- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
Scroll Down
Popular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Free CalculatorTopical Finasteride Calculator
- Free Interactive GuideInteractive Guide: What Causes Hair Loss?
- Free ResourceFree Guide: Standardized Scalp Massages
- Free Course7-Day Hair Loss Email Course
- Free DatabaseIngredients Database
- Free Interactive GuideInteractive Guide: Hair Loss Disorders
- Free DatabaseTreatment Guides
- Free Lab TestsProduct Lab Tests: Purity & Potency
- Free Video & Write-upEvidence Quality Masterclass
- Free Interactive GuideDermatology Appointment Guide
More
Articles100+ free articles.
-
Hims Hair Growth Reviews: The Pros, Cons, and Real Results
-
Topical Finasteride Before and After: Real Case Studies
-
How to Reduce the Risk of Finasteride Side Effects
-
10 Best DHT-Blocking Shampoos
-
Best Minoxidil for Men: Top Picks for 2026
-
7 Best Oils for Hair Growth
-
Switching From Finasteride to Dutasteride
-
Best Minoxidil for Women: Top 6 Brands of 2026
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
Before-Afters- Transformation Photos
Our library of before-after photos.
- Client Testimonials
Read the experiences of members
Before-Afters/ Client Testimonials- Popular Treatments
-
Articles
Anyone searching “How to reverse hair loss online” has undoubtedly come across the Big Three protocol: minoxidil (Rogaine®), finasteride (Propecia®), and ketoconazole shampoo (Nizoral®).
What many might not know: despite ketoconazole’s popularity, it’s not actually FDA-approved for pattern hair loss, nor is it as well-researched as minoxidil or finasteride.
In fact, there are just a few human studies on Nizoral for hair loss and even fewer on people with just androgenic alopecia, the most common form of hair thinning in men.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Is Ketoconazole Worthy of Big Three Status?
Here we’ll uncover the evidence on ketoconazole for hair regrowth. We’ll cut straight-to-the-facts about ketoconazole, its effects on hair loss, and whether or not this shampoo is a good fit. Along the way, we”ll also uncover…
- Which formulation is better: 1% or 2% ketoconazole
- Why not everyone is a good candidate for ketoconazole
- How to (potentially) increase ketoconazole’s efficacy (see our before-after photos)
- Who needs to worry about ketoconazole’s potential side effects
Nizoral for Hair Loss: Overview
- Effort: Low (used as shampoo just 2-3 times per week)
- Expectations: According to studies so far, hair loss improvement is observed after 3-6 months
- Response rate: 80%+
- Regrowth rate: ~5% alone; 25-40% if combined with microneedling and/or finasteride and/or minoxidil
- Cost: Low ($10-$20 per bottle of 100ml, which should last two months)
- Problems: Not as well-studied as finasteride or minoxidil; 2% formulations work better but generally require a prescription (though this can be circumvented online); less studied on women (though it’s likely just as effective)
Key Takeaways
Ketoconazole is a low-cost, low-effort shampoo with practically no side effects. It’s clinically shown to help improve hair loss from both androgenic alopecia (AGA) and telogen effluvium (TE).
While 1% ketoconazole is available over the counter, 2% ketoconazole usually requires a doctor’s prescription. Studies show that 2% ketoconazole is more effective, particularly in helping to normalize excessive hair shedding from rapid-onset AGA and/or TE. [1]https://pubmed.ncbi.nlm.nih.gov/9669136/
Can Nizoral help with hair growth?
If a 2% prescription-strength formulation is used, yes.
By itself, ketoconazole is unlikely to stimulate hair regrowth on par with finasteride or combination therapies. So, ketoconazole is just one part of a multi-pronged hair loss regimen. This shampoo may have synergistic effects with stimulation-based therapies like microneedling, massaging, and/or platelet-rich plasma therapy. It also seems to pair well with most FDA-approved / FDA-cleared treatments like finasteride, minoxidil, and low-level laser therapy.
While oral ketoconazole comes with significant risks of side effects, 2% ketoconazole shampoo seems to carry little (if any) risks of side effects – mainly because of its low time of exposure and systemic absorption versus its oral formulations.
The best candidates for 2% ketoconazole shampoo are hair loss sufferers who are comfortable using the shampoo 2-3 times per week and who are dealing with dandruff and/or excessive hair shedding from AGA or TE.
More information on the science behind ketoconazole – its mechanisms of action, supporting evidence, expectations for hair regrowth, and contraindications – can be found below.
What Is Ketoconazole?
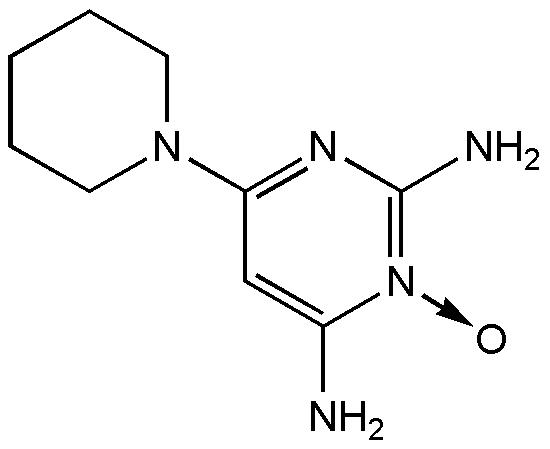
Ketoconazole: molecular structure
Ketoconazole is more commonly mentioned by the brand name Nizoral®, and most people know about it as a shampoo.
Simply put, ketoconazole is an anti-fungal medication. It’s a drug commonly used to help improve fungal-related conditions – like dandruff, fungal infections, certain hormone-linked diseases, and even hair loss from fungal and non-fungal causes.
If it’s a fungal medication, why is it used for hair loss?
Because ketoconazole’s mechanisms of action – as an anti-fungal, anti-inflammatory, anti-androgenic, and pro-anagen agent – all overlap with the causes of telogen effluvium and androgenic alopecia.
Here’s how.
Ketoconazole’s anti-fungal properties help fight off yeast, fungi, and bacterial infections that can cause excessive hair shedding.
As an anti-fungal medication, ketoconazole may also have anti-inflammatory effects, especially in hair follicle sites.[2]https://www.ncbi.nlm.nih.gov/pubmed/9669136
Many yeast, fungi, and bacteria feed off our dead skin as well as the oils our skin produces (i.e., sebum) which helps to lubricate our hair. Resultantly, these species can often be found residing in parts of our hair follicle – specifically, the infundibulum (i.e., the upper third of each hair shaft) and sebaceous glands.
However, sometimes too many yeast, fungi, and/or bacteria may colonize our sebaceous glands – leading to over-colonization. This is particularly true with the fungus-like yeast species Malassezia spp., which is found in 65% of healthy scalps.[3]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367942/
Many of these species produce toxic byproducts (i.e. porphyrins) as part of their digestion of sebum. In cases of over-colonization, the accumulation of toxins elicits an inflammatory response in the sebaceous gland. Ironically, the body often responds by sending more sebum to the sebaceous glands – which would help to otherwise resolve the inflammation, but not in these instances. Rather, the excess sebum simply feeds these pathogenic microorganisms, and the process continues.
This is known as a sebum-feedback loop. At moderate levels, it leads to excessive dandruff. At higher levels, it triggers excessive hair shedding – often characterized as microorganism-driven telogen effluvium (TE).
Enter ketoconazole – a potent anti-fungal medication that can help kill off these pathogens and, in doing so, stop this feedback loop.
Ketoconazole damages the cell membranes of fungi and yeast.[4]https://pubchem.ncbi.nlm.nih.gov/compound/Ketoconazole Specifically, it stops a fungus from producing ergosterol – a crucial part of the cell membrane that helps keep cellular content from leaking out as well as unwelcome substances from invading.
The end result?
Ketoconazole helps kill off pathogenic yeast/fungi, which then reduces scalp inflammation and helps resolve any excessive hair shedding (TE).
This is also why ketoconazole is such an effective treatment for scalp conditions caused by fungi – like dandruff and seborrheic dermatitis. Those conditions are also often caused by Malassezia spp. – the fungus-like yeast that is (fortunately) hypersensitive to ketoconazole.
Ketoconazole might help reduce inflammation in 30-50% of men with androgenic alopecia
Research shows that 30-50% of hair loss sufferers with androgenic alopecia (AGA) also have P. acnes and/or Malassezia spp. infections in the scalp. Just like with TE, the presence of these microbes may exacerbate inflammation, induce early hair shedding, and thereby accelerate the progression of AGA.
In these cases, anti-fungal and/or antibacterial shampoos tend to be useful – because they help to reduce the infections that are accelerating hair shedding in AGA.
Ketoconazole might have anti-androgenic effects in scalp tissues
Ketoconazole isn’t just an anti-fungal; it also has anti-androgenic properties when taken orally. And, while researchers have debated whether these findings extend to topically applied ketoconazole, at least one peer-reviewed paper makes a strong argument in its favor.
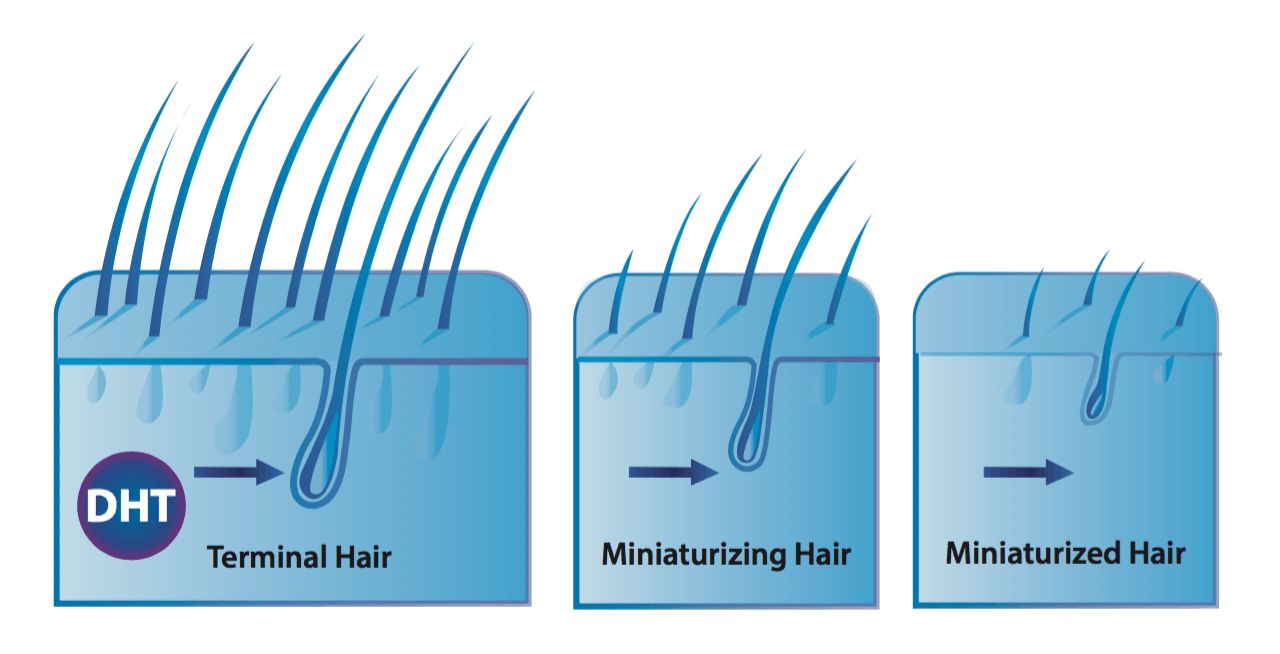
Specifically, this hypothetical model argues that topically applied ketoconazole has anti-androgenic properties.[5]https://www.ncbi.nlm.nih.gov/pubmed/14729013 In particular, it may help reduce dihydrotestosterone (DHT) – the main hormone implicated in AGA – and in two ways:
- Inhibits 5-alpha reductase. This is an enzyme that converts free testosterone into DHT.
- Blocks androgen receptors. Androgen receptors are where DHT attaches to a cell to influence tissue function (i.e., hair follicle miniaturization). If androgen receptors are blocked, DHT cannot bind to these cells, and thus does not affect that tissue’s functionality.
Together, if ketoconazole has enough of a DHT-reducing effect in balding scalp tissues, it should help to improve AGA – similar to the ways in which treatments like finasteride work.
Ketoconazole may prolong the anagen phase of the hair growth cycle
At any given moment, roughly 85% of scalp hairs are in their growth (anagen) phase, while remaining hairs are either in a resting (catagen) or shedding (telogen) phase.
One defining characteristic of telogen effluvium (TE) is a large increase in the number of shedding versus growth phase hairs (i.e., increased telogen:anagen ratio). In TE, it’s not uncommon to see telogen:anagen ratios of 40-50% and beyond.
This is also observed in androgenic alopecia (AGA) – though to a lesser degree, as AGA is characterized more so by hair follicle miniaturization, less so by hair shedding.
Interestingly, one research team demonstrated that, for reasons unknown, ketoconazole appears to prolong the anagen (growth) phase of hair follicles affected by TE and/or AGA.[6]https://www.ncbi.nlm.nih.gov/pubmed/18498517
This effect should help delay the progression of both conditions, and maybe even partially reverse them.
Summary of Mechanisms
Ketoconazole might improve telogen effluvium by:
- Killing off pathogens in the scalp, thus normalizing excessive hair shedding triggered by microorganism-mediated inflammation
- Prolonging the anagen phase of the hair cycle
Ketoconazole might improve androgenic alopecia by:
- Killing off pathogens in the scalp, thus normalizing excessive hair shedding triggered by microorganism-mediated inflammation
- Reducing scalp DHT levels by inhibiting 5-alpha reductase and blocking androgen receptors
- Prolonging the anagen phase of the hair cycle
Altogether, these mechanisms suggest that ketoconazole may improve both TE and AGA. So, what’s the evidence in human studies?
Clinical studies: is ketoconazole effective for hair loss?
As is always the case with hair loss research, context is key. And when looking into the effectiveness of ketoconazole, we need to evaluate all clinical studies with several things in mind:
- Was the ketoconazole tested on androgenic alopecia or other hair loss disorders?
- Was the formulation strength 1% or 2%?
- What, exactly, was measured?
To date, there are only four clinical studies on ketoconazole and hair loss (that we could find). As such, we’ll present them in detail. If you’d like, you can skip to the summaries of each study.
Ketoconazole Shampoo: Effect of Long-Term Use in Androgenic Alopecia
Full text: Piérard-Franchimont et al., 1998 [7]https://www.ncbi.nlm.nih.gov/pubmed/9669136
Study one: 2% ketoconazole versus a normal shampoo
- Who: 39 male only-AGA-subjects
- What: 2% ketoconazole shampoo versus a normal shampoo. During the study duration, 27 men used ketoconazole while 12 men used normal shampoo. There were also 22 non-AGA-controls – half of them testing ketoconazole; half of them trying normal shampoo.
- How long: 2-4 times per week for 21 months
- Measurement: AGA pilary index (PI). This was defined as the percentage of hairs in anagen (A) x average diameter (D, μm) of the hair shafts 1.5 cm from the hair bulb.
- Results:
- PI of non-AGA-controls remained unchanged, no matter the type of shampoo used (ketoconazole versus normal shampoo).
- PI of only-AGA-subjects with unmedicated shampoo showed a slow linear decrease over time, while the ketoconazole group “yielded a progressive PI increase that became evident after a 6-month survey and apparently reached a plateau value after about 15 months”.
- Takeaways:
- In men without androgenic alopecia, ketoconazole doesn’t improve anagen hair counts or hair shaft diameter
- In men with androgenic alopecia, ketoconazole improves both anagen hair counts and overall hair shaft diameter
Study two: 2% ketoconazole versus 2% minoxidil
- Who: 8 male only-AGA-subjects; 4 using ketoconazole, and 4 using minoxidil
- What: 2% ketoconazole shampoo (vs. 2% minoxidil lotion)
- How long: ad libitum (i.e., as often as desired) for 6 months
- Measurements: hair density; hair shaft diameter and the corresponding sebaceous gland
- Results:
- “A 7% increase in the median hair shaft diameter was yielded by both the [ketoconazole] shampoo and minoxidil + unmedicated shampoo combination.”
- “A 19.4% decrease in the mean sebaceous gland area was observed in the [ketoconazole] group. In contrast, the same variable increased by 5.3% in the minoxidil + unmedicated shampoo group.”
- Ketoconazole improved density of hair by 18% compared to minoxidil by 11%.
- Takeaways:
- Ketoconazole increases hair shaft diameter by 7%, similar to minoxidil
- Ketoconazole decreases sebaceous gland size by nearly 20% – possibly due to its anti-fungal effects. In other words, ketoconazole kills off pathogens that over-colonize, and thereby over-enlarge, the sebaceous glands. This was unique to ketoconazole (minoxidil did not have this effect).
- Ketoconazole improves hair density nearly twice as well as minoxidil
Key points:
These studies are all on men with AGA only, all of whom tested 2% ketoconazole as a shampoo.
The results all show significant improvements to hair density, as well as prolonged anagen phases and hair diameter. Moreover, one study also found that ketoconazole decreased sebaceous gland size – most likely a result of its ability to kill off pathogens overcrowding those sebaceous glands. For these reasons, it’s not unreasonable to assume that ketoconazole might also decrease sebum output.
Nudging hair shedding by antidandruff shampoos. A comparison of 1% ketoconazole, 1% piroctone olamine, and 1% zinc pyrithione formulations
Full text: Piérard-Franchimont et al., 2002 [8]https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1467-2494.2002.00145.x
- Who: 150 men presenting with telogen effluvium related to androgenic alopecia associated with dandruff, separated into three groups with different shampoos: 50 men on 1% ketoconazole, 50 on 1% piroctone olamine, and 50 on 1% zinc pyrithione
- What: 1% ketoconazole shampoo versus two other anti-dandruff shampoos
- How long: 2-3 times a week, for 6 months
- Measurements: hair shedding, hair density, anagen hair percentage, mean proximal hair shaft diameter, sebum excretion rates
- Results:
- Pruritus and dandruff cleared rapidly in all three shampoo groups
- Hair density remained unchanged in all three shampoo groups
- Hair shedding decreased by 17.3% in the ketoconazole group, 16.5% in the piroctone olamine group, and 10.1% in the zinc pyrithione group
- Anagen hair ratio increased by 4.9% in the ketoconazole group, 7.9% in the piroctone olamine group, and 6.8% in the zinc pyrithione group
- Sebum excretion rate decreased by 4.8% in the ketoconazole group, 2.9% in the piroctone olamine group, and 5.5% in the zinc pyrithione group
Key points:
The men featured in this study have telogen effluvium and androgenic alopecia. And, encouragingly, it seems like 1% ketoconazole shampoo 2-3 times per week lessened hair shedding by ~20%, increased hair shaft thickness by ~5%, and decreased sebum output by ~5%.
The bottom-line: comparing across studies, 1% ketoconazole isn’t as impressive as 2%, but the results are still there. For men (and women) suffering from both TE and AGA, 1% or 2% ketoconazole might be a great intervention (among other treatments).
Comparative Efficacy of Various Treatment Regimens for Androgenetic Alopecia in Men
Full text: Khandpur et al., 2002 [9]https://www.ncbi.nlm.nih.gov/pubmed/12227482
- Who: 100 male only-AGA-subjects randomized into four groups:
- 30 finasteride
- 36 finasteride + minoxidil
- 24 minoxidil
- 10 finasteride + ketoconazole
- What: 2% ketoconazole shampoo + finasteride 1mg oral/day (vs. finasteride vs. finasteride + 2% minoxidil vs. 2% minoxidil)
- How long: 3 times a week for 1 year
- Measurements: patients’ self-assessment and physicians’ assessment. Photographs were taken.
- Results: finasteride + minoxidil and finasteride + ketoconazole reap the best improvement scores for both self- and physician-assessments. However, finasteride + minoxidil slightly outperformed finasteride + ketoconazole.
