as scaling, redness, and itching. However, there is too little published data to make a definitive statement regarding the safety of CB-03-01.
- Evidence Quality. CB-03-01 scored 36/100 for evidence quality by our metrics.
- Best Practices. This product is not currently available at a 5% concentration for treatment of AGA. However, when available, this may be most effective when used twice daily by women with AGA under 30, based on the available data.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is CB-03-01?
CB-03-01, known by its brand name Breezula™ or clascoterone, is a topical synthetic androgen receptor antagonist owned by Cosmo Pharmaceuticals.[3]Cosmo, (no date). Breezula. Cosmo Pharmaceuticals Available at: https://www.cosmopharma.com/pipeline/breezula (Accessed: 17 October 2023) An androgen receptor antagonist is a substance that can interfere with or block androgen hormones from working as they normally would.[4]Kokal, M., Mirzakhani, K., Pungsrinont, T., Baniahmad, A. (2020). Mechanisms of Androgen Receptor Agonist- and Antagonist-Mediated Cellular Senescence in Prostate Cancer. Cancers (Basel). 12(7). … Continue reading CB-03-01 is a competitive antagonist, meaning it competes with natural androgen hormones in our bodies, such as dihydrotestosterone (DHT), for binding to the androgen receptor. CB-03-01 is primarily recognized for its potential in treating hair loss, particularly androgenetic alopecia. However, it has also been used to treat acne (under the brand name Winlevi), hirsutism (excess/unwanted facial hair in women), polycystic ovary syndrome (PCOS), and seborrheic dermatitis (Figure 1).
Figure 1: Chemical structure of CB-03-01.[5]Drugbank Online (no date), Clascoterone. Drugbank Online. Available at: https://go.drugbank.com/drugs/DB12499 (Accessed: 16 October 2023)
How Does CB-03-01 Work?
The mechanism of action of CB-03-01 (clascoterone) involves its interaction with androgen receptors in the skin, particularly in hair follicles and sebaceous glands. This compound is a selective androgen receptor antagonist with a specific affinity for androgen receptors.[6]Cosmo, (no date). Breezula. Cosmo Pharmaceuticals Available at: https://www.cosmopharma.com/pipeline/breezula (Accessed: 17 October 2023) Androgens are a group of hormones that include testosterone and dihydrotestosterone (DHT), which play a role in the development and growth of hair, but which can also contribute to conditions like androgenetic alopecia (AGA, also known as male pattern hair loss) and acne when androgen hormone activity becomes abnormal or excessive.[7]Handelsman, D.J. (2020). Androgen Physiology, Pharmacology, Use and Misuse. Endotext [Internet]. South Dartmouth (MA). Available at: https://www.ncbi.nlm.nih.gov/books/NBK279000/ (Accessed: 17 … Continue reading
Androgens like DHT normally activate androgen receptors to mediate their biological effects. CB-03-01 interferes with the ability of androgens to activate these receptors. In the context of hair loss, reducing androgen signaling can help slow down the miniaturization of hair follicles associated with androgenetic alopecia. By reducing the impact of androgens on hair follicles, CB-03-01 may help prevent hair follicle miniaturization and hair loss.
What is the Impact of CB-03-01 on Hair Follicle Biology?
There is one in vitro (or ‘test tube’) study that we could find that looks at how CB-03-01 could affect hair follicle biology. The study looked at dermal papilla cells (DPCs), which can be thought of as the hair follicle’s signaling center and which are negatively affected by testosterone in patients with AGA. DPCs from balding scalps grow slower than those of healthy scalps. They undergo a process called premature senescence, in which cells lose their ability to divide and grow.[8]Bahta, A.W., Farjo, N., Farjo, B., Philpott, M. Premature senescence of balding dermal papilla cells in vitro is associated with p16(INK4a) expression. Journal of Investigative Dermatology. 218(5). … Continue reading
Firstly, the researchers wanted to show that CB-03-01 could, in principle, interfere with androgen receptor signaling. They used an experimental tool called androgen receptor reporter cells, which are commonly used to study the activity of androgen receptors. These cells were treated with 0.4 nM testosterone in the presence or absence of CB-03-01 or finasteride. The IC50 value – the drug concentration required to give half the maximal response – was then calculated. CB-03-01 (called clascoterone here) had an IC50 of 1.55×10-6M, compared to 2.89×10-6 M for finasteride. As a lower IC50 value indicates that a drug is more effective, the results show that clascoterone is at least as potent as finasteride in inhibiting testosterone-induced androgen receptor activity; their IC50 values are in the same order of magnitude (Figure 2).[9]Rosetter, C., Rosette, N., Mazzetti, A., Moro, L., Gerloni, M. Cortexolone 17ɑ-Proprionate (Clascoterone) is an Androgen Receptor Antagonist in Dermal Papilla Cells in Vitro. Journal of Drugs in … Continue reading
Figure 2: CB-03-01 (clascoterone) and finasteride have similar potency as inhibitors of testosterone-induced androgen receptor activity.[10]Rosetter, C., Rosette, N., Mazzetti, A., Moro, L., Gerloni, M. Cortexolone 17ɑ-Proprionate (Clascoterone) is an Androgen Receptor Antagonist in Dermal Papilla Cells in Vitro. Journal of Drugs in … Continue reading
The researchers then treated reporter cells with 200 μM DHT with or without finasteride or CB-03-01 under three conditions (Figure 3).- Treated with DHT plus androgen receptor inhibitor (finasteride of CB-03-01) for 24 hours (to mimic once-daily application)
- Treated with DHT plus androgen receptor inhibitor for 12 hours, then washed off and treated with DHT alone for a further 12 hours (to mimic once daily application and examine the metabolism of the drug)
- Treated with DHT plus androgen receptor inhibitor for 12 hours, then washed off and treated with DHT plus androgen receptor inhibitor for a further 12 hours (to mimic twice-daily application)
In conditions 1 and 3, where CB-03-01 was continuously present, AR activity was significantly inhibited. This suggests that continuous exposure to the inhibitor effectively blocks androgen receptor activity. In condition 2, where CB-03-01 was removed after 12 hours, and the cells were exposed to DHT alone, the inhibitor’s effectiveness significantly decreased. The drug’s IC50 was much higher in this case. This indicates a need for a continuous presence of the inhibitor for sustained antagonism of DHT-induced AR activity. The study also found finasteride was more effective when present for 24 hours than 12 hours (Figure 3), and CB-03-01 seemed to be as effective as finasteride at a similar concentration.