Key points:
2% ketoconazole works well as a combination therapy with finasteride.Pilot Study of 15 Patients Receiving a New Treatment Regimen for Androgenic Alopecia: The Effects of Atopy on AGA
Full text: A.W. Rafi et al., 2011 [10]https://www.ncbi.nlm.nih.gov/pubmed/22363845
- Who: 15 AGA subjects with either atopic dermatitis or seborrheic dermatitis
- What: 2% ketoconazole shampoo. 8 subjects used NuH Hair + finasteride + minoxidil + ketoconazole, 5 using only NuH Hair, 1 using NuH Hair + finasteride + ketoconazole, 1 using NuH Hair + ketoconazole (a subject with seborrheic dermatitis)
- How long: ketoconazole usage 2-3 times a week for 9 months
Measurements: Average time for hair regrowth, photo and investigator assessments - Results:
- Average time for hair regrowth
- 30 days with NuH Hair + finasteride + minoxidil + ketoconazole
- 30 days with NuH Hair + finasteride + ketoconazole
- 60 days with NuH Hair + ketoconazole
- 90 days with NuH Hair alone
- Average time for hair regrowth
Key points:
Ketoconazole works well as a combination therapy with finasteride and minoxidil, and it can also improve AGA even in men with atopic and/or seborrheic dermatitis.Key points summary of clinical trials
- By itself and as a combination therapy, 2% ketoconazole improves AGA and TE by:
- Increasing anagen (growth) hairs
- Increasing hair shaft diameter
- Increasing hair density
- Hair improvements from 2% ketoconazole seem to sustain, not wane (at least over 21 months of use)
- 2% ketoconazole increases hair density; 1% ketoconazole doesn’t
Very broadly speaking, ketoconazole alone might be a little bit less effective than minoxidil alone, but it also seems to be a better bet in some respects: more people respond to Nizoral for hair loss, its effects don’t wane over 21 months, and it targets AGA from multiple angles.
Applying Ketoconazole
If you want to get the most out of ketoconazole, here are some tips to maximize your chances of hair regrowth and use ketoconazole in the most effective way:
Opt for 2% prescription, not 1% over-the-counter
There is evidence that prescription-strength 2% ketoconazole is (much) more effective than 1 % ketoconazole.
In this study, 2% ketoconazole shampoo increased hair density by 18% while in this study, 1% ketoconazole shampoo didn’t change hair density at all. Both times, ketoconazole was applied around 3 times a week for 6 months. [11]https://www.ncbi.nlm.nih.gov/pubmed/9669136 [12]https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1467-2494.2002.00145.x
Also, in this study, 1% ketoconazole and 2% ketoconazole were compared with their effect on seborrheic dermatitis, and the results were so that “[ketoconazole] 2% had superior efficacy compared to [ketozonaole] 1% in the treatment of severe dandruff and scalp seborrheic dermatitis.”[13]https://www.karger.com/Article/PDF/51628
So get the 2% ketoconazole, not the 1%.
How can I get the 2% Nizoral shampoo without a prescription?
One of our members found 2% ketoconazole online, and from a company called Nizoral Shop.
So how does this company was circumventing prescriptions and shipping to the U.S. (and elsewhere)?
As it turns out, their Nizoral products depart from overseas warehouses where prescriptions are not required.
So, for anyone looking for 2%, Nizoral Shop might be a great option. The company later offered our members a 20% discount on the first 100 orders from our community.
To access case studies, expert interviews, forums, comprehensive guides, and other special offers, join our membership. You will also get a personalized Regrowth Roadmap tailored to your needs and treatment preferences.
We aren’t affiliated with any physical product brands, and we haven’t tried this shampoo brand. The company did say that for anyone making orders during the COVID-19 period: “It is highly recommended to select UPS/DHL priority express shipping option, as the other shipping methods are suspended until further notice due to the current pandemic.”
Get the Nizoral shampoo, not the topical
This is just a practical tip. In some countries, there is a topical version of ketoconazole available to consumers. Arguably, as a topical, ketoconazole would likely have more significant effects versus a shampoo – mainly because of the differences in the length of time on the scalp.
At the same time, topical ketoconazole may be more likely to cause side effects due to higher systemic absorption. What’s more, the topical non-shampoo version of ketoconazole has never been used in human studies on hair loss.
So, we recommend sticking to what’s studied; not what’s theoretically potentially more effective. Go with Nizoral shampoo.
Apply 2-4 times per week
Collectively, these studies show that applying 2% ketoconazole 2-3 times per week seems to show the most promise at resolving hair loss disorders and not just dandruff. So, plan on using this shampoo around every other day.
Do I have to use it forever?
Not necessarily. If ketoconazole’s most beneficial mechanism of action is that it kills off the over-colonization of pathogenic organisms that are creating additional scalp inflammation, then chances are that after these pathogenic organisms are gone, you may be able to significantly reduce usage frequencies after months 3-4.
That means transitioning to once-weekly usage (or less).
Combine ketoconazole with other hair loss therapies and treatments
Generally speaking, in ketoconazole studies on humans with AGA, the best results have been achieved by those that used ketoconazole in combination with other treatments.
This makes sense, as ketoconazole’s mechanisms of action are different from minoxidil, which are different from microneedling, which are different from finasteride. The more mechanisms you target, the better your results (in most cases).
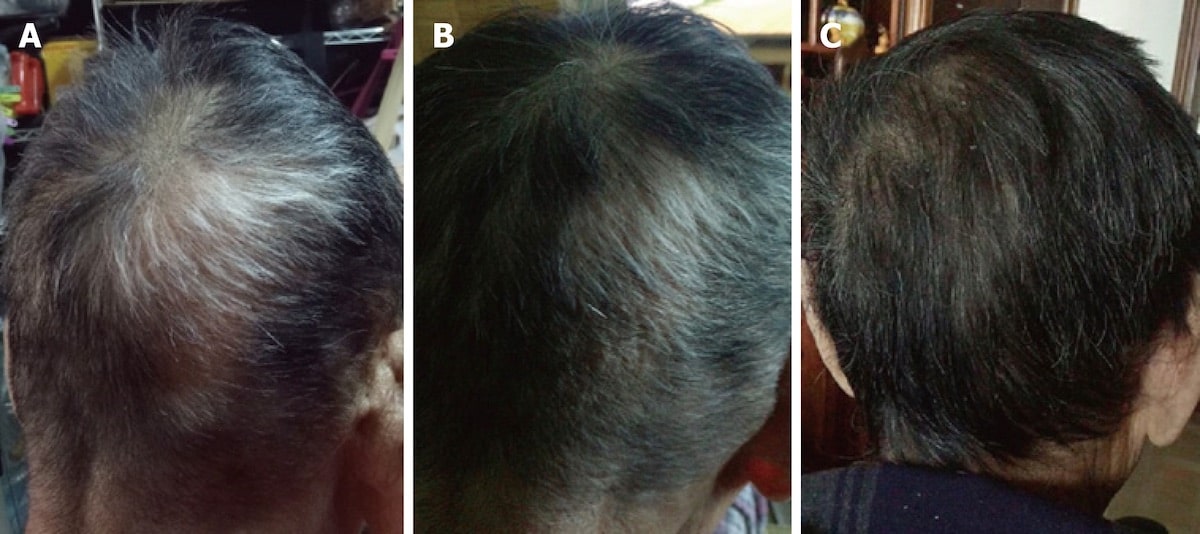
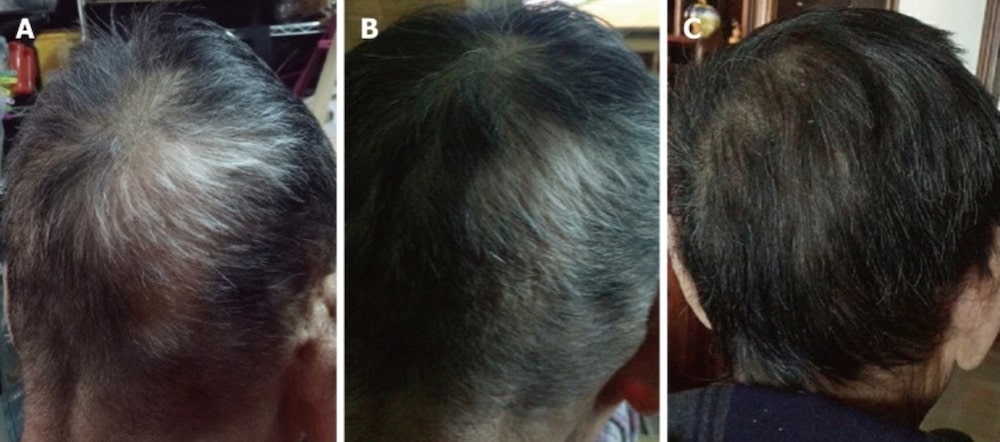
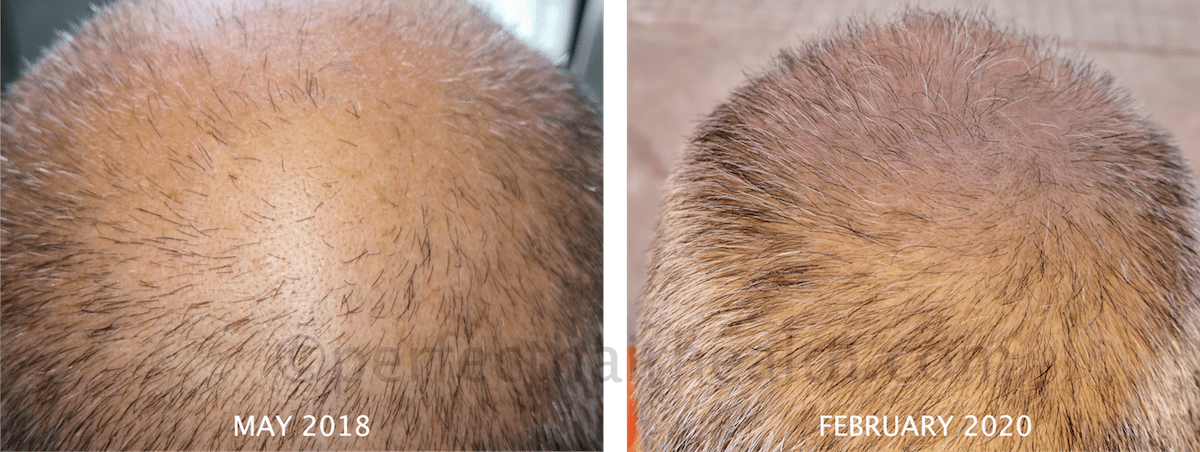
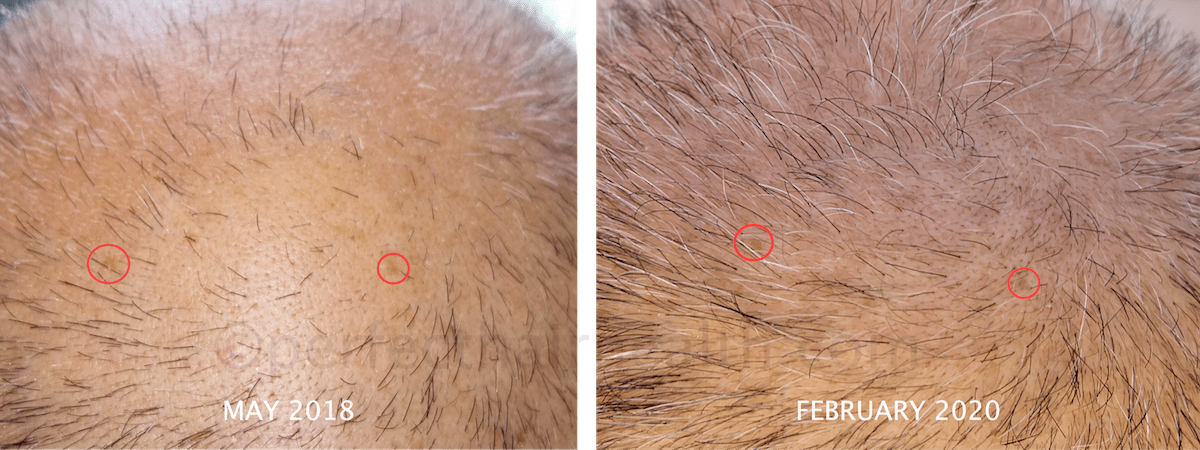
In fact, we have an example from our community of a member doing just this: combining ketoconazole with microneedling, massaging, and minoxidil to break through a period of stagnation in hair recovery.
Here are his results: 20+ months of scalp massage alongside microneedling, minoxidil, and ketoconazole
Hair growth from scalp massage alongside microneedling, minoxidil, and ketoconazole
Nizoral for Hair Loss: The Side Effects
This study showed that high doses of oral ketoconazole can impair testosterone production in men, but this review article from drugs.com states that these effects haven’t been reported – even with topical ketoconazole – and seem unlikely anyway because through topical application, way too little substance is absorbed.[14]https://www.ncbi.nlm.nih.gov/pubmed/3659003[15]https://www.drugs.com/monograph/ketoconazole-topical.html
So, based on this information, you don’t need to worry about the shampoo’s effect on testosterone.
Rare side effects are summarized here. These are not prevalent, particularly if ketoconazole is formulated as a shampoo.[16]https://www.drugs.com/sfx/ketoconazole-topical-side-effects.html
All in all, ketoconazole shampoo seems to be relatively free of side effects, and a relatively safe option for those with excessive hair shedding from androgenic alopecia, telogen effluvium, or both.
For those with sensitive skin who wish to try a more natural Nizoral formulation, Sent from Earth Caffeine & Saw Palmetto Shampoo may suffice. However, this shampoo contains just 1% ketoconazole. We are not affiliated with this company; we just wanted to provide an example of what else is out there.
Who are the best candidates for Nizoral?
In regard to hair loss sufferers, ketoconazole is proven to help:
Those with androgenic alopecia
Having checked the studies above, it is pretty indisputable that ketoconazole improves AGA in humans – and not only in those who suffer additionally from seborrheic dermatitis or telogen effluvium, but clearly also in those who have only AGA. [17]https://www.ncbi.nlm.nih.gov/pubmed/9669136
Those with a hair shedding disorder (like telogen effluvium)
When TE is derived from a pathogenic microorganism, seborrheic dermatitis, or both (which can be the case), ketoconazole might help – as its anti-fungal effects can intervene in the earliest stages of seborrheic dermatitis development.[18]https://donovanmedical.com/hair-blog/2017/5/23/is-it-possible-for-seb-derm-to-cause-hair-loss
Interestingly, ketoconazole seems to improve TE regardless of its causes. We know this from the above study with 150 TE men, which showed that ketoconazole improved TE outcomes – despite the high likelihood of myriad TE causes present within that study.[19]https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1467-2494.2002.00145.x
These studies are mostly on men. What about women?
To our knowledge, there are no published studies on Nizoral for hair loss in females with pattern alopecia (yet). However, one study on females found that 2% ketoconazole as a topical (not shampoo) demonstrated similar efficacy compared to 2% minoxidil over six months of use.[20]https://biomeddermatol.biomedcentral.com/articles/10.1186/s41702-019-0046-y
Given the results of this study (and ketoconazole’s suspected mechanisms of action), there is reason to believe ketoconazole shampoo is probably effective for women, as well.[21]https://www.derm.theclinics.com/article/S0733-8635(12)00093-9/abstract
You’re an ideal candidate for ketoconazole if you…
- Suffer from AGA and/or a hair shedding disorder, particularly alongside seborrheic dermatitis or symptoms of microorganism overgrowths (like excessive dandruff and/or sebum activity)
- Want the benefit of a chemical treatment without a high risk of severe side effects
- Are using minoxidil/finasteride and want to increase their efficacy
- Are performing stimulation-based therapies (i.e., massaging, microneedling, and/or platelet-rich plasma) and want to speed up the regrowth process.
Who is not a good candidate for ketoconazole?
Ketoconazole is less researched on women, although that doesn’t make it less effective. But there are contraindications for oral ketoconazole in pregnant women – and, as a precaution, the standard recommendation is for all women who intend on getting pregnant to avoid even the topical formulations.[22]https://www.drugs.com/pregnancy/ketoconazole.html
Regarding mothers who breastfeed, ketoconazole use is generally considered acceptable, but caution is recommended.[23]https://www.drugs.com/breastfeeding/ketoconazole.html
Above all, both men and women are strongly advised against the use of oral ketoconazole for the treatment of AGA/pattern hair loss. While topical/shampoo formulations have a strong safety profile, oral ketoconazole doesn’t. Consequently, it comes with a higher risk of side effects and is even banned from sale in certain countries.
Summary
Ketoconazole isn’t as well-researched as minoxidil or finasteride. However, studies show that it might be an effective add-on treatment for hair loss (specifically, androgenic alopecia).
There’s evidence that ketoconazole is almost as effective as minoxidil (Rogaine®) at increasing hair density… and that it might be particularly helpful for those with pattern hair loss with rapid hair shedding (i.e., telogen effluvium). So, if you fit within these categories, you might want to consider trying it.
Having said that, ketoconazole formulation matters. While 1% over-the-counter ketoconazole might help reduce dandruff and improve hair loss, 2% prescription ketoconazole is likely superior in its ability to improve hair loss outcomes. So, if you’re going to commit to Nizoral for hair loss, commit fully. Visit your doctor and get a prescription. Or, order online from the Nizoral Shop. Then, start shampooing.
References[+]
References ↑1 https://pubmed.ncbi.nlm.nih.gov/9669136/ ↑2, ↑7, ↑11, ↑17 https://www.ncbi.nlm.nih.gov/pubmed/9669136 ↑3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367942/ ↑4 https://pubchem.ncbi.nlm.nih.gov/compound/Ketoconazole ↑5 https://www.ncbi.nlm.nih.gov/pubmed/14729013 ↑6 https://www.ncbi.nlm.nih.gov/pubmed/18498517 ↑8, ↑12, ↑19 https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1467-2494.2002.00145.x ↑9 https://www.ncbi.nlm.nih.gov/pubmed/12227482 ↑10 https://www.ncbi.nlm.nih.gov/pubmed/22363845 ↑13 https://www.karger.com/Article/PDF/51628 ↑14 https://www.ncbi.nlm.nih.gov/pubmed/3659003 ↑15 https://www.drugs.com/monograph/ketoconazole-topical.html ↑16 https://www.drugs.com/sfx/ketoconazole-topical-side-effects.html ↑18 https://donovanmedical.com/hair-blog/2017/5/23/is-it-possible-for-seb-derm-to-cause-hair-loss ↑20 https://biomeddermatol.biomedcentral.com/articles/10.1186/s41702-019-0046-y ↑21 https://www.derm.theclinics.com/article/S0733-8635(12)00093-9/abstract ↑22 https://www.drugs.com/pregnancy/ketoconazole.html ↑23 https://www.drugs.com/breastfeeding/ketoconazole.html Studies show that within 3-6 months of stopping minoxidil, any hair growth resulting from the drug is lost. After quitting minoxidil, hair counts can even temporarily fall below where they would’ve been had we never sought treatment at all, before eventually rebounding back to baseline.
Why does this happen? Is there a way to lessen the “withdrawal shed” from minoxidil? For those who’ve seen hair gains with minoxidil but prefer not to use it forever, there may be some methods to mitigate shedding after quitting minoxidil. This article explains the evidence, and provides an action plan.
- About Minoxidil
- Why People Stop Taking Minoxidil
- What Happens When Quitting Minoxidil
- Is Minoxidil Plus Microneedling the Answer?
- How to (Possibly) Prevent Shedding After Stopping Minoxidil
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

About Minoxidil
Minoxidil is an over-the-counter drug approved by the FDA to treat androgenic alopecia. It’s commonly known by the brand name Rogaine. Along with finasteride, minoxidil is one of only two drugs approved to treat androgenic alopecia in both men and women.
Nobody actually knows how minoxidil works. Minoxidil was initially developed in the 1980s as an oral drug to treat high blood pressure. But when patients started reporting “unwanted” hair regrowth after three or more months of use, its manufacturers decided to reformulate it into a topical and begin testing it on men with androgenic alopecia.[1]https://www.jaad.org/article/S0190-9622(08)00809-8/abstract
Today, we still aren’t sure how it works. But since side effects are minimal, it was nonetheless approved by the FDA for use. There are two primary hypotheses on the mechanisms behind minoxidil.
Hypothesis 1: Minoxidil is a Vasodilator
One defining characteristic of androgenic alopecia is reduced blood flow to balding regions. While there’s debate over whether reduced blood flow is a consequence or cause of hair loss, it’s undisputed that without proper blood supply to a hair follicle, hair cannot grow.
As a vasodilator, minoxidil widens blood vessels, potentially increasing blood flow to the scalp. In addition, Minoxidil opens potassium ion channels, which some researchers think works alongside vasodilation to improve hair growth.[2]https://pubmed.ncbi.nlm.nih.gov/9395721/
Hypothesis 2: Minoxidil Alters the Hair Growth Cycle
It’s possible that minoxidil kicks miniaturizing hair follicles back into the anagen (growth) phase of the hair cycle. Hairs thus become thicker, giving the appearance of overall improved hair density. This could be the result of minoxidil decreasing prostaglandin D2 levels while boosting other prostaglandins, like prostaglandin E2, to downregulate pro-inflammatory growth factors that are linked to hair shedding.[3]https://www.jidonline.org/article/S0022-202X(15)42806-4/pdf
In addition, Minoxidil may prolong the growth phase of the hair cycle by maintaining beta-catenin activity in dermal papilla cells.[4]https://pubmed.ncbi.nlm.nih.gov/21524889/
How Long Does Minoxidil Take to Work?
Minoxidil’s event horizon is approximately 3-6 months. Over half of the people who try it respond to minoxidil within this time frame. But early results tend to wane over time.
One study found that at six months, men using 5% minoxidil twice-daily saw a near-60% change in hair ‘weight’ in balding regions.[5]https://www.sciencedirect.com/science/article/pii/S019096229970006X In other words, their hair had thickened or regrown to weigh 60% more than it did at the start of the study.
That’s huge.
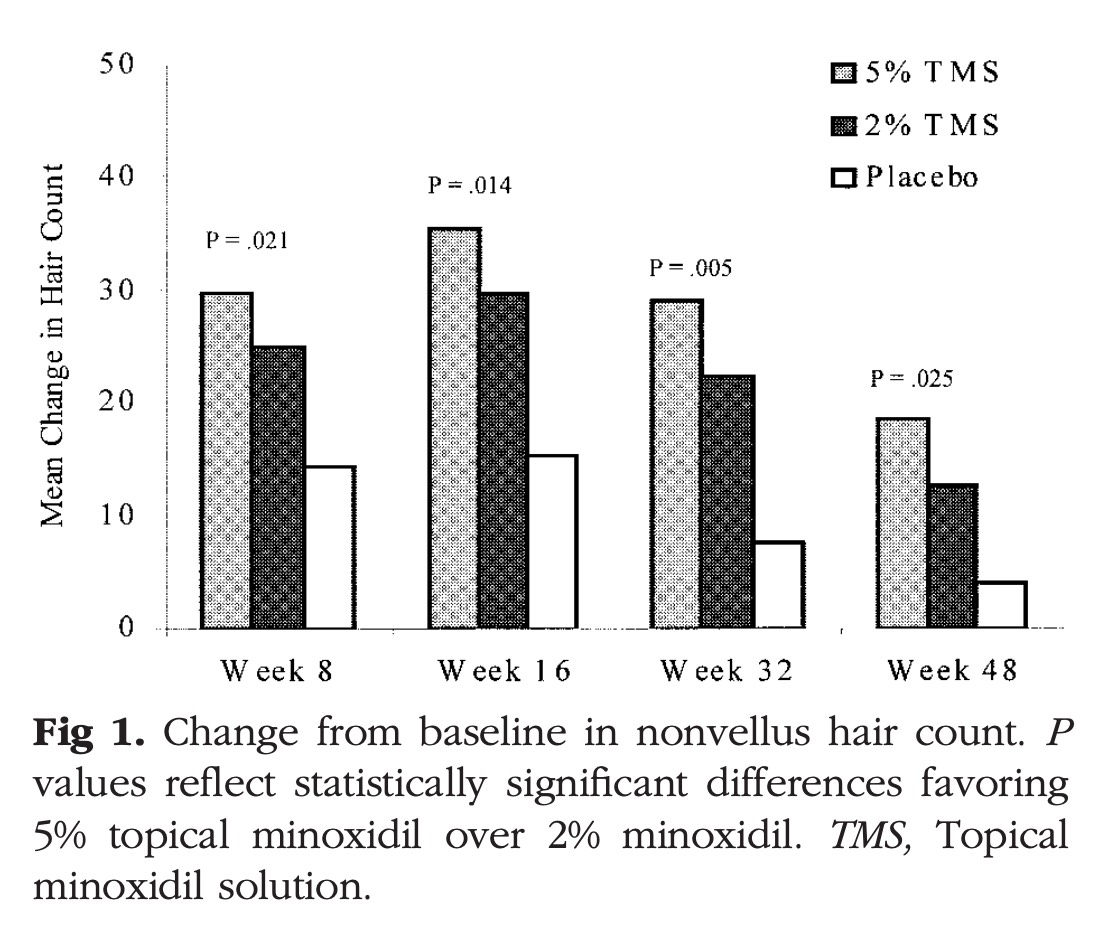
Unfortunately, the same study showed that at 96 weeks, those hair weights decreased to merely 25% higher than baseline. This also happens to be a consistent finding across most studies on minoxidil. Just see this 48-week chart on the effects of 2% and 5% minoxidil on hair counts.[6]https://pubmed.ncbi.nlm.nih.gov/12196747/ Results tend to peak at week 16, then decline thereafter.
Olsen, E. A., Dunlap, F. E., Funicella, T., Koperski, J. A., Swinehart, J. M., Tschen, E. H., & Trancik, R. J. (2002). A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. Journal of the American Academy of Dermatology, 47(3), 377–385.
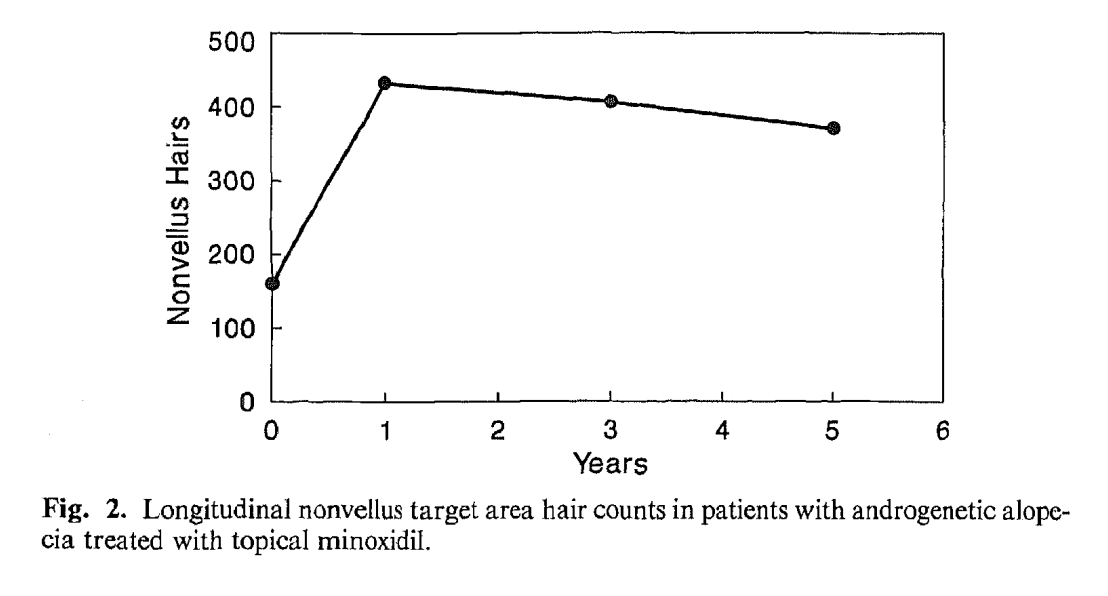
This is echoed on 5-year studies on minoxidil, which show a steady decline in non-vellus hair counts in target areas after year one: [7]https://pubmed.ncbi.nlm.nih.gov/2180995/
Olsen, E. A., Weiner, M. S., Amara, I. A., & DeLong, E. R. (1990). Five-year follow-up of men with androgenetic alopecia treated with topical minoxidil. Journal of the American Academy of Dermatology, 22(4), 643–646.
Somewhat relatedly, other studies have demonstrated greatly increased hair counts that failed to translate to visual improvements in hair density.[8]https://www.jaad.org/article/S0190-9622(08)00809-8/abstract
Long-story short: over time, minoxidil’s efficacy begins to wane. And while minoxidil can temporarily increase hair counts, these increases don’t always lead to cosmetic levels of hair regrowth.
Why is this?
Minoxidil helps kickstart hairs back into the anagen (growth) phase of the hair cycle. However, it doesn’t address DHT-driven hair follicle miniaturization. So, while hair counts increase, hair diameters continue to decline, leading to a loss of hair volume and thereby hair thinning over time.
Most people who try minoxidil quit within a year as their results stabilize or slowly decline.
Let’s take a closer look at why, and what happens when they do.
Why Stop Taking Minoxidil?
People who stop taking minoxidil tend to fall into two main camps. Either minoxidil is just not working for them at all, or it is working, but for various reasons, they’d prefer to pass on a twice-daily application for the rest of their lives.
Minoxidil Non-Responders
Some people simply don’t respond to minoxidil. This could be a sign their hair loss stems from a condition other than androgenic alopecia. But as we’ll see, minoxidil just doesn’t always work well on its own.
Is it Androgenic Alopecia?
Non-response to minoxidil could signify that hair loss is not due to androgenic alopecia but something else. There’s some evidence that oral minoxidil might improve hair shedding disorders like chronic telogen effluvium, but it’s technically not FDA-approved for that condition.[9]https://link.springer.com/article/10.1007%2Fs40257-018-0409-y
Is it Strong Enough?
When choosing between 2% and 5%, choose the more potent formula. Studies show that in men, 5% minoxidil is better than the 2% formula, and the same is likely true for women. Prescriptions are available for concentrations of 10% or 15%, and studies show minoxidil non-responders often see better hair growth after switching to these strengths.[10]https://pubmed.ncbi.nlm.nih.gov/28078868/
Is it in Use as a Monotherapy?
The reality is that minoxidil just isn’t very effective by itself. To understand why it helps to learn about an enzyme called Sulfotransferase.
In order to become active, minoxidil must come into contact with Sulfotransferase. About 40% of balding men just don’t have enough Sulfotransferase to elicit a response to Minoxidil – which happens to closely correspond with the percent of non-responders of minoxidil.
What might help increase Sulfotransferase levels? We’ll get to that later.
The Downsides of Minoxidil
Even minoxidil responders may not want to use it forever. It can be costly and inconvenient, and it does have some minor side effects.
Cost
Monthly minoxidil use costs between $15-$40. Hair loss sufferers will need to try it for 6 months and spend close to $200 just to see if they’re a responder. Stick with it for years, and they could end up spending thousands. Some users find that as their results taper off, it no longer warrants the ongoing expense.
Note: the price of minoxidil can be dramatically reduced by purchasing in bulk and through big brands – like the minoxidil offered from Kirkland. But these formulations tend to come with propylene glycol and other carrier ingredients that can irritate the scalp.
Side Effects
The biggest side effect of minoxidil seems to be skin irritation. Between 2% to 6% of users report this.[11]https://www.researchgate.net/publication/221695328_Minoxidil_Use_in_Dermatology_Side_Effects_and_Recent_Patents However, allergy testing suggests that up to 80% of skin-irritation related side effects from minoxidil may not be caused by the minoxidil itself, but rather, a carrier ingredient called propylene glycol.[12]http://www.thaiscience.info/Journals/Article/JMAT/10986429.pdf
There are brands that offer minoxidil without propylene glycol, so be sure to check the labels if you have any concerns of allergies.
Additional side effects include toxicity to cats, under-eye bags, and potential heart palpitations. But these are all relatively rare.
Inconvenience
As hair growth treatments go, minoxidil is relatively easy and convenient. Still, not everyone wants to commit to twice-daily use for the rest of their lives, regardless of its effectiveness. And as we mentioned earlier, minoxidil alone is not an effective long-term treatment. To keep results from waning, using minoxidil in combination with other therapies is recommended, which only adds time and expense.
So if someone decides to stop taking minoxidil, what are the expectations?
What Happens When Stopping Minoxidil
In 1999, researchers conducted a study on the effects of abruptly ceasing minoxidil after long-term treatment.[13]https://www.jaad.org/article/S0190-9622(99)70006-X/fulltext Not only did the group who stopped minoxidil shed hair, but for a month or two, they actually crossed below the threshold of where they would have been if they’d never used minoxidil to begin with.
Let’s take a closer look at what happened.
The Study on Stopping Minoxidil
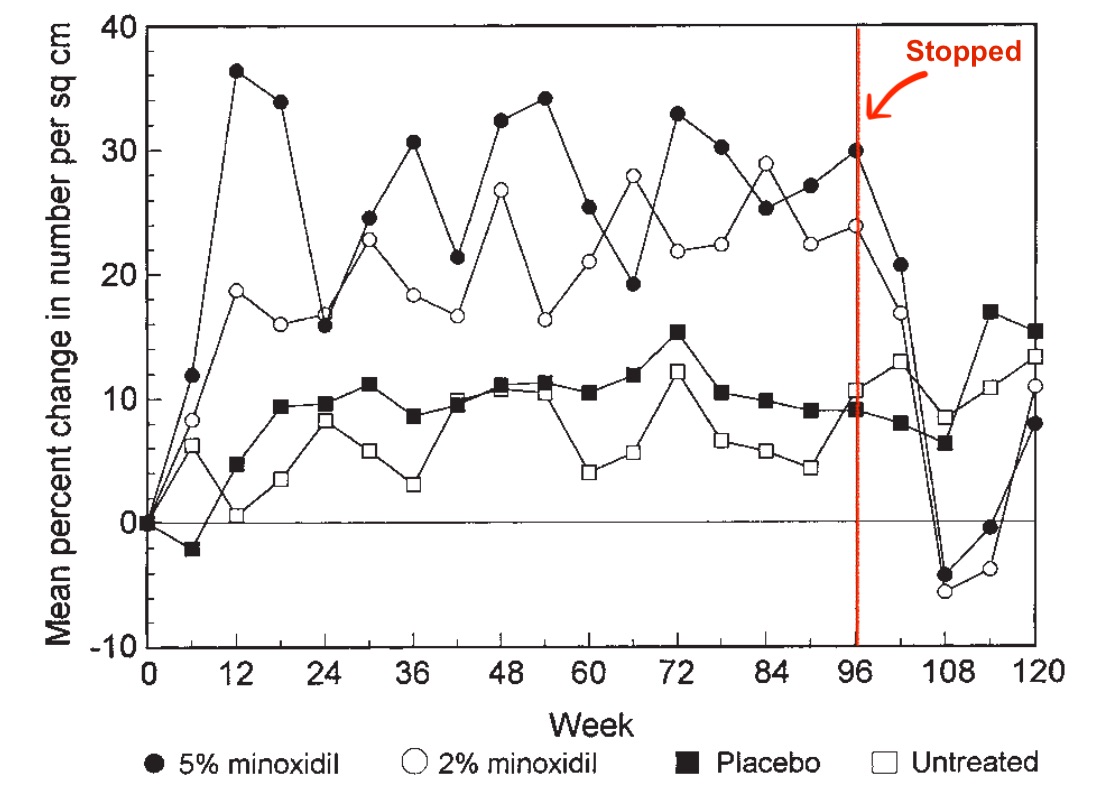
Researchers spent more than two years following four separate cohorts. One group was treated with 2% minoxidil, another group with 5%, one group was given a placebo, and the fourth group did nothing.
Both the 2% and 5% groups saw improvements in hair counts by the three-month mark. As we’ve said, these improvements leveled off a bit from that point forward but were still higher than hair counts in the placebo and control groups.
After almost two years of treatment, at the 96-week mark, the investigators took the people in the 2% and 5% minoxidil groups and discontinued treatment. We can see the exact moment this occurred by looking at the data on hair weights, which soon started decreasing.
Price, V. H., Menefee, E., & Strauss, P. C. (1999). Changes in hair weight and hair count in men with androgenetic alopecia, after application of 5% and 2% topical minoxidil, placebo, or no treatment. Journal of the American Academy of Dermatology, 41(5), 717–721.
Three months later, by week 108, their hair loss had dipped well below the placebo group and below where they were at the start of the study. Another three months after that, by week 120, both the 2% and 5% groups had rebounded to rejoin toss sufferers will end up right where they started.
As mentioned, any excess shedding should not be permanent, as hair will readjust to new homeostasis without the drug.
So the question becomes, is there a method to weaning from minoxidil that can prevent or reduce shedding?
Is Minoxidil Plus Microneedling the Answer?
In the above study, minoxidil was used as a monotherapy. And we know from the research that combining minoxidil with additional therapies, such as microneedling, can improve outcomes for non-responders and may prevent results from waning after the initial 3-6 months of usage.
So could microneedling also prevent (or delay) shedding if one decides to stop taking minoxidil? Let’s investigate what happens when we use these two therapies in tandem.
About Microneedling
Microneedling is a micro-wounding procedure that involves pricking the skin with tiny needles using either a roller or a pen-shaped tool. Studies have shown microneedling elicits growth factors, signaling proteins, and the enzymatic activity of Sulfotransferase, which we referred to earlier.
In some studies, Microneedling plus Minoxidil seems to elicit a fourfold greater effect on hair count increases than Minoxidil alone.[14]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746236/
In fact, when combining minoxidil with microneedling, new data show that all new hair gains might hold for much longer – even after quitting all treatments.
The Data on Combined Therapies
Let’s take a closer look at a 2020 study to see why microneedling could be the key to maintaining hair growth, even after quitting minoxidil.[15]https://pubmed.ncbi.nlm.nih.gov/29028377/
In the study, researchers split men into 3 groups. One treated their hair loss with minoxidil only, another group with microneedling only, and one group combined the two therapies. As other studies have shown, the combined therapies were significantly more effective in terms of hair growth.
But what the researchers did next was interesting. They stopped all treatments for each of the 3 groups, then brought them in 6 months later to ask, ‘how much hair growth did you retain, even in the absence of treatment?’ Here were their results:
- Minoxidil Only – 90% lost all new hair growth (just 10% retained new growth)
- Microneedling Only – 70% retained some new hair, 20% retained all new hair, 10% lost all new hair
- Combined Therapies – 70% retained some new hair, 20% retained all new hair, 10% lost all new hair
So the group that combined minoxidil with microneedling not only experienced at least twice the hair growth of the other two groups, but 70% of them held on to at least some of this new growth, even after stopping all treatments. And yet, before we conclude that microneedling plus minoxidil is a fail-safe method for maintaining hair growth after treatment ends, there are some possibilities to consider.
- It’s possible if researchers asked the same question 12 months versus 6 months later, all groups would report an equal amount of hair loss. We’ve seen with other therapies, Finasteride for example, that gains disappear over a longer timeline.
- While the number 70% sounds big, the sample size in this study was relatively small. Each group contained just 20 men. So, while it’s great that 14 men maintained at least some of their results for 6 months after treatment ended, it’s possible this percentage could change within a larger sample.
So, while the study above is promising, we don’t really have enough data to definitively say whether or not hair shedding after quitting minoxidil can be prevented.
We’ve yet to see any literature that would help predict who will or will not shed badly from minoxidil. However logically, it may be that those who respond better to minoxidil (or the more hair minoxidil helps one keep during use) simply have more hair to lose during withdrawal.
Anecdotally, about 50% of the male Perfect Hair Health members who have slowly weaned from minoxidil while maintaining microneedling therapy noticed no cosmetic differences in their hair counts afterward.
Basically, they’re able to maintain similar visuals even without the drugs. The other 50% do see a decline visually, but it’s nowhere near baseline or very rarely all the way back to baseline.
If hair loss sufferers do get to a point where they’re happy with their hair and want to wean away from drugs, doing so with the right tapering protocol while continuing the use of microneedling could be a solution.
The Best Way to Quit Minoxidil
When is the best time to call it quits? Never, if you’d like to take as much risk off the table as you can.
Otherwise, the following tips may help minimize any shedding related to minoxidil withdrawals.
- Start microneedling before quitting. Minoxidil and microneedling are synergistic treatments. Try them together for at least 3-6 months before dropping the drug.
- Don’t quit cold turkey. Follow a tapering protocol to minimize abrupt changes to the scalp environment. (We have a detailed weaning protocol in our membership.)
- Continue with alternative treatments. An effective weaning protocol takes up to 6 months. Continue with microneedling during this time.
- Replace minoxidil with natural therapies. Individuals may wish to experiment with other topicals instead, such as 2-5% rosemary oil.
For the most part, minoxidil requires lifelong use to hold onto any hair maintained or regrown. As such, shedding often occurs for 3-6 months following a stop in minoxidil application. But, we can significantly mitigate this shed by combining minoxidil with additional therapies and following a tapering protocol.
Summary
Minoxidil can be an effective treatment for androgenic alopecia, although research says when used alone, results taper off over time. Combining minoxidil with wounding therapies such as microneedling can make it more effective.
When stopping minoxidil, hair loss can be expected. Research shows losses will be greatest within the first 3-6 months of quitting but will eventually rebound to where hair counts would have been had minoxidil never been applied.
This doesn’t mean hair loss sufferers are stuck taking minoxidil for the rest of their lives. The same microneedling therapies that make minoxidil more effective may help sustain results after quitting the drug. This is especially true for those who commit to a strict tapering protocol versus quitting minoxidil cold turkey.
So should people use minoxidil?
For many, it’s worth a try. Some people will see visual improvements, some of which can be maintained with a proper weaning program. In the worst case, people will most likely end up where they would’ve been without treatment, but not worse off.