Figure 3: Continuous presence of CB-03-01 (clascoterone) is required for sustained androgen receptor antagonism.[11]Rosetter, C., Rosette, N., Mazzetti, A., Moro, L., Gerloni, M. Cortexolone 17ɑ-Proprionate (Clascoterone) is an Androgen Receptor Antagonist in Dermal Papilla Cells in Vitro. Journal of Drugs in … Continue reading
DPCs were treated with 200 μM DHT or vehicle control (0.1% DMSO) for 24 hours. The researchers found that exposure to high levels of DHT increased the expression of the androgen receptor in healthy dermal papilla cells. This mimicked the conditions found in the balding scalp, where DHT sensitivity contributes to hair loss. Additionally, the experiment revealed that exposure to high levels of DHT significantly increased the secretion of two cytokines: Interleukin-6 (IL-6) and basic fibroblast growth factor (bFGF) by DPCs (Figure 4A & B).
The researchers then investigated whether clascoterone (CB-03-01) could antagonize the synthesis and secretion of these cytokines. They used enzalutamide as a positive control because it also acts as an androgen receptor antagonist, competing with DHT for binding to the androgen receptor. However, it would have been more useful to compare to finasteride, which is commonly used to treat AGA.
Clascoterone was found to be more effective at reducing the secretion of IL-6 compared to enzalutamide. The IC50 (the concentration at which it inhibits 50% of IL-6 secretion) for clascoterone was much lower than that of enzalutamide, indicating that clascoterone more effectively reduced the secretion of this inflammatory cytokine (Figure 4B). However, neither of the drugs had any effect on bFGF (Figure 4C).
The researchers finally performed cell viability assays to ensure the results were not due to cell death – this is important because cell viability changes could affect cytokine secretion. These assays showed that neither clascoterone nor enzalutamide significantly affected cell viability, indicating that the results were not an artifact caused by variations in cell death (Figure 4D).
Figure 4: A: DHT-treated DPCs increased secretion of both IL-6 and bFGF; B, C: CB-03-01 (clascoterone) was effective at reducing IL-6 secretion; however, neither drug was able to inhibit bFGF secretion; D: Cell viability assays showed that the responses were not due to cell death.[12]Rosetter, C., Rosette, N., Mazzetti, A., Moro, L., Gerloni, M. Cortexolone 17ɑ-Proprionate (Clascoterone) is an Androgen Receptor Antagonist in Dermal Papilla Cells in Vitro. Journal of Drugs in … Continue reading
So, we know that CB-03-01 can effectively compete with DHT for the androgen receptor, reducing the harmful effects of the hormone. However, these experiments were conducted in cells in a dish. Let’s move on to studies conducted on human patients.
Is CB-03-01 Clinically Effective at Treating Hair Loss?
CB-03-01 has undergone three Phase II trials, which have informed the dosage for an upcoming Phase III trial that is expected to be completed in 2025. The first Phase II trial was a proof-of-concept study conducted in 2014 with 95 males with androgenetic alopecia. However, the Phase II trial results for male AGA were not publicly disclosed or published.[13]Clinical Trials, (2017). A Phase 2 Study to Evaluate the Safety and Efficacy of CB-03-01 Solution, a Comparator Solution and Vehicle Solution in Males with Androgenetic Alopecia. Clinical Trials. … Continue reading
The second Phase II study was another proof-of-concept study for the use of CB-03-01 in the treatment of female pattern baldness. Once again, there have yet to be fully published results. However, Bloomberg did publish a press release summarizing the main findings.[14]Cassiopea Spa, (2021). Cassiopea SpA Announces Topline Results of Phase II Proof of Concept Trial of Clascoterone Solution for the Treatment of Androgenetic Alopecia in Females. Bloomberg. Available … Continue reading. The trial enrolled 293 women aged 18 to 55, all experiencing androgenetic alopecia (AGA). The participants were divided into groups, with each group containing 70 individuals. The trial’s main objective was to evaluate the effects of different treatments over six months, comparing them to a control group that received a placebo (vehicle) and another group that used a 2% minoxidil solution.
All participants applied their assigned treatment twice daily. The treatment groups included two concentrations of CB-03-01, specifically 5% and 7.5%. The primary outcome measurements were changes in hair count and assessing hair growth over the six months of treatment.
Interestingly, only a subgroup of women under 30 using the 5% CB-03-01 solution showed statistically significant improvements in hair count, which was unexpected. Cassiopea mentioned that they were encouraged by the data and would further analyze it to identify further subgroups. However, since female-pattern hair loss typically occurs later in life for women (in their 50s or 60s), this treatment may not be appropriate for most patients. Therefore, further research is needed to determine its broader applicability.[15]Fabbrocini, G., Cantelli, M., Masara, A., Annunziata, M.C., Marasca, C., Cacciapuoti, S. (2018). Female pattern hair loss: A clinical, pathophysiologic, and therapeutic review. International Journal … Continue reading
Furthermore, although the press release mentioned that some participants were treated with 2% minoxidil, there was no information on how CB-03-01 performed compared to this. This highlights the issue of using press releases instead of peer-reviewed journal articles, as important data can be omitted.