References[+]
References ↑1 https://www.jaad.org/article/S0190-9622(08)00809-8/abstract ↑2 https://pubmed.ncbi.nlm.nih.gov/9395721/ ↑3 https://www.jidonline.org/article/S0022-202X(15)42806-4/pdf ↑4 https://pubmed.ncbi.nlm.nih.gov/21524889/ ↑5 https://www.sciencedirect.com/science/article/pii/S019096229970006X ↑6 https://pubmed.ncbi.nlm.nih.gov/12196747/ ↑7 https://pubmed.ncbi.nlm.nih.gov/2180995/ ↑8 https://www.jaad.org/article/S0190-9622(08)00809-8/abstract ↑9 https://link.springer.com/article/10.1007%2Fs40257-018-0409-y ↑10 https://pubmed.ncbi.nlm.nih.gov/28078868/ ↑11 https://www.researchgate.net/publication/221695328_Minoxidil_Use_in_Dermatology_Side_Effects_and_Recent_Patents ↑12 http://www.thaiscience.info/Journals/Article/JMAT/10986429.pdf ↑13 https://www.jaad.org/article/S0190-9622(99)70006-X/fulltext ↑14 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746236/ ↑15 https://pubmed.ncbi.nlm.nih.gov/29028377/ Minoxidil is just one of two FDA-approved hair loss drugs. But FDA-approval doesn’t necessarily equate to guaranteed results with Minoxidil. In fact, many hair loss sufferers use minoxidil (i.e., Rogaine®) for six months and still don’t see significant benefits.
Why is that? In other words, why do 50% of people seem to respond favorably to minoxidil, while the remaining 50% see little-to-no benefit?
Research suggests this split in regrowth might be tied to an enzyme in the hair follicle called sulfotransferase.
Without coming into contact with sulfotransferase, Minoxidil won’t have an effect, and about 40% of men just don’t have enough sulfotransferase to elicit a response to Minoxidil.
Minoxidil is a pro-drug, meaning it has to be activated before it can exert its effects. Sulfotransferase plays an irreplaceable role in this because it turns minoxidil (its pro-drug form) into minoxidil sulfate (its active form).
We call this a rate-limiting step in the response rate to topical minoxidil, meaning the individual activity of the sulfotransferase enzymes on your scalp will predict your response rate to minoxidil.
This enzyme is also found in the liver. When oral minoxidil is ingested, it passes through these sulfotransferase enzymes, where it’s then distributed to the hair follicles throughout the body.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

When Can Responders Expect to See Visible Regrowth from Minoxidil?
Olsen, E. A., Dunlap, F. E., Funicella, T., Koperski, J. A., Swinehart, J. M., Tschen, E. H., & Trancik, R. J. (2002). A randomized clinical trial of 5% topical minoxidil versus 2% topical minoxidil and placebo in the treatment of androgenetic alopecia in men. Journal of the American Academy of Dermatology, 47(3), 377 385.
First, let’s talk about the event horizon for Minoxidil. With Minoxidil, results can be expected a little faster than Finasteride, so typically shedding is experienced between two and four months, but then re-growth is usually cosmetically perceptible around the one month to six-month mark. This makes sense, as Minoxidil acts more like a stimulant, or growth agonist.
Minoxidil turns more hairs on; it doesn’t necessarily target miniaturization. So Minoxidil doesn’t have as dramatic of an impact on reversing hair miniaturization and thereby improving hair thickness, but it can help to create a denser, fuller head of hair.
For those looking to reverse hair thinning, here are three ways to enhance the effectiveness of minoxidil treatment.
1. Acute Wound Generation via Microneedling
One of the easiest ways to enhance the efficacy of minoxidil is through acute wound generation, which is best administered through microneedling and massage.
Microneedling plus Minoxidil seems to elicit a four-fold greater effect of hair count increases than just Minoxidil alone.
Microneedling elicits growth factors, signaling proteins and enzymatic activity of sulfotransferase. Microneedling may also increase topical absorption and potentially even attenuate scarring – all of which pair well with minoxidil use.
Researchers started testing minoxidil + microneedling as a combination treatment back in 2013 – with incredible results.
One study showed over 12 weeks, minoxidil+ microneedling increased minoxidil efficacy four-fold and led to a 40% increase in hair count – with real, visual hair changes.[1]http://www.ijtrichology.com/article.asp?issn=0974-7753;year=2013;volume=5;issue=1;spage=6;epage=11;aulast=Dhurat
More recently, this study showed that over 6 months, minoxidil + microneedling had a 100% response rate and led to a 25% increase in hair count.[2]https://www.tandfonline.com/doi/abs/10.1080/14764172.2017.1376094?journalCode=ijcl20
It’s suspected that these improvements are due to microneedling’s ability to:
1 – Enhance skin enzymes required to activate minoxidil (i.e., sulfotransferase),
2 – Improve the absorbability of topicals like minoxidil – since the wounding allows for easier access to hair follicles and their blood supply, and
3 – Potentially attenuate or partially reverse fibrosis.
As with microneedling, Perfect Hair Health’s standardized scalp massages may help responders increase hair counts.
2. Switch to higher concentrations
Studies show that minoxidil non-responders see better hair growth after switching to 10% or 15% minoxidil. One such study was conducted on women with female pattern hair loss who were non-responders to 5% Minoxidil. They were trialed with 15% Minoxidil topically, and 70-80% of them saw a significant response. Participants saw an average of about 13% increase in hair counts.[3]https://clinicaltrials.gov/ct2/show/NCT02486848
So moving from 5% as a non-responder to 15% can really improve results.
Anecdotally, 15% Minoxidil is relatively safe. There’s not a ton of data on it, but when looking at the half-lives of Minoxidil, its transfusion into the system, and how much circulates from topical application, it doesn’t seem like there’s a massive uptake in the systemic volume of Minoxidil from going from 5% to 15%, at least from a biological perspective.
3. Add in topical retinol / retinoic acid
Another way to improve sulfotransferase activity? Using Tretinoin or Retinoic Acid. These are Vitamin A derivatives that help to activate sulfotransferase activity, stimulate a little bit of inflammation and cell turnover and in doing so, make minoxidil way more effective.
Topical minoxidil is delivered as a “pro-drug” – meaning that it is not technically active when it touches the scalp skin. Rather, minoxidil has to come into contact with an enzyme called sulfotransferase.
Unfortunately, many men and women don’t have enough sulfotransferase activity in the skin to elicit a major hair change with minoxidil alone. Fortunately, adding in topical retinol / retinoic acid can increase the activation of sulfotransferase, and thereby minoxidil – potentiating even bigger hair gains.
Just a few short years ago, hair loss sufferers had to ask their doctor to write a prescription for Vitamin A derivatives. There are brands online that sell combination formulas – like Happy Head, Adegen®, and MinoxidilMax. No doctor visit is required.
These companies sell products, but are these companies actually legitimate? Do their products actually contain the advertised ingredients? How do these formulas stand up to our rigorous lab tests? Join the Perfect Hair Health Membership Program to find out.
Summary
About 60% of people seem to be hyper-responders to Minoxidil. They see great hair count increases, and usually, they’ll see this in the first six months of treatment. Then those hair count increases will steadily decline over time. For the other 40% of people who try Minoxidil, there’s zero effect.
For high-responders, there is utility in taking a more multifactorial approach to Minoxidil treatment, where microneedling, high-concentration Minoxidil, and retinoic acid are combined to accelerate hair growth.
References[+]
Stool transplants – also known as fecal microbiota transplants (FMT) – are a controversial therapy reserved for life-threatening bacterial infections and autoimmune disorders. Fascinatingly, people who’ve undergone stool transplants have later reported unintended benefits: weight loss, less acne, personality improvements, and even hair regrowth.
At face value, a connection between stool transplants and hair loss sounds like science fiction. How could altering the bacteria inside of our guts affect hair growth on top of our scalps?
At the same time, new research suggests that the hair loss-fecal microbiota connection is very real, and may even become a future therapeutic target for people looking to regrow hair.
In this article, we’ll dive into the science surrounding stool transplants: what this therapy is, what it does to our gut microbiome, and the evidence linking fecal microbiota transplants to hair regrowth in alopecia areata, telogen effluvium, and maybe even androgenic alopecia.
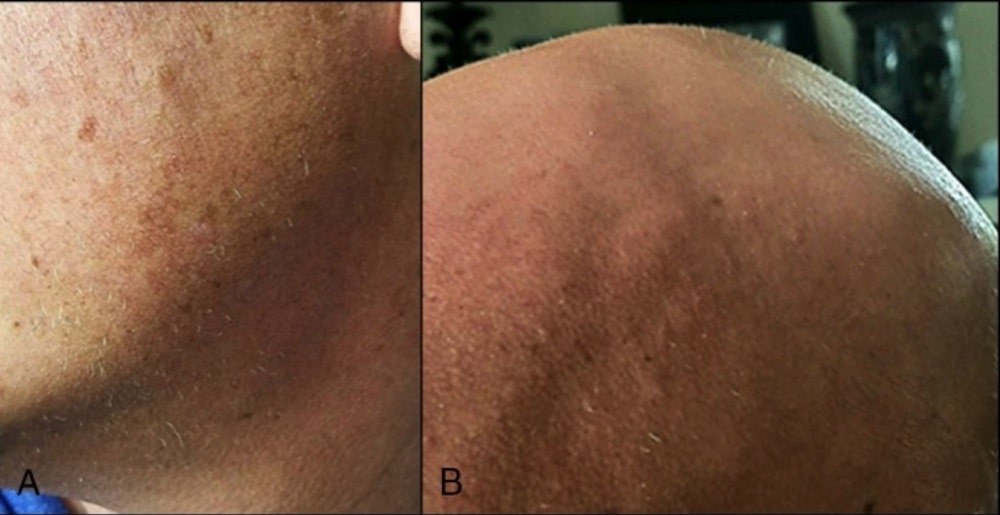
We’ll even showcase a few before-after photos featured in studies and forums from people who received stool transplants to treat unrelated health conditions, and ended up (accidentally) experiencing hair regrowth.
If you have any questions, feel free to reach us in the comments below.
Table of contents
All-Natural Hair Supplement + Topical
The top natural ingredients for hair growth, all in one serum & supplement.
Take the next step in your hair growth journey with a world-class natural serum & supplement. Ingredients, doses, & concentrations built by science.

What is a fecal microbiota transplant (i.e., stool transplant)?
Our guts are like a storage facility for large colonies of microbes. Because of the role the gut microbiome encompasses, many diseases and conditions that relate to a dysfunctional gut microbiome, have now been treated utilizing a fecal microbiota transplant.
An artist’s rendering of gut organisms and debris
A fecal microbiota transplant (FMT) is basically what it sounds like: the transfer of stool from one individual’s colon into another person. The aim? To improve gut bacteria density and diversity. In other words: increase the total number of “good” bacteria in the gut, as well as the number of “good” species.
Stool transplants – or FMTs – are nothing new. This practice has been around since the 4th century. More recently, it gained notoriety when the FDA approved FMTs for recurrent Clostridium difficile infections – a deadly bacterial infection that often grows resistant to antibiotics [1].
In this context, FMT’s are incredibly successful. For a benchmark, antibiotic treatments for C. difficile tend to boast a 20-30% remission rate. FMTs boast around a 90% remission rate [2]. In the veterinary world, FMT’s are used for similar purposes [3].
While the use of a FMT seems most pertinent to gastrointestinal diseases, there is a much broader spectrum for the therapy in relation to other conditions, such as multiple sclerosis, Alzheimer’s disease, epilepsy, obesity, and metabolic syndrome (to name only a few) [4, 5].
Can fecal microbiota transplants alter our gut microbiome?
FMTs are perhaps one of the most powerful ways to alter our gut microbiome: the collection of bacteria inside our intestines that help regulate anything from autoimmune reactions to hormonal levels to nutrient metabolism.
C. difficile & stool transplants: alterations to gut flora
In one study, researchers decided to investigate 55 stool samples from donors and recipients who used FMTs as a treatment for C. difficile infections. They found major differences in the pre- versus post-procedure samples of the recipients [6].
Before the procedure, healthy donors’ stools contained a significant portion of the phylum of bacteria – known as Firmicutes and Bacteroides – constituting roughly 85% of bacteria identified.
We can first think of a phylum as the link between different species of bacteria. For example, while an oak tree differs from a palm tree, ultimately, they’re still all trees. As such, no one group can be labeled as good or bad as often the species within those groups can exhibit both helpful and disruptive properties. This is evident with helminth infections – where the same helminth can cause inflammation in the first-world but protect from malaria in the developed world. To put it simply: the effects of a bacteria often rely on its environment, the health of an individual, the ratio of that bacteria to others, and about a billion other factors [7,8].
However, in the case of resistant Clostridium infections, Firmicutes and Bacteroides tend to be absent. This suggests that these phylum may play a role in preventing gut dysbiosis and thereby C. difficile overgrowths.
With respect to the study, here’s what researchers found:
- Prior to the stool transplants, recipients’ stools had lower amounts of Firmicutes and Bacteroides and markedly high Fusobacteria and Proteobacteria.
- Donor stool contained exceptionally higher Firmicutes and Bacteroides, as well as lower Fusobacteria and Proteobacteria.
- After treatments, recipients’ stool showed the higher Firmicutes and Bacteroides as well as lower Fusobacteria and Proteobacteria (thereby more closely resembling that of the donor’s gut).
- After transplantation, the more closely a recipient’s gut matched that of its donor, the more likely that recipient was to experience a remission from C. difficile.
In other words, FMTs significantly altered gut flora – and to the benefit of sick patients.
Interestingly, the health of our gut microbiome is linked to many hair loss disorders – particularly alopecia areata and telogen effluvium. Moreover, research now links gut bacteria to the regulation of DHT – the hormone implicated in pattern hair loss.
We’ll dive into this evidence below: what it is, what it means, and why it might rewrite a lot of what we think we know about hair loss.
Stool transplants for hair loss: the evidence
When it comes to FMTs as a treatment for hair loss, evidence is very limited. This is because reports of fecal transplants and hair regrowth have mainly happened by accident – specifically, after a patient with C. difficile + hair loss receives a stool transplant and later inadvertently sees improvements to both conditions.
Nonetheless, there is compelling evidence of a gut microbiome-hair loss connection. To best outline this evidence, we’ll dive into the research on FMT’s and hair loss as organized by :
- Alopecia Areata
- Telogen Effluvium
- Androgenic Alopecia
Let’s begin.
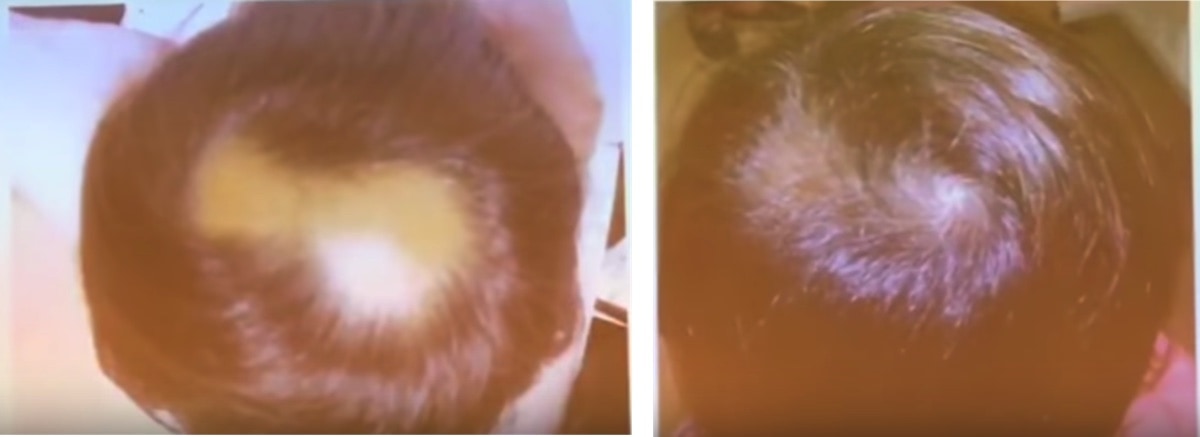
Alopecia areata and fecal microbiota transplants
Alopecia areata (AA) is an autoimmune form of hair loss; it often presents as patchy-related hair loss in the scalp. Researchers currently believe AA is the result of a collapse in “immune privilege” of the hair follicles – whereby the immune system begins to read hair follicles as foreign invaders, and then starts to attack them.
Alopecia areata: patchy hair loss
When it comes to stool transplants, alopecia areata is the best-studied form of hair loss. This isn’t saying much – because there’s not a ton of data on stool transplants and hair regrowth in general. Again, the studies here have been unintended and inadvertent: people with alopecia areata seem to have higher rates of gut dysbiosis, and thereby they seem to suffer disproportionately from infections like C. difficile. Therefore, they’re probably more likely to eventually become eligible for extreme treatments like a stool transplant – which is why we have case reports of FMTs and AA-related regrowth in the first place.
So, what limited evidence do we have on stool transplants for hair regrowth from alopecia areata?
Case reports of FMTs and hair regrowth from alopecia areata
Study #1: two uncontrolled retrospective case reports
In a study where two patients received an FMT for treating Clostridium difficile, researchers reported that both people saw an unintended benefit of hair regrowth following the procedure [14]. In these cases, both patients were classified as having alopecia universalis – an advanced form of alopecia areata where the hair loss has progresses beyond the scalp and to the body.
In the first case, the 38-year old man began to grow peach fuzz not only on his head, but also his face and arms. The regrowth became cosmetically noticeable 8 weeks after the stool transplant – after having suffered from progressive alopecia universalis for decades without any improvements.
In the second case, a 20-year old man – diagnosed with alopecia universalis 2 years prior to his FMT – saw major improvements to scalp hair regrowth over a 1.5-year period after receiving a stool transplant. Prior to the FMT, this subject had tried to treat his alopecia using corticosteroid injections, topical steroids, squaric acid, and laser treatments— all to no avail. While this man also received steroid injections within his scalp after the FMT, he began to grow hair throughout the rest of his body as well, even where had not received a steroid injection [21].
Study #2: a case report of FMT + hair regrowth in an elderly patient with diffuse alopecia areata
In a second study investigating FMT’s effects on an elderly man (86-year old) with diffuse alopecia areata, researchers found some unexpected benefits [15]. Originally, FMT was used to treat his intestinal disorders (with success). However, alongside the treatment of his other digestive ailments, his hair thickness began to return. What’s more, his previously gray hair had regrown as its original color.
These are just three case reports. That’s not really “overwhelming” evidence…
You’re right! We always have to evaluate any intervention in respect to its quality and quantity of evidence. In regard to FMT and alopecia areata, the quality and quantity of evidence is low: three uncontrolled, retrospective case reports.
Having said that, we also have to recognize that the total number of alopecia areata patients who (1) develop C. difficile, and (2) have it progress to the severity where they become eligible for an FMT – is also low. On that note, the evidence here has excited other research teams enough to launch a clinical trial on FMT and alopecia areata – the results of which will (hopefully) be available in the coming year.
So, needless to say, the preliminary evidence (and mechanistic data) supporting a connection between is FMT and AA-related regrowth is exciting enough to continue exploring.
How might FMT’s improve alopecia areata?
Alopecia areata is mainly categorized by an autoimmune attack on the hair follicles. This is predominantly mediated by a group of immune cell known as T-cells. Specifically, a type of T-cell known as TH17 [16].
Not surprisingly, TH17 is a major contributor to intestinal conditions that manifest as inflammation. Since the gut is our largest site of immune cell concentration, then by altering the gut microbiome to a more favorable anti-inflammatory profile, we may be able to alter T-cell activity throughout the rest of our body.
In fact, studies have shown that modulating the microbiome to favor this anti-inflammatory profile can nearly shutdown TH17 cell activity [17]. By this very same mechanism, it is possible that a more widespread shutdown of TH17 could alleviate a TH17-mediated attack on hair follicles – even at the top of the scalp.
Furthermore, there is an established link between inflammatory bowel disease and alopecia areata [18]. The implication: an unhealthy microbiome may drive both inflammatory bowel disease and alopecia areata. After all, patients with alopecia areata and inflammatory bowel conditions who undergo FMT seem to inadvertently regrow hair – and at a consistency worth noting by investigators.
Summary so far: Alopecia areata (AA) is an autoimmune form of hair loss; it’s likely driven by the over-activation of T-cells, and specifically, TH17 cells. Interestingly, patients with AA who’ve undergone stool transplants (FMTs) to treat C. difficile infections have inadvertently regrown hair. The gut microbiome is the body’s largest site of immune cell concentration – and thereby TH17 activation. So, it’s plausible that FMTs might dampen TH17 immune activation – all by restoring gut microflora balance to a more commensal state.