The third phase II study recruited more than 400 male participants in Germany, aged 18-55, with mild to moderate AGA. All participants applied CB-03-01 at concentrations of 2.5%, 5%, 7.5% twice daily, or 7.5% once daily. The control group applied a vehicle solution (once- or twice daily).[16]Cassiopea Spa, (2021). Cassiopea Announces Very Positive Phase II Twelve Months Results for Breezula® (Clascoterone) in Treating Androgenetic Alopecia Bloomberg. Available at: … Continue reading Once again, the results were only available via a press release, so while some data was present we do not know if any has been omitted. It is reported that the results showed statistically significant improvements in target area hair counts and hair growth assessment scores across all active groups compared to the vehicle control. Notably, the highest change occurred in the 7.5% twice-daily group. This group also showed the highest statistically significant improvements in hair width in the treated area.
Two Phase III studies are awaiting recruitment, with expected completion dates in January 2025.[17]Clinical Trials, (no date). CB-03-01. NIH. Available at: https://clinicaltrials.gov/search?cond=Hair%20Loss%2FBaldness&term=CB-03-01 (Accessed: 17 October 2023)
Is CB-03-01 Safe?
According to the Bloomberg press release, treatment-emergent adverse events (TEAEs) were mostly minimal, mild, or trace and unrelated to the study drug. However, very little detail is given. The most frequently observed local skin reactions across all treatment groups were minimal to mild scaling, redness, or minimal itching.[18]Cassiopea Spa, (2021). Cassiopea SpA Announces Topline Results of Phase II Proof of Concept Trial of Clascoterone Solution for the Treatment of Androgenetic Alopecia in Females. Bloomberg. Available … Continue reading
In a Phase III trial of CB-03-01 for patients with facial acne, TEAEs were also generally mild in severity and similar to the control. The most common were pain, dryness, hypersensitivity at the site of application, redness, contact dermatitis, and headache.[19]Hebert, A., Thiboutot, D., Gold, L.S., Cartwright, M., Gerlonim M., Fragasso, E., Mazzetti, A. (2020). Efficacy and Safety of Topical Clascoterone Cream, 1% for Treatment in Patients with Facial … Continue reading
CB-03-01 has yet to receive FDA approval for hair loss treatment, and certainly, more information on its safety and efficacy is required. The results from the upcoming Phase III studies should provide more information.
Can I Make CB-03-01 at Home?
We want to make it clear here – we do not endorse the use of homemade CB-03-01 (or any other treatment) as there may be issues with the purity of CB-03-01 and may lead to other unintended side effects. However, some people are buying powdered CB-03-01 and making a topical solution at home. CB-03-01 powder is widely available online for research and is easy to buy. As for a vehicle, some are using ethanol, propylene glycol (PG), and diethylene glycol monoethyl ether (DEGEE) at a 1:1:1 ratio, whereas others are using ethanol and PG alone.[20]Reddit, (2020). Anyone know how to make your own CB0301 vehicle? Reddit. Available at: https://www.reddit.com/r/tressless/comments/l5y0di/anyone_know_how_to_make_your_own_cb0301_vehicle/ (Accessed: … Continue reading According to Selleckchem, it is soluble in both dimethylsulfoxide (DMSO) and ethanol.[21]Selleckchem, (no date). Clascoterone. Selleckchem. Available at: https://www.selleckchem.com/datasheet/clascoterone-S689601-DataSheet.html (Accessed 17 October 2023)
Is CB-03-01 for Me?
While CB-03-01 is available under the brand name Winlevi for acne at a 1% concentration, it will not be available at the 5% dosage (which seemed effective in Phase II studies) until Phase III studies have been completed and FDA approval application has begun.
However, when it is available, you may want to try this treatment if:
- You are male or female
- You are female and 30 or under
- You have AGA (this treatment targets androgen receptors, so it will not be beneficial for those with other types of hair loss)
References[+]
References ↑1, ↑14, ↑18 Cassiopea Spa, (2021). Cassiopea SpA Announces Topline Results of Phase II Proof of Concept Trial of Clascoterone Solution for the Treatment of Androgenetic Alopecia in Females. Bloomberg. Available at: https://www.bloomberg.com/press-releases/2021-09-10/eqs-adhoc-cassiopea-spa-announces-topline-results-of-phase-ii-proof-of-concept-trial-of-clascoterone-solution-for-the-treatment (Accessed: 17 October 2023) ↑2, ↑16 Cassiopea Spa, (2021). Cassiopea Announces Very Positive Phase II Twelve Months Results for Breezula® (Clascoterone) in Treating Androgenetic Alopecia Bloomberg. Available at: https://www.bloomberg.com/press-releases/2019-04-16/cassiopea-announces-very-positive-phase-ii-twelve-months-results-for-breezula-clascoterone-in-treating-androgenetic (Accessed: 17 October 2023) ↑3, ↑6 Cosmo, (no date). Breezula. Cosmo Pharmaceuticals Available at: https://www.cosmopharma.com/pipeline/breezula (Accessed: 17 October 2023) ↑4 Kokal, M., Mirzakhani, K., Pungsrinont, T., Baniahmad, A. (2020). Mechanisms of Androgen Receptor Agonist- and Antagonist-Mediated Cellular Senescence in Prostate Cancer. Cancers (Basel). 