Telogen effluvium and stool transplants
Telogen effluvium (TE) is a temporary form of hair loss that is characterized by a dysregulation of the hair cycle.
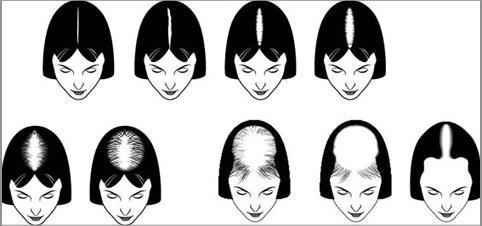
This can occur in many ways: for instance, too many hairs can “shed” prematurely, or there can be a delay between when a hair sheds out and when a new hair grows in (to start a new hair cycle). This often presents as diffuse thinning, or sometimes even region-specific shedding (oftentimes the hairline for women).
A hair loss patient with suspected telogen effluvium (TE)
What causes telogen effluvium (TE)?
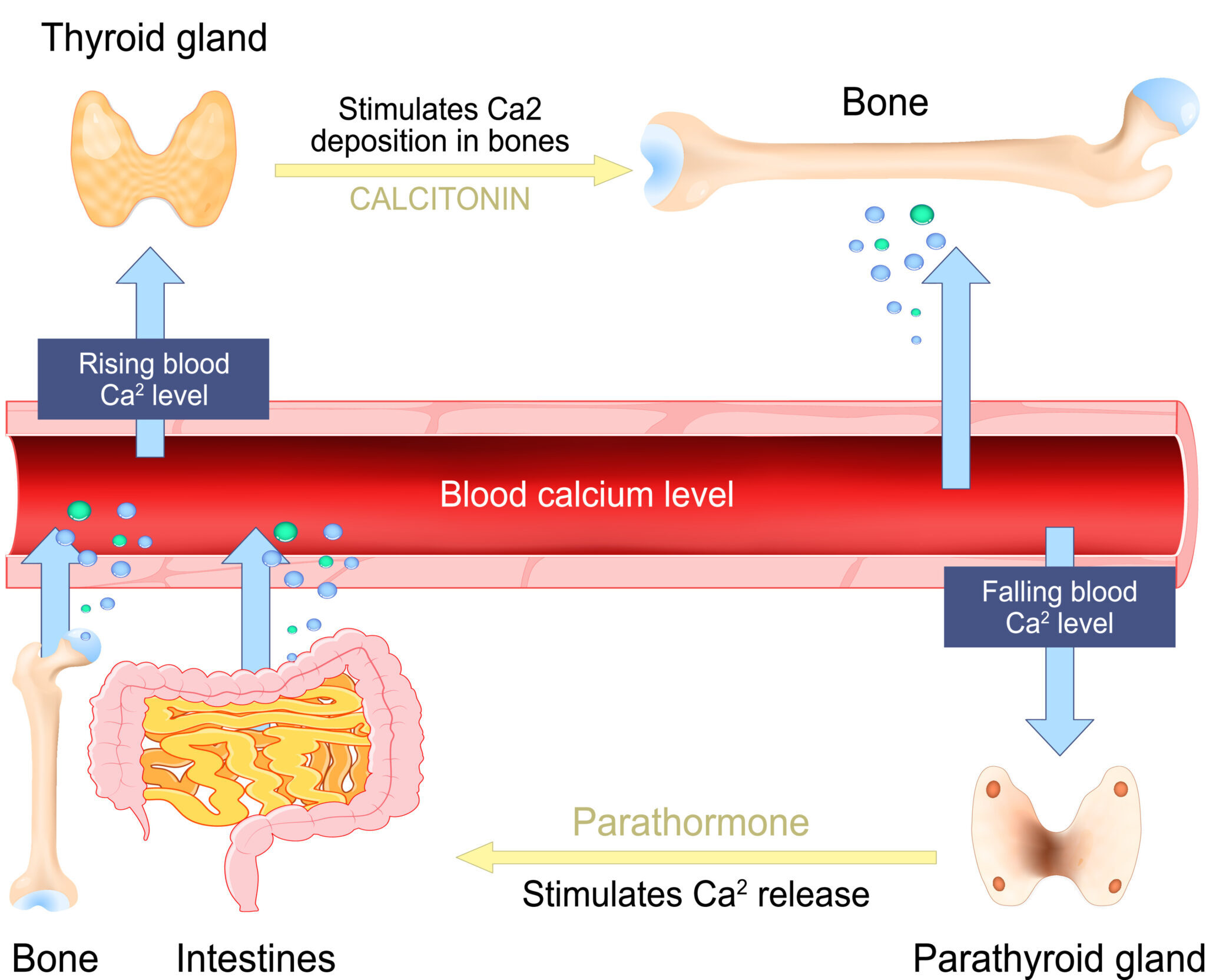
Telogen effluvium (TE) is sort of like a catch-all diagnosis for a wide array of hair loss triggers. But the main drivers of TE are often considered (1) stress (emotional or physical), (2) nutrient imbalances, and (3) chronic conditions (i.e., hypothyroidism, heavy metal toxicities, etc.).
Currently, there are no studies investigating a link between FMTs and TE. However, there is mechanistic evidence that FMTs may help address some (of the many) underlying factors leading to TE.
For example, nutrient deficiencies – namely, iron, zinc, and/or vitamin D – have been associated with telogen effluvium [20]. Given that evidence implicates the state of the microbiome in nutrient absorption, it’s possible that disruptions to the microbiome may result in poor nutrient absorption and, consequently, telogen effluvium-related hair shedding [21].
Research has also found elevated cadmium levels in some people with TE – a trace element that may trigger hair shedding if consumed in excness [22]. Most interesting, though, is that excessive cadmium has also been shown to alter the gut microbiome of mice in a way that directly mirrors individuals plagued by antibiotic-resistant Clostridium difficile infections… the exact condition FMT is designed to treat [23].
Altogether, direct (i.e., by bacterial infection) or indirect (i.e., by excess cadmium) changes to the microbiome, both of which seem to be associated with telogen effluivum, may benefit from FMT.
Summary so far: Telogen effluvium (TE) is a temporary form of hair loss caused by a disruption to the hair cycle – oftentimes resulting from stress, nutrient imbalances, or a chronic condition. While no evidence directly implicates stool transplants as a therapeutic procedure for TE, there is mechanistic data showing that our gut microbiome has the capacity to improve chronic conditions as well as the synthesis of vitamins commonly found as deficient in TE patients. Therefore, it’s possible that stool transplants might help TE by addressing its underlying causes. But again, we’re extrapolating here!
Androgenic alopecia and fecal transplants
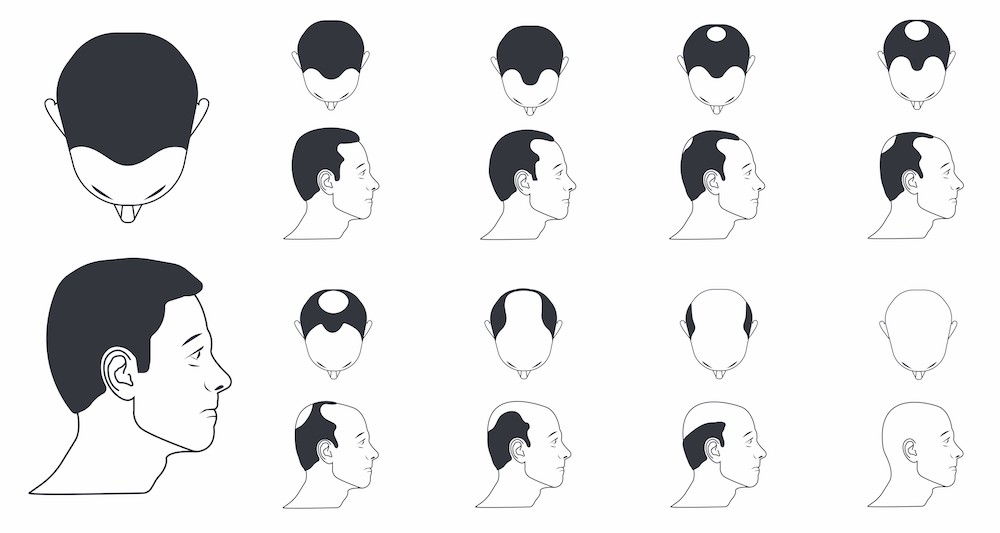
Androgenic alopecia (AGA) is one of the world’s most common hair loss disorders – affecting at least 50% of women and 80% of men throughout a lifetime. Its often characterized by progressive hair follicle miniaturization, whereby affected hair follicles get thinner and thinner over a series of hair cycles. It presents most commonly across the top of the scalp as temple recession + a bald spot in men, and diffuse thinning in most women.
Androgenic alopecia in a male: temple recession
What causes androgenic alopecia (AGA)?
While all of the causes aren’t fully elucidated, most researchers agree that AGA is caused by a combination of male hormones and genetics, and possibly the scalp’s environment (i.e., inflammatory microorganisms, the contraction of muscles surrounding the scalp perimeter, inflammation-mediated tension, etc.).
Specifically, the hormone dihydrotestosterone (DHT) seems to overexpress in balding scalp regions. In vitro studies demonstrate that DHT may trigger premature shedding, inflammatory signaling proteins, and cell death in dermal papillae cells (the “powerhouse” of the hair follicle) – all of which can lead to progressive hair follicle miniaturization. Moreover, studies have shown that men without DHT do not go bald, and that reducing DHT can help prevent (and partially reverse) the balding process.
Is there evidence that stool transplants can improve pattern hair loss (AGA)?
Clinical evidence? No. Mechanistic evidence? Yes. Anecdotes of AGA improvements after stool transplants? Yes – even with photos. We’ll uncover all of this below.
First, to our knowledge, no case reports or clinical trials investigating the benefits of FMT have occurred. Nonetheless, the absence of evidence doesn’t imply evidence against a therapy (remember: FMTs are a very limited intervention). On that note, there are anecdotes online of people with AGA regrowing their hair (accidentally) following a fecal transplant.
One anecdote comes from a male forum user who suffered simultaneously from both irritable bowel syndrome (IBS) and AGA. In the past, he’d tried to treat his AGA with finasteride. Unfortunately, he did not see any improvements, so he stopped using the drug.
In search for a way to improve his IBS, he later stumbled upon the evidence supporting fecal microbiota transplants to treat C. difficile, Crohn’s disease, and gut dysbiosis. His symptoms were severe enough that he ended up tracking down a willing practitioner and giving the therapy a try – potentially outside of legal means.
A week after the therapy, he reported that his hair shedding dramatically decreased. A year later, he reported significant hair thickening (and potential regrowth)… regrowth that occurred outside of any drug interventions or hair growth therapies.
AGA-related hair regrowth one-year after a stool transplant
This anecdote is promising. But again, it’s just the experience of one person. Beyond this report, are there any other examples?
When it comes to fecal microbiota transplants – we couldn’t find any other anecdotes of hair regrowth from AGA. But interestingly, we were able to find reports of hair regrowth (with photos) from people adhering to incredibly restrictive diets that completely revamp gut microflora constitutions.
One such diet is the carnivore diet – whereby someone nearly completely restricts carbohydrate and fiber intake and begins to subsist entirely off of meat. It sounds like a crazy diet (and it just might be). However, it’s also the only diet where I’ve actually seen people regrow hair lost due to androgenic alopecia. For instance:
- A 1928 case report detailed two men under clinical observation for an entire year while eating only meat. One observation from the investigation team? One of the men saw a complete stop in the progression of his pattern hair loss.
- Some members of our community (who have failed to see success with drugs like finasteride) have later opted to adopt the carnivore diet as an experiment for health. A few of these members have reported hair regrowth.
For an example – take Brian (a member of our community). He’d tried finasteride for two years, saw zero improvements, and then eventually quit the drug. Later, he and his wife decided to try the carnivore diet. Simultaneously, he also started to incorporate our scalp massages to see if that would improve his hair loss (since finasteride didn’t work).
One year later, he’d noticed significant hair regrowth at hairline, as well as overall hair thickening. Here were his results.
AGA-related hair regrowth one-year after the carnivore diet + massaging
Interestingly, preliminary evidence suggests that the carnivore diet may increase gut microorganism biodiversity – one of the objectives of FMT. It may also reduce the totality of bacteria inside the gut – since these microorganisms feed off carbohydrate and fiber (two things that are nearly eliminated on a diet consisting of all meat).
Moreover, the carnivore diet eliminates a lot of inflammatory food groups (i.e., FODMAPs) that might contribute to systemic inflammation for sensitive individuals. This may help reduce the number of pathogenic bacteria residing in the gut, as well [27].
This leads to some interesting discussion points about a possible connection between AGA, stool transplants, the carnivore diet, and subsequent changes to the microbiome that could improve hair loss outcomes. We’ll explore these below.
Mechanisms: how might stool transplants improve pattern hair loss?
There’s evidence that our microbiome may help regulate our endocrine system (i.e., the balance of our sex hormones). More specifically, our microbiome may play a direct role in the metabolism of androgens – the sex hormone implicated in AGA.
To start, here’s a quick overview on how hormone metabolism works:
- Once circulating hormones have “completed” a task, they reach the liver. The liver is where free hormones (i.e., the active, unbound hormones) in our blood are processed to later become excreted.
- The liver conjugates these free hormones. Simply put, the livers converts the structure of these hormones from lipophilic (i.e., fat-loving) to hydrophilic (i.e., water-loving). This does two things: it makes the hormone less potent, and it increases that hormone’s chances of entering the digestive tract (i.e., small and large intestine) where they can get excreted.
- Once these conjugated forms of hormones enter the digestive tract, the body excretes these conjugates or metabolites in the stool and urine.
Put simply, our liver conjugates active hormones, those hormones enter our digestive tract, then our digestive tract flushes those hormones out of the body.
But here is where things get interesting: some of our gut bacteria produce an enzyme called beta-glucuronidase. This enzyme has the ability to reverse the process of hormone excretion. Specifically, when conjugated forms of hormones come into contact with beta-glucuronidase, those hormones become unconjugated. In other words, they reconvert back into an active (i.e., unbound) form – where they can potentially reenter our circulatory system.
So, if gut bacteria have the ability to act as gatekeepers for hormone excretion and reabsorption, what does this have to do with AGA?
Fascinatingly, research in healthy men has demonstrated that free dihydrotestosterone (DHT) – the hormone implicated in AGA – exists at levels in the colon at levels 70-fold higher than free DHT found in the blood [24].
This suggests (at least) two things:
- Serum levels of DHT represent just a tiny fraction of total DHT within our body.
- If this free DHT can exit the digestive tract and reenter the circulatory system, this means that gut bacteria might act as a gatekeeper for androgen excretion / reabsorption… and that our microflora might be directly implicated in androgenic-linked conditions: heart disease, prostate enlargement, and maybe even pattern hair loss.
It’s already been shown that gut bacteria have a directly influence on steroid levels. In fact, in the case of periodontal disease and gingivitis, certain cultured bacterial species can actually increase levels of testosterone and DHT [25]. Moreover, researchers have linked this increase to the development of inflammation in periodontitis itself.
Free DHT (as opposed to conjugated DHT) is the type of DHT that likely elicits the majority of DHT-mediated effects on the body. This includes supporting the processes that lead to AGA. You can learn more about this here.
Can unconjugated DHT (in the gut) reenter the circulatory system?
No studies have demonstrated this. But to our knowledge, no studies have actually asked this question (to our knowledge). Not to sound like a broken record, but the absence of evidence cannot imply evidence against something.
It’s worth noting that gut bacteria can produce (and recirculate) estrogens. So, it’s not out of the realm of possibilities that DHT can also be recirculated. In fact, it’s more likely than not.
Moreover, studies on patients with post-finasteride syndrome (long-lasted sexual dysfunction and/or cognitive disorders after cessation of finasteride) show marked gut microbiota alterations [26]. Researchers believe that these microbiota alterations may possibly contribute to the symptoms of finasteride syndrome.
Of course, there are still no clear connections between post-finasteride syndrome and these microbiome alterations. However, if free DHT levels in the colon contribute to overall DHT levels and finasteride results in prolonged changes to the population of these bacteria, it’s possible that reduced colon DHT may contribute to blood DHT, and, thereby the symptoms of post-finasteride syndrome.
Similarly, the opposite could also prove true: if colonic DHT influences blood DHT levels (in an upwards or downwards direction), then anything that increases the total number of our gut bacteria might also increase DHT levels.
Whether this affects scalp DHT (and thereby AGA) – we just don’t know. But we do find these anecdotes of stool transplants and/or carnivore diets regrowing hair absolutely fascinating. After all, both interventions likely lead to improvements in gut biodiversity and changes to the total number of commensal / pathogenic microflora. Therefore, they likely alter DHT activity in the gut. But whether these effects extend to our scalp hair – we can’t yet say (aside from admiring those before-after photos and “hoping” that, after all these years, it’s just that easy to reverse AGA).
Summary so far: Androgenic alopecia (AGA) is driven by a combination of genes and androgens. Interestingly, some patients who’ve undergone stool transplants have later reported hair thickening from AGA without any other treatments. The main hormone implicated in AGA is dihydrotestosterone (DHT). Recent research has found that gut bacteria can actually produce DHT, and even convert it from an inactive to active form. Moreover, researchers recently discovered that free DHT is found in stool samples at levels 70-fold greater than in the blood supply. It has been demonstrated that gut microorganisms influence estrogen production, and the amount of estrogen circulating in our blood. Therefore, it’s not unreasonable to assume that gut flora may also act as gatekeepers for DHT activation between the gut and the circulatory system. If true, this may directly implicate gut bacteria in the pathogenesis of AGA.
Fecal microbiota transplants: undergoing the procedure
What’s it like to do a fecal microbiota transplant?
While FMT may sound like a cure-all for all autoimmune ailments, it’s worth mentioning that research here is still in its infancy, and there’s always the very real possibility that a transplant won’t work or might worsen your symptoms due to unforeseen interactions between donor and recipient microflora.
In the US and Europe, strict guidelines are set to screen a potential donor for any negative attributes that could trigger unwanted side effects for the recipient. There is a questionnaire that is given, stool sample analysis is performed approximately four weeks prior, and blood samples taken [1], followed by an additional interview at the time of the donation. Preferably, you would want a stool sample from someone close to you, with whom you may have shared a common environment. This reduces the chances of any unwanted immune reactions that may occur.
Any failure in the proper preparation of the FMT can present with complications such as bacteremia (i.e., bacteria in the bloodstream) or hospitalizations. Other mishaps such as perforations can occur, but tend to be attributed to the tools and technicians rather than infectious agents [10].
Usually, preparations of the fecal material are done up to six hours before the procedure. The sample is frozen, then thawed out, and, finally mixed with a solution to deliver in a syringe.
It’s also been shown that the size of the sample matters dramatically. Usually, sample sizes are around 50g, which is no more than a few teaspoons. With difficult to treat clostridium infections, larger sample sizes have demonstrated better efficacy and reduced chances chances of failure with the treatment [11]. Many times, FMT requires multiple treatment sessions as well for optimal results.
An important (and interesting) aspect of the procedure is the fact that antibiotics are not to be given to the recipient within 48-hours [12]. While this may seem like an obvious aspect of FMT, this also points to the possibility that it actually is the bacteria present within the stool itself that produces results… not another confounding variable such as immune molecules, proteins, or other components.
Even more supportive of that notion: studies have shown when the procedure is given to the lower digestive tract, (which is also where a majority of the gut microbiome resides), results are drastically better than when administered in the upper digestive tract [1].
Is there a way around the “yuck factor” of FMT?
The idea of taking someone else’s fecal material and implanting it inside of your colon isn’t exactly appealing. And while a lot of the hesitancy is likely psychological, it’s reasonable to ask if there’s a way to do an FMT without doing an enema.
Yes. Researchers have shown that oral capsules produced results on par with the procedure itself – at least in the treatment of resistant Clostridium infections [13]. Obviously, oral supplementation may come across as even less appealing to some. Tto others, the possibility of supplementation certainly reduces the “barrier to entry”.
Summary: stool transplants for hair loss
By regulating the gut microbiome and reducing gut inflammation, a fecal microbiota transplant may improve hair loss outcomes for alopecia areata, telogen effluvium, and perhaps even androgenic alopecia.
Evidence on stool transplants and hair regrowth is incredibly limited. Our knowledge base comes from:
- Four case reports demonstrating significant hair regrowth across patients with autoimmune forms of hair loss
- Anecdotes from people who’ve undergone stool transplants for gut dysbiosis and later reported inadvertent hair regrowth
- Mechanistic data revealing possible connections between stool transplants, the gut microbiome, DHT production, and immunological changes – as well as their overlap with common hair loss disorders.
Nonetheless, I personally find this arena of research fascinating, and I hope it rapidly expands.
In the meantime, please note that we’re not recommending stool transplants as a first-line of defense for any hair loss disorder. If you’re interested in getting one, you’ll need to connect with a qualified physician – we’re not in a position to help you here.
You can reach us in the comments any time!
References
- Wang, J.-W., Kuo, C.-H., Kuo, F.-C., Wang, Y.-K., Hsu, W.-H., Yu, F.-J., … Wu, D.-C. (2018). Fecal microbiota transplantation: Review and update. Journal of the Formosan Medical Association. doi:10.1016/j.jfma.2018.08.011
- van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG,de Vos WM, et al. Duodenal infusion of donor feces for recur-rent Clostridium difficile.N Engl J Med2013;368:407e15.
- Pereira GQ, Gomes LA, Santos IS, Alfieri AF, Weese JS, Costa MC. Fecal microbiota transplantation in puppies with canine parvovirus infection. J Vet Intern Med. 2018 Mar;32(2):707-711. doi: 10.1111/jvim.15072. Epub 2018 Feb 20. PMID: 29460302; PMCID: PMC5867004.
- [Vendrik, K., Ooijevaar, R. E., de Jong, P., Laman, J. D., van Oosten, B. W., van Hilten, J. J., Ducarmon, Q. R., Keller, J. J., Kuijper, E. J., & Contarino, M. F. (2020). Fecal Microbiota Transplantation in Neurological Disorders. Frontiers in cellular and infection microbiology, 10, 98. https://doi.org/10.3389/fcimb.2020.00098
- Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JF, Dallinga-Thie GM, Ackermans MT, Serlie MJ, Oozeer R, Derrien M, Druesne A, Van Hylckama Vlieg JE, Bloks VW, Groen AK, Heilig HG, Zoetendal EG, Stroes ES, de Vos WM, Hoekstra JB, Nieuwdorp M. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012 Oct;143(4):913-6.e7. doi: 10.1053/j.gastro.2012.06.031. Epub 2012 Jun 20. Erratum in: Gastroenterology. 2013 Jan;144(1):250. PMID: 22728514.
- Yoon H, Shim HI, Seol M, Shin CM, Park YS, Kim N, Lee DH. Factors Related to Outcomes of Fecal Microbiota Transplantation in Patients with Clostridioides difficile Infection. Gut Liver. 2021 Jan 15;15(1):61-69. doi: 10.5009/gnl20135. PMID: 32839363.
- Leimbach A, Hacker J, Dobrindt U. E. coli as an all-rounder: the thin line between commensalism and pathogenicity. Curr Top Microbiol Immunol. 2013;358:3-32. doi: 10.1007/82_2012_303. PMID: 23340801.
- Renga G, Bellet MM, Stincardini C, Pariano M, Oikonomou V, Villella VR, Brancorsini S, Clerici C, Romani L, Costantini C. To Be or Not to Be a Pathogen: Candida albicans and Celiac Disease. Front Immunol. 2019 Dec 5;10:2844. doi: 10.3389/fimmu.2019.02844. PMID: 31867008; PMCID: PMC6906151.
- Flannigan, K. L., Rajbar, T., Moffat, A., McKenzie, L. S., Dicke, F., Rioux, K., Workentine, M. L., Louie, T. J., Hirota, S. A., & Greenway, S. C. (2017). Changes in Composition of the Gut Bacterial Microbiome after Fecal Microbiota Transplantation for Recurrent Clostridium difficile Infection in a Pediatric Heart Transplant Patient. Frontiers in cardiovascular medicine, 4, 17. https://doi.org/10.3389/fcvm.2017.00017
- [Dailey, F. E., Turse, E. P., Daglilar, E., & Tahan, V. (2019). The dirty aspects of fecal microbiota transplantation: a review of its adverse effects and complications. Current Opinion in Pharmacology, 49, 29–33. doi:10.1016/j.coph.2019.04.008
- Cammarota, G., Ianiro, G., Tilg, H., Rajilić-Stojanović, M., Kump, P., Satokari, R., Sokol, H., Arkkila, P., Pintus, C., Hart, A., Segal, J., Aloi, M., Masucci, L., Molinaro, A., Scaldaferri, F., Gasbarrini, G., Lopez-Sanroman, A., Link, A., de Groot, P., de Vos, W. M., … European FMT Working Group (2017). European consensus conference on faecal microbiota transplantation in clinical practice. Gut, 66(4), 569–580. https://doi.org/10.1136/gutjnl-2016-313017
- William M. Tauxe, MST, Tanvi Dhere, MD, Angela Ward, MSN, FNP, Lori D. Racsa, DO, Jay B. Varkey, MD, Colleen S. Kraft, MD, MSc, Fecal Microbiota Transplant Protocol for Clostridium Difficile Infection, Laboratory Medicine, Volume 46, Issue 1, Winter 2015, Pages e19–e23, https://doi.org/10.1309/LMCI95M0TWPDZKOD
- Kao D, Roach B, Silva M, Beck P, Rioux K, Kaplan GG, et al.Effect of oral capsule- vs colonoscopy-delivered fecal micro-biota transplantation on recurrent Clostridium difficile infec-tion: a randomized clinical trial.JAMA2017;318:1985e93.
- Rebello, D., Wang, E., Yen, E., Lio, P. A., & Kelly, C. R. (2017). Hair Growth in Two Alopecia Patients after Fecal Microbiota Transplant. ACG case reports journal, 4, e107. https://doi.org/10.14309/crj.2017.107
- [Xie, W. R., Yang, X. Y., Xia, H. H., Wu, L. H., & He, X. X. (2019). Hair regrowth following fecal microbiota transplantation in an elderly patient with alopecia areata: A case report and review of the literature. World journal of clinical cases, 7(19), 3074–3081. https://doi.org/10.12998/wjcc.v7.i19.3074
- Loh SH, Moon HN, Lew BL, Sim WY. Role of T helper 17 cells and T regulatory cells in alopecia areata: comparison of lesion and serum cytokine between controls and patients. J Eur Acad Dermatol Venereol. 2018 Jun;32(6):1028-1033. doi: 10.1111/jdv.14775. Epub 2018 Jan 17. PMID: 29283462.
- [Pandiyan, Pushpa & Bhaskaran, Natarajan & Zou, Mangge & Schneider, Elizabeth & Jayaraman, Sangeetha & Huehn, Jochen. (2019). Microbiome Dependent Regulation of Tregs and Th17 Cells in Mucosa. Frontiers in Immunology. 10. 426. 10.3389/fimmu.2019.00426.
- Maghfour J, Olson J, Conic R, R, Z, Mesinkovska N, A: The Association between Alopecia and Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Dermatology 2021. doi: 10.1159/000512747
- Ojuawo A, Keith L. The serum concentrations of zinc, copper and selenium in children with inflammatory bowel disease. Cent Afr J Med. 2002 Sep-Oct;48(9-10):116-9. PMID: 14562534.
- Asghar, F., Shamim, N., Farooque, U., Sheikh, H., & Aqeel, R. (2020). Telogen Effluvium: A Review of the Literature. Cureus, 12(5), e8320. https://doi.org/10.7759/cureus.8320
- Krajmalnik-Brown, R., Ilhan, Z. E., Kang, D. W., & DiBaise, J. K. (2012). Effects of gut microbes on nutrient absorption and energy regulation. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition, 27(2), 201–214. https://doi.org/10.1177/0884533611436116
- [Abdel Aziz AM, Sh Hamed S, Gaballah MA. Possible Relationship between Chronic Telogen Effluvium and Changes in Lead, Cadmium, Zinc, and Iron Total Blood Levels in Females: A Case-Control Study. Int J Trichology. 2015 Jul-Sep;7(3):100-6. doi: 10.4103/0974-7753.167465. PMID: 26622152; PMCID: PMC4639951.
- He X, Qi Z, Hou H, Qian L, Gao J, Zhang XX. Structural and functional alterations of gut microbiome in mice induced by chronic cadmium exposure. Chemosphere. 2020 May;246:125747. doi: 10.1016/j.chemosphere.2019.125747. Epub 2019 Dec 24. PMID: 31891852.
- Colldén, H., Landin, A., Wallenius, V., Elebring, E., Fändriks, L., Nilsson, M. E., Ryberg, H., Poutanen, M., Sjögren, K., Vandenput, L., & Ohlsson, C. (2019). The gut microbiota is a major regulator of androgen metabolism in intestinal contents. American journal of physiology. Endocrinology and metabolism, 317(6), E1182–E1192. https://doi.org/10.1152/ajpendo.00338.2019
- Soory M. Bacterial steroidogenesis by periodontal pathogens and the effect of bacterial enzymes on steroid conversions by human gingival fibroblasts in culture. J Periodontal Res. 1995 Mar;30(2):124-31. doi: 10.1111/j.1600-0765.1995.tb01261.x. PMID: 7776153.
- Borgo, F., Macandog, A. D., Diviccaro, S., Falvo, E., Giatti, S., Cavaletti, G., & Melcangi, R. C. (2020). Alterations of gut microbiota composition in post-finasteride patients: a pilot study. Journal of endocrinological investigation, 10.1007/s40618-020-01424-0. Advance online publication. https://doi.org/10.1007/s40618-020-01424-0
- Pedersen N, Ankersen DV, Felding M, Wachmann H, Végh Z, Molzen L, Burisch J, Andersen JR, Munkholm P. Low-FODMAP diet reduces irritable bowel symptoms in patients with inflammatory bowel disease. World J Gastroenterol. 2017 May 14;23(18):3356-3366. doi: 10.3748/wjg.v23.i18.3356. PMID: 28566897; PMCID: PMC5434443.
The calcium-hair loss connection
The connection between calcium and hair loss isn’t straightforward. On the one hand, no studies have directly examined the relationship between calcium and hair loss. On the other hand, calcium imbalances are common in chronic conditions linked to hair shedding. So, what’s the verdict on the calcium-hair loss connection?
Can low calcium levels cause hair loss? What about high calcium levels? And if yes, by which mechanisms?
This article uncovers the answers. By the end, you’ll uncover:
- The calcium-hair loss connection: where this mineral does (and doesn’t) influence hair loss
- Calcium loading: why supplementing isn’t always the answer
- The two chronic conditions linked to hair loss and a calcium imbalance… and what to do about them.
If you have any questions, please feel free to reach out in the comments.
All-Natural Hair Supplement
The top natural ingredients for hair growth, all in one supplement.
Take the next step in your hair growth journey with a world-class natural supplement. Ingredients, doses, & concentrations built by science.

What is calcium?
Calcium is one of the most abundant trace minerals in the body. It’s most well-known for its role as a building block of teeth and bone. But, calcium does much more than that. It’s a cellular signaling molecule – driving processes from inflammation to skin cell production and the firing of our neurons (1-3).
Calcium: an essential mineral
Interestingly, calcium also influences our endocrine system: the glands, tissues, and organs that regulate hormone production. And our endocrine systems can influence nearly every aspect of biology, including the development of common hair loss disorders like androgenic alopecia (AGA) and telogen effluvium.
This is why so many people wonder if calcium plays a role in hair loss. The thinking is as follows: calcium levels influence our hormone production, and hormones influence hair loss. So maybe calcium imbalances can cause hair loss.
But is this actually true? Let’s dive into the evidence.
Can a calcium deficiency cause hair loss?
Necessary disclaimer: at the extremes, anything can cause hair loss. For example, a water deficiency can cause hair loss. If we don’t drink water, we die. If we’re dead, we can’t grow hair.
The same is true for most vitamins, minerals, and nutrients – including calcium. If we don’t ingest any calcium, we can’t grow bone. If we can’t grow bone, we die. If we’re dead, we can’t grow hair.
I hope you see where I’m going with this – which is that we’re asking the wrong question. Rather than ask, “Can a calcium deficiency cause hair loss?”, we need to ask is, “Can a calcium deficiency within realistic means cause hair loss?”
And to answer that question, we have to dive into the literature. So, what do the studies say about calcium’s role in hair loss?
There are no studies measuring calcium’s role in human hair loss.
We know that calcium is essential for the function of many tissues. We know that calcium plays a significant role in cellular signaling, a process necessary for maintaining hair growth. And we know that, in animal studies, vitamin D-deficient dogs fed a low-calcium diet develop hair loss (4).
Unfortunately, no studies have directly examined the relationship between calcium and hair loss in humans. That means we don’t yet have data to directly answer this question.
What also makes this complicated: calcium is a tightly regulated mineral. We need calcium to mediate thousands of biochemical processes. In cases of dietary deficiencies, our bodies pull calcium from bone to maintain optimal levels. In cases of dietary surpluses, our bodies expel excess calcium to avoid over-accumulation.
For these reasons, it’s unlikely that – under normal settings – our bodies would let calcium levels to drop low enough to cause problems like bone mineral depletion or hair cycling dysfunction.
But what about abnormal settings?
For example, what about in cases of disease states where our bodies’ nutrient demands are much higher… or nutrient absorption is much lower (i.e., SIBO)… or certain supplements, medications, or surgeries have caused a dysregulation of nutrients in the body?
Under these scenarios, are calcium levels implicated in hair loss? Interestingly, the answer is yes.
Both low and high calcium levels are linked to hair loss – at least indirectly. Here’s how.
The indirect links between calcium imbalances & hair loss
Calcium deficiencies: polycystic ovarian syndrome (PCOS)
Polycystic Ovarian Syndrome (PCOS) is a chronic condition that affects 15-20% of women of reproductive age (5). Its biological biomarkers: high testosterone and insulin insensitivity. Its tell-tale signs: the formation of small cysts on the ovaries, missed or infrequent periods (cycles of 35+ days), weight gain, sluggishness, and even the development of female pattern hair loss – a consequence of the prolonged hormonal imbalances (specifically, the elevated testosterone).
Interestingly, PCOS is also associated with slight (but significant) deficiencies in vitamin B-12, C, D, and calcium (6). This begs the question: are these nutrient deficiencies a cause or a consequence of PCOS?
At least so far, literature reviews suggests that PCOS-related nutrient deficiencies are consequences of PCOS, not causes (7). Specifically, these nutrient deficiencies are partly the result of prolonged insulin resistance, which can increase nutrient demand.
That means that calcium deficiencies do not cause PCOS, and are thereby only indirectly associated with the female pattern hair loss that often accompanies the condition.
Calcium surpluses: hyperparathyroidism
Interestingly, there’s at least one more way that calcium imbalances are indirectly linked to hair loss. In this case, it’s a calcium surplus… and the condition is called hyperparathyroidism.
To explain this, we’ll start by uncovering the parathyroid glands, how this relates to hair shedding, and where calcium comes into play.
The parathyroid-hair loss connection
The parathyroid glands are part of our endocrine system. They consist of four glands that sit right behind the thyroid.
When our blood calcium levels go down, the parathyroid is responsible for getting them back in the normal range. It does this by secreting a hormone called parathyroid hormone (8).
The way this happens is out-of-scope for this article, but in short, parathyroid hormone signals for our bodies to leech calcium from our bone. In leeching bone calcium, blood levels of calcium increase, and the calcium then gets redistributed to other tissues in need.
Parathyroid’s action on bone to maintain calcium homeostasis
However, there are cases where this process can backfire.
Studies have shown that when parathyroid hormone is added to hair follicle cultures, it can cause them to prematurely enter the catagen phase of the hair cycle (9). Catagen is the transition step between the growth and shedding phases of the hair cycle. Therefore, anything that initiates catagen will eventually culminate into hair shedding.
If many hairs enter catagen at once, the hair shedding can be so drastic that it leads to a visible decrease in hair density. This can lead to a temporary form of hair thinning called telogen effluvium.
Hypothetically, this opens up the possibility that chronically elevated parathyroid hormone levels could trigger chronic, persistent hair shedding. Unsurprisingly, hair loss is a common complain amongst those with an overactive parathyroid (9).
So, what causes parathyroid hormone to remain elevated for significant periods of time? And what does any of this have to do with calcium intake?
The parathyroid-calcium connection
When parathyroid hormones go out of range, it is classified as a condition called hyperparathyroidism. There are two types of hyperparathyroidism: primary and secondary.
Primary hyperparathyroidism is almost always caused by a tumor on the parathyroid gland (10). Treatment for this type of hyperparathyroidism is usually confined to removing the affected gland – and through surgery.
Secondary hyperparathyroidism, on the other hand, are characterized as out-of-range parathyroid hormone levels caused by something unrelated to a direct dysfunction of the parathyroid gland itself. As such, its causes are more complex, individualized, and wide-ranging than primary hyperparathyroidism.
One common cause of secondary hyperparathyroidism is chronic kidney disease – which severely impacts the kidney’s ability to handle calcium and vitamin D.
The other common cause of secondary hyperparathyroidism is a vitamin D deficiency (11). Interestingly, vitamin D helps regulate calcium levels in the blood. When vitamin D levels are low, calcium levels in the blood drop. This engages the parathyroid gland to increase secretion of parathyroid hormone, all so that calcium levels can increase.
Low vitamin D >> low serum calcium >> increased parathyroid hormone >> increased calcium leeching from bone >> increased serum calcium
Therefore, hyperparathyroidism is another scenario where we can see imbalanced calcium levels and hair loss. In this case, it’s usually high calcium. But similar to PCOS, the calcium dysregulation is a consequence of the chronic condition, and not a cause of the hair thinning.
If I have secondary hyperparathyroidism, will eating less calcium lower my calcium scores?
Probably not. Here’s a quick overview of the relationship between calcium intake and elevated parathyroid hormones:
- No studies have currently established a link between calcium and secondary hyperparathyroidism.
- One study on almost 60,000 women found that increased calcium intake was independently associated with a decreased risk of developing primary hyperparathyroidism (12). This suggests that, in the long run, consuming adequate calcium may prevent primary hyperparathyroidism caused by tumors.
- Outside of this, some studies (13-15) have suggested that calcium and parathyroid hormones have an inverse relationship. In other words, decreased calcium intake may lead to increased parathyroid hormone levels while increased intake leads to lower parathyroid levels. However, this increase doesn’t lead to parathyroid hormones going out of range.
From this, we can glean three things: (1) adequate calcium intake may prevent primary hyperparathyroidism, but (2) poor calcium intake doesn’t appear to cause secondary hyperparathyroidism, and (3) decreased calcium intake may lead to increased parathyroid hormone (however, this doesn’t likely lead to hyperparathyroidism).
So, when we look at the big picture, it seems that poor calcium intake isn’t strongly associated with hyperparathyroidism as both a cause or a treatment. Rather, it elevates parathyroid levels, but not too far outside of the normal range.
Therefore, if you’re dealing with hair loss and you have high (or low) calcium scores, consider getting tested for vitamin D, PCOS, and hyperparathyroidism. In the interim, make sure to eat adequate amounts of calcium.
The good news is that for most modern diets, getting enough calcium shouldn’t be too hard.
How to optimize calcium intake
In general, I’ve always felt best to get nutrients from foods as opposed to supplements. In the case of calcium, this is especially important. Here’s why.
Calcium supplementation has been linked to an increased risk of cardiovascular events (16). In some cases, calcium supplements can also disrupt the pH of the stomach, which is critical for optimal digestion and nutrient assimilation (and, thus, hair growth) (17).
The good news is that calcium is readily available in the diet – even if you’re not currently consuming dairy. Here are just a few non-dairy foods replete with calcium:
Food sources of calcium (RDI: 1,000mg) Food source, serving size Mg, % DV Egg shells (3g) 1,200mg, 120% Firm tofu (100g) 683mg, 53% Black eyed peas (100g) 128mg, 10% Okra (100g) 77mg, 6% Trout (100g) 86mg, 7% Acorn squash (100g) 44mg, 3% For most adults consuming a balanced diet, you’re probably getting enough calcium. However, if you want to be sure about your calcium intake (and other nutrients), you can always track the micronutrient sufficiency of your diet using Cronometer or FitDay.
Summary
Calcium is an essential nutrient. But aside from extreme deficiencies, calcium imbalances don’t appear to cause hair loss.
There are no human studies examining the role of calcium levels and hair loss. However, calcium is indirectly related to hair follicle cycling. Moreover, studies have shown that vitamin D-deficient animals fed a low calcium diet develop alopecia. Therefore, it’s not unreasonable to wonder if calcium plays a role in hair loss.
To date, there are only two scenarios where calcium imbalances are linked to thinning hair:
- Low calcium and hair loss observed in polycystic ovarian syndrome patients
- High calcium and hair loss observed in hyperparathyroid patients
But in both situations, the calcium imbalances are consequences of the condition, rather than the cause of the hair loss.
Evidence shows that dietary calcium has little-to-no impact on blood calcium levels, at least within normal boundaries. Having said that, calcium supplementation may lead to an increased risk of heart disease – and potentially as a direct consequence to increased arterial calcification. For these reasons, it’s generally best to avoid calcium supplements altogether and stick to food sources (if possible).