12(7). Available at: https://doi.org/10.3390/cancers12071833 ↑5 Drugbank Online (no date), Clascoterone. Drugbank Online. Available at: https://go.drugbank.com/drugs/DB12499 (Accessed: 16 October 2023) ↑7 Handelsman, D.J. (2020). Androgen Physiology, Pharmacology, Use and Misuse. Endotext [Internet]. South Dartmouth (MA). Available at: https://www.ncbi.nlm.nih.gov/books/NBK279000/ (Accessed: 17 October 2023) ↑8 Bahta, A.W., Farjo, N., Farjo, B., Philpott, M. Premature senescence of balding dermal papilla cells in vitro is associated with p16(INK4a) expression. Journal of Investigative Dermatology. 218(5). 1088-1094. Available at: https://doi.org/10.1038/sj.jid.5701147 ↑9 Rosetter, C., Rosette, N., Mazzetti, A., Moro, L., Gerloni, M. Cortexolone 17ɑ-Proprionate (Clascoterone) is an Androgen Receptor Antagonist in Dermal Papilla Cells in Vitro. Journal of Drugs in Dermatology. 18(2). 197-201 Available at: https://jddonline.com/articles/cortexolone-17a-propionate-clascoterone-is-a-novel-androgen-receptor-antagonist-that-inhibits-produc-S1545961619P0412X/ (Accessed 17 October 2023) ↑10, ↑11, ↑12 Rosetter, C., Rosette, N., Mazzetti, A., Moro, L., Gerloni, M. Cortexolone 17ɑ-Proprionate (Clascoterone) is an Androgen Receptor Antagonist in Dermal Papilla Cells in Vitro. Journal of Drugs in Dermatology. 18(2). 197-201 Available at: https://jddonline.com/articles/cortexolone-17a-propionate-clascoterone-is-a-novel-androgen-receptor-antagonist-that-inhibits-produc-S1545961619P0412X/ (Accessed 17 October 2023) ↑13 Clinical Trials, (2017). A Phase 2 Study to Evaluate the Safety and Efficacy of CB-03-01 Solution, a Comparator Solution and Vehicle Solution in Males with Androgenetic Alopecia. Clinical Trials. Available at: https://clinicaltrials.gov/study/NCT02279823 (Accessed: 17 October 2023) ↑15 Fabbrocini, G., Cantelli, M., Masara, A., Annunziata, M.C., Marasca, C., Cacciapuoti, S. (2018). Female pattern hair loss: A clinical, pathophysiologic, and therapeutic review. International Journal of Womens Dermatology. 4(4). 203-211. Available at: https://doi.org/10.1016/j_ijwd.2018.05.001 ↑17 Clinical Trials, (no date). CB-03-01. NIH. Available at: https://clinicaltrials.gov/search?cond=Hair%20Loss%2FBaldness&term=CB-03-01 (Accessed: 17 October 2023) ↑19 Hebert, A., Thiboutot, D., Gold, L.S., Cartwright, M., Gerlonim M., Fragasso, E., Mazzetti, A. (2020). Efficacy and Safety of Topical Clascoterone Cream, 1% for Treatment in Patients with Facial Acne. Two Phase 3 Randomized Clinical Trials. JAMA Dermatol. 156(6). 1-10. Available at: https://doi.org/10.1001/jamadermatol.2020.0465 ↑20 Reddit, (2020). Anyone know how to make your own CB0301 vehicle? Reddit. Available at: https://www.reddit.com/r/tressless/comments/l5y0di/anyone_know_how_to_make_your_own_cb0301_vehicle/ (Accessed: 17 October 2023) ↑21 Selleckchem, (no date). Clascoterone. Selleckchem. Available at: https://www.selleckchem.com/datasheet/clascoterone-S689601-DataSheet.html (Accessed 17 October 2023) Corticosteroids are a class of steroid hormones that have emerged as a treatment against, in particular, alopecia areata and scarring alopecia. These compounds, synthesized to mimic the activity of cortisol, a hormone produced by the adrenal glands, exhibit potent anti-inflammatory and immunosuppressive properties. This makes them effective in treating hair loss conditions where inflammation or an autoimmune response plays a critical role.
However, long-term corticosteroid use is not without potential drawbacks. When overused (or used for too long), topical corticosteroids are causally linked to hormonal changes, alterations to skin pigmentation, the creation of spider veins, and even skin thinning. Some adverse effects can be permanent – with the risk of irreversibility increasing alongside the dose and duration of use. Without usage breaks and/or careful dosing guidelines, long-term users of topical corticosteroids can inadvertently disfigure their skin.
In the last two years, we’ve observed a concerning trend in the hair loss industry: big-brand telehealth companies now add low-dose corticosteroids – i.e., 1% hydrocortisone and 0.01% fluocinolone – to their prescription hair growth topicals. They’re also recommending patients apply corticosteroids to their scalps up to twice daily, forever.
These corticosteroids undoubtedly help lower scalp inflammation and may offset skin irritation from ingredients like tretinoin (retinoic acid) – which is often paired with hair growth drugs, such as minoxidil, to enhance drug activation and penetration.But is there any evidence that twice-daily use of topical corticosteroids – applied daily, forever, and with no pulse dosing or dosing breaks – is safe? Or are these telehealth companies exposing their patients to unknown risks, gambling with their health, and selling them into short-term hair gains without considering the long-term consequences?
This article will delve into the efficacy and long-term safety of corticosteroids – particularly as a therapy for hair loss disorders. We’ll explore corticosteroids and their therapeutic role in treating hair loss. We’ll also explore considerations for dosing and duration. This is particularly important for people who might be currently using topical corticosteroids on their scalps and who don’t understand the risks they might be exposing themselves to 5-10 years into the future.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What Role Do Corticosteroids Play in Treating Alopecia?
In the context of alopecia, corticosteroids reduce inflammation and suppress the immune system’s activity around hair follicles. This action can halt the progression of hair loss and, in many cases, stimulate hair regrowth. The application of corticosteroids in hair loss treatment can vary; they can be administered topically, injected directly into the scalp, or taken orally.
Within the class of corticosteroids are:
Glucocorticoids: such as cortisol and cortisone, influence carbohydrate, fat, and protein metabolism.[1]Macfarlane, D.P., Forbes, S., Walker, B.R. (2008). Glucocorticoids and fatty acid metabolism in humans: fuelling fat redistribution in the metabolic syndrome. Journal of Endocrinology. 197(2), … Continue reading They are anti-inflammatory, immunosuppressive, and vasoconstrictive (narrow blood vessels). Their anti-inflammatory effects occur through inhibiting inflammatory mediators and stimulating anti-inflammatory mediators. Their immunosuppressive effects occur through direct action on immune cells.[2]Coutinho, A.E., Chapman, K.E. (2011). The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments, and mechanistic insights. Molecular and Cellular Endocrinology. … Continue reading
Mineralocorticoids: such as aldosterone, regulate electrolyte and water balance. They modulate ion transport in the renal tubules of the kidneys.[3]Yang, J., Young, M.J. (2009). The mineralocorticoid receptor and its coregulators. Journal of Molecular Endocrinology. 43(2), 53-64. Available at: https://doi.org/10.1677/JME-09-0031
How is the Potency of a Corticosteroid Decided?
There are seven potency classifications for corticosteroids, which range from Class I – super potent corticosteroids to Class VII – least potent corticosteroids.[4]Gabros, S., Nessel, T.A., Zito, P.M. (2023) Topical Corticosteroids. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: … Continue reading This is based on several factors, including its chemical structure, formulation, and the ability of the drug to cause vasoconstriction in the skin, which is often assessed through vasoconstrictor assays.[5]Stoughton, R.B. (1992). The vasoconstrictor assay in bioequivalence testing: practical concerns and recent developments. International Journal of Dermatology. Available at: … Continue reading These assays measure the degree of skin blanching (induction of longer-than-normal skin paleness) induced by the corticosteroid.
What are the Benefits of Corticosteroids in Treating Alopecia?
Corticosteroids are particularly beneficial in treating alopecia areata and scarring alopecias because they modulate inflammatory and immune response pathways. High potency, medium potency, and low potency have all shown some efficacy in treating alopecia, with the highest efficacy observed with high-potency corticosteroids under occlusion.[6]Alsantali, A. (2011). Alopecia areata: a new treatment plan. Clinical Cosmetic and Investigational Dermatology. 4, 107-115. Available at: https://doi.org/10.2147/CCID.S22767
However, it should be noted that their maximum usage durations depend on the potency of the corticosteroid. Super potent corticosteroids have a maximum duration of 3 weeks, high and medium potency have a maximum duration of 12 weeks, and low potency have no specified limit.[7]Stacey, S.K., Mceleney, M. (2021). Topical Corticosteroids: Choice and Application. American Family Physician. 103(6). 337-343. Available at: … Continue reading Continuing to use corticosteroids after these time points may increase the risk of experiencing adverse effects.
What Risks Are Associated with Corticosteroid Use?
Topical corticosteroids can lead to both skin-related (cutaneous) and whole-body (systemic) side effects, with risk increasing with a larger area of application and higher potency of the drug.[8]Stacey, S.K., Mceleney, M. (2021). Topical Corticosteroids: Choice and Application. American Family Physician. 103(6). 337-343. Available at: … Continue reading
Some common skin-related effects can include:
- Skin thinning
- Stretch marks
- Spider veins
- Easy bruising and purpura
- Delayed wound healing
- Hyper or hypopigmentation
- Acne and rosacea like eruptions
- Hypertrichosis (increased hair growth)
- Infections or aggravation of existing infections
Long-term use may lead to whole-body (systemic) effects. These can include:
- Hypothalamus-pituitary-adrenal activity suppression (characterized by weakened immunity, anxiety, midday fatigue, difficulty sleeping, depression, and aching joints, amongst others)
- Cushingoid appearance (moon face, acne, and thin, easily bruised skin, amongst others)
- Unwanted facial skin hair in women (hirsutism)
- Impotence
- Menstrual irregularities
- Peptic ulcer disease
- Cataracts
- Increased intraocular pressure/glaucoma
- Myopathy
- Osteoporosis
- Vertebral compression fractures
Some patients may also experience a rebound phenomenon – although this is rare in low-potency corticosteroids.
One case study shows a patient who experienced worsening rebound after being treated with first 0.5%, then 1% of hydrocortisone, and again after a 5-day course of clobetasol butyrate and then hydrocortisone.[9]MEDSAFE, (2013). Steroid Rebound – A Topical Issue. MEDSAFE. Available at: https://www.medsafe.govt.nz/profs/PUArticles/June2013Steroid.htm (Accessed: 12 January 2023) It only resolved 3.5 months after stopping all steroid treatments.
However, a retrospective study of 300 patients found that patients who had received hydrocortisone 0.75% and precipitated sulfur 0.5% lotion for up to 15 years for common dermatological conditions of the face showed no evidence of rebound phenomenon, steroid acne, and perioral dermatitis.[10]Harlan, S.L. (2008). Steroid acne and rebound phenomenon. Journal of Drugs in Dermatology. 7(6). 547-550. Available at: PMID:18561585
What are the Long-Term Effects and Safety Profiles of Low Potency Corticosteroids?