The bottom line: calcium likely plays little to no role in the overwhelming majority of hair loss cases. If you’re dealing with hair loss and you have high (or low) calcium scores, consider getting tested for vitamin D, PCOS, and hyperparathyroidism. You might save yourself a lot of time, energy, and hair.
Questions? Comments? Please reach out in the comments section below.
References
- Klein G. L. (2018). The Role of Calcium in Inflammation-Associated Bone Resorption. Biomolecules, 8(3), 69. https://doi.org/10.3390/biom8030069
- Bikle, D. D., Xie, Z., & Tu, C. L. (2012). Calcium regulation of keratinocyte differentiation. Expert review of endocrinology & metabolism, 7(4), 461–472. https://doi.org/10.1586/eem.12.34
- Gleichmann, M., & Mattson, M. P. (2011). Neuronal calcium homeostasis and dysregulation. Antioxidants & redox signaling, 14(7), 1261–1273. https://doi.org/10.1089/ars.2010.3386
-
Mady LJ, Ajibade DV, Hsaio C, Teichert A, Fong C, Wang Y, Christakos S, Bikle DD. The Transient Role for Calcium and Vitamin D during the Developmental Hair Follicle Cycle. J Invest Dermatol. 2016 Jul;136(7):1337-1345. doi: 10.1016/j.jid.2016.02.813. Epub 2016 Mar 16. PMID: 26994969.
- Sirmans SM, Pate KA. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin Epidemiol. 2013;6:1-13. Published 2013 Dec 18. doi:10.2147/CLEP.S37559
-
Szczuko M, Skowronek M, Zapałowska-Chwyć M, Starczewski A. Quantitative assessment of nutrition in patients with polycystic ovary syndrome (PCOS). Rocz Panstw Zakl Hig. 2016;67(4):419-426. PMID: 27925712.
- El Hayek S, Bitar L, Hamdar LH, Mirza FG, Daoud G. Poly Cystic Ovarian Syndrome: An Updated Overview. Front Physiol. 2016;7:124. Published 2016 Apr 5. doi:10.3389/fphys.2016.00124
-
Lofrese JJ, Basit H, Lappin SL. Physiology, Parathyroid. [Updated 2020 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
-
Skrok, A., Bednarczuk, T., Skwarek, A., Popow, M., Rudnicka, L., & Olszewska, M. (2015). The effect of parathyroid hormones on hair follicle physiology: implications for treatment of chemotherapy-induced alopecia. Skin pharmacology and physiology, 28(4), 213–225. https://doi.org/10.1159/000375319
-
Pokhrel B, Levine SN. Primary Hyperparathyroidism. [Updated 2020 Aug 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
-
Muppidi V, Meegada SR, Rehman A. Secondary Hyperparathyroidism. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
-
Paik, J. M., Curhan, G. C., & Taylor, E. N. (2012). Calcium intake and risk of primary hyperparathyroidism in women: prospective cohort study. BMJ (Clinical research ed.), 345, e6390. https://doi.org/10.1136/bmj.e6390
-
Jorde, R., Sundsfjord, J., Haug, E., & Bonaa, K. H. (2000). Relation between low calcium intake, parathyroid hormone, and blood pressure. Hypertension (Dallas, Tex. : 1979), 35(5), 1154–1159. https://doi.org/10.1161/01.hyp.35.5.1154
-
Patel, P., Mughal, M. Z., Patel, P., Yagnik, B., Kajale, N., Mandlik, R., Khadilkar, V., Chiplonkar, S. A., Phanse, S., Patwardhan, V., Patel, A., & Khadilkar, A. (2016). Dietary calcium intake influences the relationship between serum 25-hydroxyvitamin D3 (25OHD) concentration and parathyroid hormone (PTH) concentration. Archives of disease in childhood, 101(4), 316–319. https://doi.org/10.1136/archdischild-2015-308985
-
Aloia, J., Bojadzievski, T., Yusupov, E., Shahzad, G., Pollack, S., Mikhail, M., & Yeh, J. (2010). The relative influence of calcium intake and vitamin D status on serum parathyroid hormone and bone turnover biomarkers in a double-blind, placebo-controlled parallel group, longitudinal factorial design. The Journal of clinical endocrinology and metabolism, 95(7), 3216–3224. https://doi.org/10.1210/jc.2009-1294
-
Bolland, M. J., Grey, A., & Reid, I. R. (2013). Calcium supplements and cardiovascular risk: 5 years on. Therapeutic advances in drug safety, 4(5), 199–210. https://doi.org/10.1177/2042098613499790
-
Salisbury BH, Terrell JM. Antacids. [Updated 2020 Sep 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526049/
Does vitamin B12 improve hair growth? Supplement companies say yes, but scientific studies reveal a much murkier (and nuanced) relationship between vitamin B12, hair loss, and hair growth… one you’ll want to understand before you start supplementing.
In this article, we’ll dive into the arguments for and against a connection between vitamin B12 and hair growth. We’ll explore methylation, vitamin B12’s role in the hair cycle, and B12’s connection to different hair loss disorders. Then, we’ll reveal when vitamin B12 might (and might not) help our hair.
Finally, we’ll outline some potential best-practices for those who want to supplement with vitamin B12 for hair growth. After all, too little (and too much) of this vitamin may be counterproductive to both our hair and overall health.
All-Natural Hair Supplement
The top natural ingredients for hair growth, all in one supplement.
Take the next step in your hair growth journey with a world-class natural supplement. Ingredients, doses, & concentrations built by science.

What is vitamin B12?
Vitamin B12 is a singular vitamin apart of the greater B complex family. Like many B vitamins, vitamin B12 acts as an enzymatic cofactor for essential functions of the body (1). Specifically, vitamin B12 helps us metabolize food, produce red blood cells, and “methylate” DNA (more on this later). It also plays a protective role in cardiovascular health, as it helps to reduce excess amounts of a protein called homocysteine – which, at high levels, is inflammatory.
Vitamin B12 Supplement Mockup
Given its importance in so many bodily functions, it’s natural to wonder: does vitamin B12 also help fight hair loss? After all, it seems to be a staple ingredient in most hair health nutritional supplements. So, what does the evidence show?
The case for a vitamin B12-hair loss connection
From a scientific perspective, vitamin B12 might support hair growth in many ways.
- Vitamin B12 help support the production of DNA – which is necessary to maintain the rapid cell division that drives hair growth (2). Without cell division, not only can hair not grow… but human life cannot sustain itself, either. In this respect, technically anything that supports human survival – even water – supports hair growth.
- Vitamin B12 helps us produce hemoglobin – a molecule inside our red blood cells that carries oxygen and iron into our tissues (3). When someone has low hemoglobin, they often have an iron deficiency (i.e., anemia). Interestingly, anemia is highly correlated with hair loss – particularly in women ages 14-40 – and vitamin B12 supplementation can help improve hemoglobin product and thereby iron levels for those who are deficient.
But there’s also another reason that vitamin B12 might support hair growth – and it happens to do with one of the biggest buzzwords surrounding this vitamin: methylation.
In the simplest terms, methylation is a way in which our bodies can “turn on” or “turn off” certain genes. In other words, methylation helps change our gene expression – and thereby influences our ability to prevent cancer, reduce inflammation, and everything in between.
Here are just a few roles that methylation – and our methylation cycle – regulates inside our bodies:
- Production of methionine and cysteine. These are two sulfur-based amino acids that play integral roles in muscle building, inflammation regulation, and antioxidant production.
- Glutathione production. Sulfur amino acids are a major precursor for glutathione, the body’s master antioxidant.
- Homocysteine reduction. High levels of homocysteine in the blood are linked to a variety of inflammatory diseases.
- Production of SAMe. This protein is believed to support mental health, among many other things (4).
So, how does methylation relate to B12 and hair loss?
In one study on rabbits, researchers found methionine to be a promoter of hair growth. The mechanism behind this? An increase in the activity of the Wnt/β-catenin signaling pathway (5).
The Wnt/β-catenin pathway is important to this discussion for a few reasons:
- This pathway helps promote the creation of stem cells, which are required for hair growth and hair follicle function (6).
- In androgenic alopecia (AGA) – the most common form of hair loss in adult men – male hormones interfere with Wnt/β-catenin signaling. Specifically, this signaling pathway is dampened, also known as downregulated. As a result, hair follicle stem cell activity is impaired, which prevents proper hair cycling. This shortens the growth stage of a hair follicle, causing it to prematurely shed. Over time, this hinders hair growth and may even accelerate hair follicle miniaturization – a defining hallmark of male and female pattern hair loss (7).
Here’s where vitamin B12 might come into play:
Vitamin B-12 is a cofactor in the methylation cycle, meaning that it helps to activate methylation. Interestingly, vitamin B-12 deficiencies are believed to be a major driver of a dysfunctional methylation cycle – as evidenced by an association between homocysteine levels and vitamin B-12 deficiency (8). This suggests that the methylation cycle is “backed up”, preventing homocysteine from being converted to cysteine and methionine.
Thus, B-12 deficiency may impair methionine synthesis from the methylation cycle. Because we know that methionine contributes to Wnt/β-catenin signaling, it’s possible that a reduction in methionine may lead to reduced Wnt/β-catenin activity. And therefore, it’s possible that a vitamin B12 deficiency in scalp tissues might play a role for people dealing with androgenic alopecia.
Summary (so far): how vitamin B12 might help fight hair loss
There are a variety of ways that vitamin B12 might be connected to hair loss in humans:
- Vitamin B12 helps support DNA synthesis. Without DNA synthesis, we would die. We can’t grow much hair if we’re dead.
- Vitamin B12 helps normalize hemoglobin production (and thereby iron levels). For females with both hair loss and an iron deficiency, vitamin B12 might be a great way to improve iron status and encourage hair growth.
- Vitamin B12 helps support methylation. This might have ramifications for one of the world’s most common hair loss disorders – male pattern hair loss (AGA. In AGA-affected hair follicles, the Wnt / β-catenin signaling pathway is dampened, which leads to shorter-growing hair, premature hair shedding, and potentially even hair follicle miniaturization. If this happens to be the direct result of a deficit in localized methylation in scalp tissues, then vitamin B12 might help improve methylation and thereby improve Wnt / β-catenin signaling, which would allow for hairs to grow longer, shed less prematurely, and (hopefully) not miniaturize as quickly.
But it’s important to stress: these suspected mechanism are all hypothetical. Yes, vitamin B12 is connected to each mechanism. Yes, these mechanisms are linked to hair loss (and hair growth). But there’s a difference between association and causation. And this difference, unfortunately, is consistently forgotten by companies trying to sell you B12 supplements. Thus, to prove a strong association or causation, the real questions we should be asking are:
- Are vitamin B12 deficiencies (in skin tissues or throughout the body) observed more frequently in people who are balding?
- Does vitamin B12 – through supplementation or topical application – actually improve hair loss outcomes?
In answering these questions, we can actually discern whether or not it makes sense for most people to spend money on vitamin B12 supplements to try and regrow their hair.
And as you can guess, these questions happen to lead us to our next section: the case against a vitamin B12-hair loss connection.
The case against a vitamin B12-hair loss connection
While there is hypothetical evidence linking vitamin B12 to hair loss and hair growth, this argument begins falls apart when we zoom out and start looking at the broader evidence.
Specifically, we’re going to talk about the following:
- Misconceptions about methylation, B12, Wnt/β-catenin pathways, and hair loss
- Vitamin B12 levels of hair loss patients
- Observations in birth control-induced vitamin B12 deficiencies, and what this does (or doesn’t do) to hair
Methylation misconceptions
Earlier we discussed how, in balding hair follicles, a deficiency in the methylation cycle might interfere with Wnt/β-catenin signaling pathways, which might accelerate hair loss. We argued that because vitamin B12 supports methylation, this vitamin might also help reverse this methylation deficiency, and thereby help fight hair loss from androgenic alopecia.
But it’s important to note: vitamin B12 is just one (of many) vitamins and nutrients that support methylation. For instance, many other B-vitamins also support methylation, and these B-vitamins are found in abundance in foods like beef, eggs, and poultry.
This means that even if you do have a vitamin B12 deficiency, your body will likely be able to compensate for this – at least from a methylation perspective – via your dietary choices. Therefore, in balding hair follicles, even if Wnt / β-catenin downregulation were exclusively due to a methylation issue (it isn’t), your body would still have many “fallback” vitamins to address that methylation issue. So, in androgenic alopecia, changes to a hair follicle’s gene expression cannot be significantly attributed to a vitamin B12 deficiency.
Therefore, it also shouldn’t be surprising to find out that there aren’t any differences in vitamin B12 levels between those with and without hair loss.
Looking at B12 levels in the blood of hair loss patients
When we zoom out beyond the actual hair follicle and look at studies on people with common hair loss disorders like AGA, telogen effluvium (TE), or alopecia areata (AA) – the data are consistently clear: there is no difference in blood measurements of vitamin B12 between people with and without hair loss (9). In other words, people who are losing their hair and who have full heads of hair appear to have the same vitamin B12 levels.
Even more compelling, recent literature reviews have found no evidence to support the use of vitamin B12 for hair loss of any type (9). That means that not only are vitamin B12 levels the same across those with and without hair loss, but that for those with hair loss, vitamin B12 supplementation generally doesn’t improve hair loss outcomes.
What about women with hair loss due to an iron deficiency? Doesn’t vitamin B12 help improve iron stores, and have some therapeutic benefit here?
Yes and no.
Earlier, we argued a connection between hemoblogin, iron, vitamin B12, and hair loss. As a refresher, hemoglobin is a molecule found in red blood cells. Hemoglobin carries oxygen and iron, and in general, when someone has low hemogloblin levels, they also have low iron (10). Low iron levels are often found in women ages 14-40 with hair loss. Vitamin B12 is a key cofactor in hemoglobin formulation. Therefore, you might be able boost hemoglobin production with vitamin B12, and therefore potentially normalize low iron levels. If someone is dealing with hair loss as a direct result of low iron levels, then vitamin B12 supplementation might help to normalize these levels and maybe regrow some hair.
So, in a situation where someone’s hair loss is due to poor iron status, and their poor iron status is a direct result of low vitamin B12, then it absolutely makes sense to supplement with vitamin B12. In doing so, you’d improve hemoglobin production, oxygen and iron transport, and (very likely) hair loss outcomes. This is why a lot of popular hair loss supplements – like Nutrafol – contain B12.
At the same time, a vitamin B12 deficiency is only one possible contributor toward an iron deficiency. A more likely contributor? A deficiency in iron itself (11). So, while vitamin B12 is probably therapeutically useful in some circumstances of iron deficiency-related hair loss, it’s not the only reason – or even the biggest reason – for why the iron deficiency arises.
Therefore, B12 is likely useful for a much smaller percentage of women than advertisements for these hair health supplements might lead you to believe.
Observations in birth control-induced B12 deficiency
This argument is further strengthened by another observation researchers have made: women with vitamin B12 deficiencies caused by hormonal birth control don’t experience hair loss or adverse changes to hair growth (9). As such, even when a deficiency is present, it doesn’t seem to negatively impact hair growth. In fact, many women on hormonal contraceptives report the opposite effect – hair regrowth – which is why some contraceptives are also used off-label as a hair loss treatment.
The good news? Vitamin B12 might help reverse premature hair graying
In regard to hair health, there is one way that vitamin B12 might positively impact hair health outcomes. It might help to prevent, or even reverse, premature graying.
To be clear, the majority of research doesn’t indicate B12 deficiency is a cause of hair loss. But, there are several reports supporting an association between inadequate B12 levels and premature hair graying, which is grey hair that onsets before the ages of 20-30 (depending on the demographic) (12).
For instance, one small study demonstrated that individuals with premature hair graying had lower vitamin B12, folate, and biotin levels than control subjects without premature gray hair (13). Additionally, some studies report a higher incidence of premature graying in pernicious anemia, a blood condition sometimes caused by B12 deficiency (14).
There are also three case reports of patients reversing their premature gray hair with B12 supplementation (15-17). Needless to say, there seems to be evidence of both an association of low B12 and early greying, and a reversal of early greying following B12 supplementation.
The association between B12 deficiency and premature graying isn’t fully established, and there are absolutely other factors that can lead to premature hair graying. Moreover, B12 supplementation is really only relevant to reversing graying hair in the context of B12 deficiency.
That being said, a vitamin B12 deficiency may be worth investigating for anyone experiencing premature hair graying – regardless of whether you’re losing your hair.
The verdict: in most situation, vitamin B12 likely has no effect on hair loss (and hair regrowth), but vitamin B12 might reverse premature hair graying in the presence of B12 deficiency
Although hypothetical evidence suggests an absence of B12 activity could negatively impact hair growth, in vivo human studies indicate that either (1) there is no relationship between vitamin B12 deficiency and hair loss and/or (2) there is an overriding factor (like methionine provision outside of the methylation cycle) that prevents B12 deficiency from causing hair loss.
The exception to this is if someone has iron deficiency-related hair loss, and if their iron deficiency is exclusively the result of poor hemoglobin production due to a vitamin B12 deficiency. In this case, vitamin B12 supplementation can address the deficiency, improve hemoglobin production, and thereby drastically improve iron transport (and, ultimately, hair growth). But it goes without mentioning that this is a very specific scenario that is not faced by the majority of hair loss sufferers in the developed world.
In any case, it’s clear that supplementing with B12 is probably not the best solution for improving hair growth – at least as a standalone therapy.
That being said, it’s important to note that having adequate B12 is essential for optimal health. Even if it doesn’t cause hair loss, B12 deficiency can still lead to anxiety, fatigue, neuropathy, and cardiovascular issues, among other health issues. Moreover, B12 deficiency appears to be one potential cause of premature hair graying.
As such, even if it doesn’t improve hair loss, some may still find it necessary to supplement with vitamin B12. So, in these cases, what’s the best approach for supplementation?
Things to keep in mind when supplementing with vitamin B12
Vitamin B12 supplements are available in three forms: cyanocobalamin, methylcobalamin, and adenosylcobalamin. Methyl- and adenosylcobalamin are naturally-occurring forms of B12 whereas cyanocobalamin is synthetic.
Though synthetic is not always subpar to naturally-occurring forms of B12, in this case, supplementing with methyl- and adenosylcobalamin B12s is much more efficient. The reason for this is they are already in their active forms, ready to be used by the body. Cyanocobalamin, on the other hand, requires enzymatic processing before it can be utilized. On top of this, cells don’t seem to retain cyanocobalamin as well as some of the other forms (18).
Additionally, some researchers have raised concerns with long term cyanocobalamin supplementation, due to the cyanide present in the compound (18). Even though these concerns aren’t yet substantiated, an abundance of caution may be warranted here.
The bottom line? If your diet isn’t providing you with enough vitamin B12 and you choose to supplement, consider opting for a B-complex or multivitamin formulated with methyl- or adenosylcobalamin.
Summary
Vitamin B12 deficiency isn’t likely to be a cause for hair loss. As such, claims that supplementing with B12 will improve hair growth are largely unfounded. This is despite some pretty compelling theoretical evidence – like B12’s role in hemoglobin formation, nucleic acid synthesis, and the methylation cycle that produces growth-supporting methionine.
It just goes to show how important it is that we don’t rely on studies of isolated nutrients in cell cultures. Moreover, we shouldn’t have high hopes for products marketed on these premises when it comes to regrowing our hair.
That being said, vitamin B12 deficiency can still cause real problems and, in some cases, may be an underlying factor in premature hair graying. So, for those who are dealing with early-onset gray hair, it may be worth checking your B12 levels. And if you are deficient? Restoring your B12 levels may just reverse the condition.
So, if supplementing is warranted in your case, opt for a methyl- or adenosylcobalamin-containing supplement over one containing cyanocobalamin. They’re more bioavailable and may be safer in the long-term.
But, for the overwhelming majority? You’re likely to get all the vitamin B12 you need from food — more than enough to rule it out as a plausible factor in hair loss.
Have any questions about vitamin B12? Leave them below.
References
- Al Amin ASM, Gupta V. Vitamin B12 (Cobalamin) [Updated 2020 Jun 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559132/
- Almohanna HM, Ahmed AA, Tsatalis JP, Tosti A. The Role of Vitamins and Minerals in Hair Loss: A Review. Dermatol Ther (Heidelb). 2019;9(1):51-70. doi:10.1007/s13555-018-0278-6
- Ferreira GC. Heme biosynthesis: biochemistry, molecular biology, and relationship to disease. J Bioenerg Biomembr. 1995;27(2):147-150. doi:10.1007/BF02110029
- Sharma A, Gerbarg P, Bottiglieri T, et al. S-Adenosylmethionine (SAMe) for Neuropsychiatric Disorders: A Clinician-Oriented Review of Research. J Clin Psychiatry. 2017;78(6):e656-e667. doi:10.4088/JCP.16r11113
-
Zhu Y, Wu Z, Liu H, Liu G, Li F. Methionine promotes the development of hair follicles via the Wnt/β-catenin signalling pathway in Rex rabbits. J Anim Physiol Anim Nutr (Berl). 2020 Jan;104(1):379-384. doi: 10.1111/jpn.13238. Epub 2019 Nov 15. PMID: 31732998.