There is no specified limit on the duration of use of low-potency corticosteroids. But how safe are they really? Are there any long-term studies showing that these steroids are safe to use long-term?
We’ve collated the longest studies available for several low-potency corticosteroids to help us determine this.
Corticosteroid Study: alopecia Study: other indication Safety profile (adverse effects?) References Alclometasone dipropionate 0.05% N/A Applied twice daily for 21 days in 31 patients with psoriasis. A comparative study with clobetasone butyrate cream 0.5%. No reported adverse events. [11]Aggerwal, A., Maddin, S. (1982). Alclometasone Dipropionate in Psoriasis: A Clinical Study. Journal of International Medical Research. 10, 414-418. Available at: … Continue reading Desonide 0.05% N/A Twice daily application of either desonide 0.05% hydrogel or desonide 0.05% ointment in 46 patients with mild to moderate atopic dermatitis. The study length was 4 weeks. No reported adverse events. [12]Trookman, N.S., Rizer, R.L. (2011). Randomized Controlled Trial of Desonide Hydrogel 0.05% versus Desonide Ointment 0.05% in the Treatment of Mild-to-moderate Atopic Dermatitis. The Journal of … Continue reading Fluocinolone acetonide 0.01% N/A Once daily application for 12 months alongside hydroquinone 4% and tretinoin 0.05% in 228 patients for treating facial melasma. Six cases of telangiectasia (spider veins), 5 mild and 1 moderate. [13]Torok, H.M., Jones, T., Rich, P., Smith, S., Tschen, E. (2005). Hydroquinone 4%, tretinoin 0.05%, fluocinolone acetonide 0.01%: a safe and efficacious 12-month treatment for melasma. Cutis. 75(1), … Continue reading Hydrocortisone 1% Applied twice daily to areas of hair loss for 2 cycles of 6 weeks on and 6 weeks off for a total of 24 weeks. 42 children with alopecia areata. Hydrocortisone 1% compared to clobetasol propionate 0.05%. Twice daily application of either hydrocortisone 1% or desonide 0.05% for 5 weeks in 113 children with mild-to-moderate atopic dermatitis. 36 children continued the study through to 6 months. Alopecia study: 2 patients in the hydrocortisone group experienced abnormal cortisol levels, which were resolved by the end of the study. One patient showed skin atrophy, which resolved by week 6. [14]Lenane, P., Macarthur, C., Parkin, C.P., Krafchik, B., DeGroot, J., Khambalia, A., Pope, E. (2014). Clobetasol Propionate, 0.05%, vs. Hydrocortisone, 1% for Alopecia Areata in Children. A Randomized … Continue reading,[15]Jorizzo, J., Levy, M., Lucky, A., Shavin, J., Goldberg, G., Dunlap, F., Hinds, A., Strelka, L., Baker, M., Tuley, M., Czernielewski, J.M. (1995). Multicenter trial for long-term safety and efficacy … Continue reading,[16]Salava, A., Perala, M., Pelkonen, A.S., Remitz, A., Makela. (2022). Safety of tacrolimus 0.03% and 0.1% ointments in young children with atopic dermatitis: a 36-month follow-up study. Clinical and … Continue reading,[17]Sigurgeirsson, B., Boznanski, A., Todd, G., Vertruyen, A., Schuttelaar, M.L.A., Zhu, X., Schauer, U., Qaqundah, P., Poulin, Y., Kristjansson, S., von Berg, A., Nieto, A., Boguniewicz, M., Paller, … Continue reading Twice daily application of 1. Hydrocortisone 1% or, if needed, hydrocortisone-17-butyrate or 2. 0.03% tacrolimus ointment for a 3-7 day course until clearance was achieved in 152 young children (aged 1-3) with eczema. 3 year follow-up. No side effects were observed for the hydrocortisone group. Application (not mentioned how often) of either pimecrolimus or 1% hydrocortisone in 2418 infants with atopic dermatitis. The treatment was used at the first signs/symptoms until clearance and initiated at the first signs/symptoms of atopic dermatitis. 5-year follow-up. 1% hydrocortisone was associated with an increased incidence of fever, cough, pharyngitis, viral rash, and lower respiratory tract infection. A number of the corticosteroids did not have any studies conducted for alopecia areata. Furthermore, several studies did not report any side effects; however, the corticosteroids were only used for 21 – 28 days in these cases. The study using fluocinolone 0.01% was the longest and was used daily for one year, with few side effects, which is promising.[18]Torok, H.M., Jones, T., Rich, P., Smith, S., Tschen, E. (2005). Hydroquinone 4%, tretinoin 0.05%, fluocinolone acetonide 0.01%: a safe and efficacious 12-month treatment for melasma. Cutis. 75(1), … Continue reading However, the researchers claimed that there were no signs of skin atrophy or thinning, but 6 patients did experience telangiectasia (otherwise known as spider veins) – which incidentally is a sign of skin thinning.[19]Mount Sinai, (no date), Telangiectasia. Mount Sinai. Available at: … Continue reading
The only study that used a low-potency corticosteroid to treat alopecia areata was hydrocortisone 1%. In this study, participants applied hydrocortisone 1% or clobetasol propionate 0.05% twice daily to areas of hair loss for 2 cycles of 6 weeks on and 6 weeks off for 24 weeks. During this time, there were few adverse events reported. These were abnormal cortisol levels, which were resolved before the end of the study. Furthermore, one patient who had extensive alopecia areata showed skin atrophy, which resolved by itself in 6 weeks.[20]Lenane, P., Macarthur, C., Parkin, C.P., Krafchik, B., DeGroot, J., Khambalia, A., Pope, E. (2014). Clobetasol Propionate, 0.05%, vs. Hydrocortisone, 1% for Alopecia Areata in Children. A Randomized … Continue reading
Furthermore, the only two studies that did include long-term follow-up either used very short pulses of the topical corticosteroid treatment or didn’t mention how often it was used at all.
It is clear from the above table that there is a distinct lack of long-term safety data for the use of corticosteroids in dermatological conditions and hair loss conditions. However, short-term or pulsed use (in the case of hydrocortisone) showed very few, if any, adverse effects.
What Role Do Telehealth Companies Play in The Sale and Use of Corticosteroid Treatments?
Telehealth companies provide a convenient alternative to accessing personalized medication and specialized knowledge that may not be readily available in general practice. Furthermore, you can do this from home, eliminating the need for travel and spending time in waiting rooms. You can buy compounded medications from these companies, including mixtures of finasteride, minoxidil, retinoids, and corticosteroids, amongst other treatments.
However, it appears that some telehealth companies may not be providing enough information for the typical buyer to determine how often they should be using their products that contain corticosteroids.
Some of these companies are also burying the known safety concerns of low-potency corticosteroids deep within their website navigations, while also not clearly stating these concerns upfront to prospective consumers. This strategy might help to mitigate these companies from legal actions related to non-disclosures, while at the same time, not truly informing their customers of the very real (and uncertain) risks they may face 2, 3, or 5 years into the future while using their products.
Conclusion
Short-term or pulsed use of low-potency corticosteroids might be safe and effective for hair loss conditions such as alopecia areata. However, the long-term safety of these treatments is less clear, with a distinct lack of extensive, long-term studies. The risks of long-term corticosteroid use are well-documented, which underscores the importance of careful monitoring and following medical guidance when using these treatments. While telehealth companies offer convenience and access to a range of hair loss treatments, including those containing corticosteroids, there is a gap in providing comprehensive safety information and use guidelines that align with the currently available data. This lack of information raises concerns about the potential for overuse or misuse of these products.
References[+]
References ↑1 Macfarlane, D.P., Forbes, S., Walker, B.R. (2008). Glucocorticoids and fatty acid metabolism in humans: fuelling fat redistribution in the metabolic syndrome. Journal of Endocrinology. 197(2), 189-204. Available at: https://doi.org/10.1677/JOE-08-0054 ↑2 Coutinho, A.E., Chapman, K.E. (2011). The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments, and mechanistic insights. Molecular and Cellular Endocrinology. 335(1), 2-13. Available at: https://doi.org/10.1016/j.mce.2010.04.005 ↑3 Yang, J., Young, M.J. (2009). The mineralocorticoid receptor and its coregulators. Journal of Molecular Endocrinology. 43(2), 53-64. Available at: https://doi.org/10.1677/JME-09-0031 ↑4 Gabros, S., Nessel, T.A., Zito, P.M. (2023) Topical Corticosteroids. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532940 ↑5 Stoughton, R.B. (1992). The vasoconstrictor assay in bioequivalence testing: practical concerns and recent developments. International Journal of Dermatology. Available at: https://doi.org/10.1111/j.1365-4362.1992.tb04009.x ↑6 Alsantali, A. (2011). Alopecia areata: a new treatment plan. Clinical Cosmetic and Investigational Dermatology. 4, 107-115. Available at: https://doi.org/10.2147/CCID.S22767 ↑7, ↑8 Stacey, S.K., Mceleney, M. (2021). Topical Corticosteroids: Choice and Application. American Family Physician. 103(6). 337-343. Available at: https://www.aafp.org/pubs/afp/issues/2021/0315/p337.html#:~:text=Triamcinolone%20acetonide%200,Ointment%2C%20cream%2C%20lotion%2C%20gel%2C%20foam (Accessed: 12 January 2024) ↑9 MEDSAFE, (2013). Steroid Rebound – A Topical Issue. MEDSAFE. Available at: https://www.medsafe.govt.nz/profs/PUArticles/June2013Steroid.htm (Accessed: 12 January 2023) ↑10 Harlan, S.L. (2008). Steroid acne and rebound phenomenon. Journal of Drugs in Dermatology. 7(6). 547-550. Available at: PMID:18561585 ↑11 Aggerwal, A., Maddin, S. (1982). Alclometasone Dipropionate in Psoriasis: A Clinical Study. Journal of International Medical Research. 10, 414-418. Available at: https://doi.org/10.1177/030006058201000605 ↑12 Trookman, N.S., Rizer, R.L. (2011). Randomized Controlled Trial of Desonide Hydrogel 0.05% versus Desonide Ointment 0.05% in the Treatment of Mild-to-moderate Atopic Dermatitis. The Journal of Clinical and Aesthetic Dermatology. 4(11), 34-38. Available at: PMID:22125657 ↑13 Torok, H.M., Jones, T., Rich, P., Smith, S., Tschen, E. (2005). Hydroquinone 4%, tretinoin 0.05%, fluocinolone acetonide 0.01%: a safe and efficacious 12-month treatment for melasma. Cutis. 75(1), 57-62. Available at: PMID:15732437 ↑14, ↑20 Lenane, P., Macarthur, C., Parkin, C.P., Krafchik, B., DeGroot, J., Khambalia, A., Pope, E. (2014). Clobetasol Propionate, 0.05%, vs. Hydrocortisone, 1% for Alopecia Areata in Children. A Randomized Clinical Trial. JAMA Dermatology. 150(1). 47-50. Available at: https://doi.org/10.1001/jamadermatol.2013.5764 ↑15 Jorizzo, J., Levy, M., Lucky, A., Shavin, J., Goldberg, G., Dunlap, F., Hinds, A., Strelka, L., Baker, M., Tuley, M., Czernielewski, J.M. (1995). Multicenter trial for long-term safety and efficacy comparison of 0.05% desonide and 1% hydrocortisone ointments in the treatment of atopic dermatitis in pediatric patients. American Academy of Dermatology. 33(1). 0-77. Available at: https://doi.org/10.1016/0190-9622(95)90014-4 ↑16 Salava, A., Perala, M., Pelkonen, A.S., Remitz, A., Makela. (2022). Safety of tacrolimus 0.03% and 0.1% ointments in young children with atopic dermatitis: a 36-month follow-up study. Clinical and Experimental Dermatology. 47(5). 889-902. Available at: https://doi.org/10.1111/ced. ↑17 Sigurgeirsson, B., Boznanski, A., Todd, G., Vertruyen, A., Schuttelaar, M.L.A., Zhu, X., Schauer, U., Qaqundah, P., Poulin, Y., Kristjansson, S., von Berg, A., Nieto, A., Boguniewicz, M., Paller, A.S., Dakovic, R., Ring, J., Luger, T. (2015). Safety and Efficacy of Pimecrolimus in Atopic Dermatitis: A 5-year Randomized Trial. Pediatrics. 135(4). 597-607. Available at: https://doi.org/10.1542/peds.2014-1990 ↑18 Torok, H.M., Jones, T., Rich, P., Smith, S., Tschen, E. (2005). Hydroquinone 4%, tretinoin 0.05%, fluocinolone acetonide 0.01%: a safe and efficacious 12-month treatment for melasma. Cutis. 75(1), 57-62. Available at: PMID:15732437 ↑19 Mount Sinai, (no date), Telangiectasia. Mount Sinai. Available at: https://www.mountsinai.org/health-library/symptoms/telangiectasia#:~:text=Telangiectasias%20of%20the%20skin%20occur,in%20the%20formation%20of%20telangiectasias. (Accessed: 12 January 2024) IngredientsPharmaceuticalsNatural RemediesCompany ReviewsBy Sarah King, PhDJun 23, 2025OS-01 Hair Review: Does It Live Up to the Hype?
Curious about OneSkin’s OS-01 scalp serum that’s all over your feed? It claims to combat hair thinning by targeting cellular senescence, essentially attempting to “rejuvenate” your follicles. In this deep dive, we break down what senescence actually is, how it affects hair loss, and whether the scie...By Sarah King, PhDJun 12, 2025Stretching The Truth: 3 Misrepresented Claims From Hair Loss Studies
Think that new hair growth product sounds too good to be true? It might be. In this article, we break down how research findings in hair loss treatments are often misinterpreted, or worse, misrepresented. From misleading percentages to press release spin, we highlight real examples involving TTFE, N...By Ben Fletcher, PhDMay 19, 2025Does Minoxidil Cause Skin Aging?
Online discussions have raised alarms about a possible link between minoxidil and premature skin aging, especially among users reporting under-eye puffiness, dryness, and fine lines. Could a hair loss treatment really be affecting facial skin quality? This article takes a balanced look at the scienc...By Sarah King, PhDMay 12, 2025Thermus Thermophilus Extract Does Not Increase Hair Density By 96.88%, Despite Dermatology Times’ Claims.
Can Thermus Thermophilus Extract (TTFE) really boost hair density by 96.88%? That’s what a recent Dermatology Times article claimed. But a closer look at the original study tells a very different story. In this article, we unpack the misleading interpretation of TTFE data, why it matters even when i...By Sarah King, PhDMay 5, 2025Does Retinoic Acid (Tretinoin) Improve Hair Growth From Minoxidil?
Retinoic acid, a biologically active form of vitamin A, has long been known for its role in skin health, but could it also help with hair loss? In this article, we explore the science behind retinoic acid and its derivative tretinoin, their effects on hair follicle stem cells, and whether clinical s...By Ben Fletcher, PhDApr 29, 2025Topical Cetirizine: An Anti-Histamine That Regrows Hair? (New Evidence)
Curious if an allergy medication could help with hair loss? Cetirizine, a second-generation antihistamine, is best known for treating allergies, but emerging research suggests it might also promote hair growth when applied topically. From reducing inflammation and mast cell activity to lowering leve...By Sarah King, PhDMar 25, 2025Scalp Psoriasis: Symptoms, Causes, and Effects on Hair Loss
Scalp psoriasis goes beyond surface-level flaking; it’s a chronic autoimmune condition driven by genetic and immune system factors. From thick plaques and itching to potential hair loss, it can seriously impact daily life. Curious about what causes it, how to tell it apart from similar conditions, a...By Sarah King, PhDMar 11, 2025Can Methylene Blue Regrow Your Hair? A Look At The Science.
Methylene blue, a well-known compound with antioxidant and anti-aging properties, has recently gained attention as a potential hair loss treatment. But does the science support the hype? In this article, we examine preclinical research on methylene blue, its mechanisms related to hair health, and wh...By Sarah King, PhDMar 4, 2025Hair Loss Breakthroughs or Media Hype? Stem Cell Secretome Treatments
Stem cell secretome treatments are making headlines as the next big breakthrough in hair regrowth—but do they really work? While the science behind exosomes and growth factors sounds promising, media hype often overshadows the need for rigorous clinical trials. Curious about the real evidence behind...By Sarah King, PhDFeb 25, 2025Seborrheic Dermatitis: Symptoms, Treatments, & Its Impact On Hair Loss
Seborrheic dermatitis is a common cause of dandruff, but what’s really happening to your scalp when it flares up? From excess sebum and yeast overgrowth to genetic factors, this condition has multiple triggers. Wondering what treatments work best and how to manage symptoms long-term? Check out our i... - Mission Statement
 Scroll Down
Scroll Down