- Choi YS, Zhang Y, Xu M, et al. Distinct functions for Wnt/β-catenin in hair follicle stem cell proliferation and survival and interfollicular epidermal homeostasis. Cell Stem Cell. 2013;13(6):720-733. doi:10.1016/j.stem.2013.10.003
- Chen X, Liu B, Li Y, et al. Dihydrotestosterone Regulates Hair Growth Through the Wnt/β-Catenin Pathway in C57BL/6 Mice and In Vitro Organ Culture. Front Pharmacol. 2020;10:1528. Published 2020 Jan 23. doi:10.3389/fphar.2019.01528
- Gilfix BM. Vitamin B12 and homocysteine. CMAJ. 2005;173(11):1360. doi:10.1503/cmaj.1050170
- Almohanna HM, Ahmed AA, Tsatalis JP, Tosti A. The Role of Vitamins and Minerals in Hair Loss: A Review. Dermatol Ther (Heidelb). 2019;9(1):51-70. doi:10.1007/s13555-018-0278-6
- National Academy of Sciences (US) and National Research Council (US) Division of Medical Sciences. Conference on Hemoglobin: 2–3 May 1957. Washington (DC): National Academies Press (US); 1958. THE ROLE OF IRON IN HEMOGLOBIN SYNTHESIS. Available from: https://www.ncbi.nlm.nih.gov/books/NBK224286/
- Trost LB, Bergfeld WF, Calogeras E. The diagnosis and treatment of iron deficiency and its potential relationship to hair loss. J Am Acad Dermatol. 2006 May;54(5):824-44. doi: 10.1016/j.jaad.2005.11.1104. PMID: 16635664.
- Kumar AB, Shamim H, Nagaraju U. Premature Graying of Hair: Review with Updates. Int J Trichology. 2018;10(5):198-203. doi:10.4103/ijt.ijt_47_18
- Daulatabad D, Singal A, Grover C, Chhillar N. Prospective Analytical Controlled Study Evaluating Serum Biotin, Vitamin B12, and Folic Acid in Patients with Premature Canities. Int J Trichology. 2017;9(1):19-24. doi:10.4103/ijt.ijt_79_16
-
Dawber RP. Integumentary associations of pernicious anaemia. Br J Dermatol. 1970 Mar;82(3):221-3. doi: 10.1111/j.1365-2133.1970.tb12428.x. PMID: 5441758.
-
Noppakun N, Swasdikul D. Reversible hyperpigmentation of skin and nails with white hair due to vitamin B12 deficiency. Arch Dermatol. 1986 Aug;122(8):896-9. PMID: 3740873.
-
Carmel R. Hair and fingernail changes in acquired and congenital pernicious anemia. Arch Intern Med. 1985 Mar;145(3):484-5. PMID: 3977516.
-
Niiyama S, Mukai H. Reversible cutaneous hyperpigmentation and nails with white hair due to vitamin B12 deficiency. Eur J Dermatol. 2007 Nov-Dec;17(6):551-2. doi: 10.1684/ejd.2007.0285. Epub 2007 Oct 19. PMID: 17951150.
- Paul C, Brady DM. Comparative Bioavailability and Utilization of Particular Forms of B12 Supplements With Potential to Mitigate B12-related Genetic Polymorphisms. Integr Med (Encinitas). 2017;16(1):42-49.
Alopecia areata is an autoimmune form of hair loss that affects 2% of people worldwide. If you’re dealing with alopecia areata, the burden of hair loss often feels overwhelming – as the condition can progress rapidly, inexplicably, and without regard.
Fortunately, alopecia areata is treatable. In many cases, it’s also reversible. The first step toward making progress? Understanding alopecia areata, its myriad triggers, and how these factors relate to your unique hair loss situation.
In this article, we’ll uncover the characteristics of alopecia areata: its clinical presentations, histological features, and more. We’ll also dive into alopecia areata’s causes: what we know, what we don’t, and what this type of hair loss can tell us about our health.
Finally, we’ll outline treatments for alopecia areata (both conventional and natural): the research supporting them, the expectations for regrowth, and who might be the best candidates for each intervention.
What is alopecia areata?
Alopecia areata (AA) is a form of hair loss driven by autoimmunity. To put it simply, alopecia areata occurs when our bodies mistakenly recognize our hair follicles as foreign invaders, and then begin to attack our hair follicles. This leads to the dysfunction of hair follicle stem cells, and eventually, hair loss.
What does alopecia areata look like?
You might know alopecia areata (AA) from its “patchy” presentation, whereby slick-bald patches begin to form in a non-uniform fashion. But AA can also vary in appearance – and even mask the look of many other common hair loss disorders.
Types of alopecia areata
Alopecia areata focalis or “patchy” alopecia areata Hair loss in patches, can extend beyond just the scalp. The most common form of alopecia areata. It may or may not progress into alopecia totalis or alopecia universalis. Alopecia areata totalis Loss of all hair on the scalp including eyelashes and eyebrows. Alopecia areata universalis Hair loss of the scalp, eyelashes, eyebrows, and whole body, including all body hair. Ophiasis or alopecia areata marginata Hair loss around the circumference of the head in a band-like fashion. It is most commonly seen behind the ears and the nape of the neck, but can occur in the frontal hairline and extend throughout the scalp in severe cases, as well. Ophiasis inversus Hair loss that begins in the center of the scalp and progresses into the surrounding regions. Alopecia areata incognita Diffuse hair loss whereby no specific bald “patches”, normally characteristic of alopecia areata, can be distinguished. What’s the histology of alopecia areata?
Histology is a term used to describe a close-up view of a tissue’s structure. In the world of hair loss, histology refers to the microscopic view of a hair follicle (i.e., what a hair follicle looks like when biopsied).
When doctors are uncertain about someone’s hair loss diagnosis, they’ll often take a biopsy of their patient’s scalp so that they can get a look of the histological features of the affected hair follicles. Then, they’ll compare what they see against the histological hallmarks of certain hair loss disorders.
It might sound invasive, but these scalp biopsies are perhaps the most effective way for dermatologists to definitively diagnose someone’s hair loss. And when it comes to alopecia areata, this type of hair loss has a lot of interesting features:
- Inflammation. Specifically, the infiltration of lymphocytes near hair follicle stem cell bulges. Lymphocytes are immune cells; the bodies uses them as part of an inflammatory response. Where there are high lymphocytes, there are usually high amounts of inflammation. One study found that 84% of alopecia areata subjects presented with this kind of inflammation.
- Dysfunctional hair follicle stem cell bulges. Hair follicle stem cells contain the blueprints to make new hair follicles. When too many lymphocytes collect near these stem cells, they generate inflammation, and that inflammation interferes with the ability for these stem cells to function. This leads to stem cell dysfunction and an inability to form new hair.
- Hair follicle miniaturization. This is a decrease in hair strand diameter, which leads to thinner-looking hair. One study observed that 90% of alopecia areata subjects had hair follicle miniaturization. Conversely, this study only found miniaturization in 25% of subjects. This study found that the presence of miniaturization is likely dependent on the nature of the hair loss – for example, early stages of AA likely do not present with miniaturization. It is most commonly often found in recurrent and chronic forms of AA.
- Increased number of catagen hairs. This study found that 93% of patients presented with an abnormally high number of hair follicles in the catagen phase – the phase in the hair cycle whereby nutrient supply is cut off and the hair prepares to shed. In healthy scalps, only 1% of hair follicles are typically in catagen. With AA, that percent can skyrocket.
Isn’t inflammation & hair follicle miniaturization part of androgenic alopecia (AGA)?
Yes.
Pattern hair loss, also known as androgenic alopecia (AGA), is also often defined by the presence of inflammation, hair follicle miniaturization, and even an increased number of catagen and telogen hairs. This begs the question: how can we distinguish between AGA and alopecia areata… especially in cases where alopecia areata is diffuse?
Well, there are some additional factors that can help us identify if we’re dealing with alopecia areata (AA) or androgenic alopecia (AGA).
What makes alopecia areata (AA) unique from androgenic alopecia (AGA)?
- The patterning of AA. In most AA cases, hair loss begins in a “patchy” fashion — a patterning that is exclusive to AA. In contrast, AGA occurs in a very different, yet still distinct manner. For men, it’s temple recession and crown thinning. For women, it’s most often a widening of the part while their hairline stays intact (also known as a “Christmas tree” pattern).
- Exclamation-point hairs in AA. Exclamation point hairs, pictured below, are a phenomenon only observed in AA. These hairs remain thick along the shaft but are noticeably thinner towards the opening of the follicle, creating an appearance akin to that of an exclamation mark ( ! ). This is only a defining factor if hair is still present.
-
Exclamation mark (!) hair
-
- Pigment casts in AA. Melanin is a substance produced by cells to create pigment for our skin and hair. Interestingly, in cases of AA, there are often “clumps” of melanin deposits throughout the follicular unit. This can appear like a small, dark tattoo where there should be a hair follicle. The incidence of pigment casts varies from study to study from 44% to 72%. Having said that, pigment casts by themselves aren’t a good indicator of AA – mostly because they’re often observed at similar rates in other hair loss disorders like trichotillomania (i.e., a “hair-pulling disorder”).
What causes alopecia areata?
To reiterate from earlier, inflammation seems to initiate of AA. The process looks like this:
- Inflammatory cells infiltrate the area surrounding a hair follicle stem cell bulge.
- This inflammation disrupts stem cell functionality, leading to stem cell dysfunction.
- These dysfunctional stem cells stop producing normal-looking hair follicles.
This leads to:
- Rapid hair follicle miniaturization (i.e., exclamation hairs).
- A loss of visible hair (i.e., slick-bald patches in alopecia areata focalis).
- Weaker, brittler hair that breaks off soon after growing out of the skin surface.
This begs the question… when it comes alopecia areata, what causes the inflammation that kickstarts the whole process?
What causes the inflammation in alopecia areata?
While the exact origin of inflammation isn’t known, researchers have a good idea of three contributing factors: genetics, environmental triggers, and loss of immune privilege in the follicle.
And though we don’t know the exact nature of these contributing factors, researchers have begun to uncover some of the details:
- Genetics. Studies have shown that AA is common among family members, affirming the role of a genetic component in certain cases. Specific genes affected include those that code for immune cell receptors, cell death coordination, immune-regulating cells, other proteins that regulate cellular communication.
- Environmental factors. Much like genetics, environmental elements faced by AA-affected families might also explain why this condition tends to appear multiple times within the same family. These environmental factors include
- Stress
- Infections
- Hormone fluctuations
- Dysbiosis of the gut flora
- Oxidative stress
- Soy consumption (implicated in animal studies, though not yet confirmed in human studies)
- Nutrient deficiencies (specifically, vitamin A and/or vitamin D deficiency.
- Loss of immune privilege. Under normal circumstances, a hair follicle produces its own “shield” from our own immune system. This shield is comprised of many immune-suppressing molecules. This is known as immune privilege, and it’s what make hair follicles incredibly unique mini-organs. However, in AA, researchers believe this immune privilege collapses – preventing the hair follicle from protecting itself against a damaging attack by the immune system. This would lead to inflammation and, thereby, the destruction of the hair follicle stem cell bulge. How this occurs is unknown, but researchers believe it is a result of proteins secreted by skin cells that the body forms an “antibody” to, leading to an immune attack.
What are the available treatments?
Currently, there are a variety of drug and non-drug treatments for AA. But before we reveal them, there are two things worth mentioning:
- Because we don’t fully understand why AA occurs, the most well-studied treatments primarily focus on suppressing the signals that lead to AA (as opposed to treating its root cause). More recent research has explored treatments that try to target some of these potential root causes. These studies show promise, but they’re also a little “out there” in terms of peoples’ comfortabilities. So, as you read on, keep this in mind.
- When it comes to reversing alopecia areata, 34-50% of cases resolve spontaneously. This makes it hard to know which treatments work, and which treatments just happened to coincide with spontaneous reversals. This is why control groups are so important in AA studies. Moreover, the likelihood of spontaneous reversal depends highly on the progression of the disease: as AA progresses, the likelihood of spontaneous resolution declines.
Regardless of these factors, it seems like treating AA in earlier stages leads to better outcomes and decreases the risk of future treatment resistance. So, if you’re facing AA right now, it’s best not to place your bets on a spontaneous reversal; rather, hedge those bets with the treatment options at your disposal (or at least the ones you’re comfortable trying).
The following sections detail many conventional and alternative treatments: the evidence, best practices, mechanisms of action, and more.
Drug-based treatments
Topical, intralesional, and systemic steroids (first line of treatment)
- Best candidates: Patchy AA may be controlled with topical or intralesional steroids. More severe or resistant cases (alopecia totalis, alopecia universalis, ophiasis) may require systemic steroid treatment or combination therapy (steroids + other treatments).
- Mechanisms of action: Reduction of inflammation.
- Dosages: For topical steroids, concentrations vary from 0.05% to 0.25%; for intralesional steroids, most commonly-used agent is triamcinolone acetonide, at concentrations of 2.5 mg/mL to 10 mg/mL; for systemic steroids, varying doses given as pulse doses, a.k.a large bolus doses for a specific period of time, administered in intervals.
- Outcomes: Results vary between methods of administration. Topical steroids are best suited to earlier stages of AA, with about 57% of these patients demonstrating complete regrowth. Intralesional steroids have a slight advantage over topicals, with 63% of patients achieving complete growth in one study. Systemic steroid treatment is primarily relegated to resistant cases.
- Problems: With topical and intralesional treatment, the main side effect is cutaneous atrophy or thinning of the skin. Systemic steroids come with a higher risk of side effects, and these risks may outweigh the benefits of hair growth. The relapse rate after steroid treatment ranges between 33% and 75%.
Janus kinase (JAK) inhibitors (oral and topical)
- Best candidates: Men, women, and children with patchy AA, alopecia universalis, alopecia totalis, according to preliminary evidence.
- Mechanisms of action: Blocks inflammatory signaling.
- Dosages: 5mg twice per day.
- Outcomes: Efficacy is similar in patchy alopecia areata, alopecia universalis, and alopecia totalis as well as in both men vs. women and adults vs. children. Oral administration is more likely to produce a good response when compared to the use of topical applications. Studies show initial hair growth occurs as soon as 2 months, with full regrowth occurring in an average of 6 months.
- Problems: Evidence is limited and primarily in the form of case reports. As such, though JAK inhibitors show promise, we don’t know a lot about the safety or efficacy of these medications in AA, yet. Drugs in this class have been linked to an increased risk of upper respiratory issues, latent virus reactivation, and cancer. The exact risk of these adverse effects in the treatment of AA is unknown, however, upper respiratory infection was the most common among available case studies. Like other therapies in AA, there is a high rate of relapse after cessation of the drug.
Immunotherapy (dinitrochlorobenzene, squaric acid dibutylester and diphenylcyclopropenone, with diphenylcyclopropenone)
- Best candidates: Mild to moderate patchy alopecia areata.
- Mechanisms of action: Immunogenic compound “distracts” the immune system with a more stimulating antigen than the self-antigen the mediates the autoimmune reaction.
- Dosages: Concentration sufficient enough to induce an allergic response.
- Outcomes: Response rates as reported in the literature range widely, from about 9% to 87%. About 20% to 30% of patients are able to achieve significant hair growth, such that they are able to manage their hair loss without a wig. This specific therapy may require longer treatment times, as evidenced by over a two-fold increase in response rate at 32 months versus 6 months. So, ask your doctor about whether a longer treatment period might be right for you. In over 30 years of use, long-term side effects have not been reported with immunotherapy, however, some side effects can occur during therapy. The most common side effect is cervical and occipital lymphadenopathy and severe dermatitis, however, these only last for the duration of the therapy. Moreover, dermatitis can be avoided by using the proper concentration of the antigenic compounds. Vitiligo and itching have also been reported but are considered rare. Overall, the treatment appears to be well-tolerated and effective.
- Problems: As with most treatments, relapse rates are high at around 62%. Response rates are somewhat low when administered for the same treatment periods as other treatments. In other words, immunotherapy takes longer to work than other treatments.
Minoxidil
- Best candidates: Mild patchy AA, AA patients tapering off of steroid therapy
- Mechanisms of action: Not fully known, but is believed to stimulate the “anagen” growth phase of the hair cycle, thereby promoting regrowth of lost hairs.
- Dosages: 2% or 5% minoxidil, two to three times daily.
- Outcomes: In one study, 85% of patients using 5% minoxidil alone experienced regrowth, however, this regrowth wasn’t cosmetically significant. Another study demonstrated that the application of 2% minoxidil, when applied three times daily, helped retain hair regrowth after tapering off of steroid treatment.
- Problems: Minoxidil doesn’t seem to be that effective outside of post-steroid hair retention.
Methotrexate
- Best candidates: Moderate to severe AA, including universalis, diffuse, and totalis phenotypes.
- Mechanisms of action: Suppression of the immune system.
- Dosage: 10-25mg per week + folate/folic acid supplements (methotrexate depletes folic acid).
- Outcomes: One study reported that 44.4% of subjects taking methotrexate were able to regain 50% or more of their hair as observed in a follow-up period ranging from 3 to 51 months. The best responders were males, those with multifocal patchy AA (followed by totalis, then universalis, and, lastly, diffuse), and those who used a cumulative dose of 1,000 to 1,500mg. When corticosteroids were used alongside methotrexate, the number of patients regrowing at least 50% of their hair increased to 77.3%.
- Problems: Methotrexate isn’t well-studied for AA — the evidence is primarily made up of case studies. 3-24% of patients can expect to experience side effects like mild to moderate leukopenia, thrombocytopenia, and megaloblastic anemia. There is also the risk of liver fibrosis, with an incidence ranging from 7% to 71.8%. Such a wide range makes the true risk hard to quantify. Myelosuppression is also a dangerous side effect and its risk associated with methotrexate use is unpredictable. Relapse rates vary from 33% to 80%, with some studies suggesting the rate is associated with how much hair is gained during treatment — more hair regrowth during treatment is associated with a lower risk of relapse after treatment.
Non-drug based treatments
Fecal microbiota transplant (FMT)
Fecal microbiota transplant (FMT) is a procedure whereby gut bacteria are isolated from a donor’s feces, purified, and then transplanted into an FMT candidate. This is the only procedure in which bacterial strains that have been lost from the gut can be reinoculated.
Currently, the procedure is elective in Europe (anyone can elect to have it performed). But in the U.S., it’s only available for chronic C. difficile infections. In the U.K., Taymount Clinic is one of the most popular worldwide-serving clinics for elective FMT.
- Best candidates: Evidence is limited but FMT has been used to treat patchy AA and alopecia universalis. May also be effective in treatment-resistant cases.
- Mechanisms of action: Unknown, but probably a normalization of the gut flora, leading to reduced autoimmune activity.
- Dosage: N/A; donor transplant is performed in one procedure, although people often elect for multiple procedures (depending on the delivery method).
- Outcomes: There are currently three case studies (studies here and here) investigating the efficacy of FMT in AA: two in alopecia universalis and one in patchy AA. Of the 3 case studies, all patients showed marked improvement following FMT — with two cases of almost full regrowth (one in universalis alopecia and one in patchy AA) and one case of partial regrowth. In all cases, this hair regrowth was sustained for at least 1.5 to 3 years. Considering the relapse of AA for most treatments is high, this sustained regrowth is promising. However, whether or not this regrowth was sustained beyond the follow-up period is unknown.
- Problems: FMT is still considered an investigative treatment in the U.S. and is, therefore, not elective for individuals with AA, unless a patient is also dealing with chronic C. difficile infection. As such, US residents wanting to explore the treatment must travel for the procedure and pay for it out-of-pocket — these costs can rack up (but may be worth it in the long run).
FMT before & after photos
Case #1: (A) 1 month, (B) 4 months, (C) 1.5 years after FMT in patchy AA
Case #2: (A) The patient’s scalp when his AA first began (B) a few months, (C) 1.5 years after FMT in alopecia universalis
Case #3: The beginning of hair regrowth after FMT in a case of long-standing alopecia universalis
Essential oils
- Best candidates: Evidence is limited, however, efficacy has been demonstrated for general AA in one study. In this specific study, the authors did not specify which kind of AA patients were dealing with.
- Mechanisms of action: Unknown, but probably a reduction in inflammation.
- Dosage: 2 drops thyme essential oil (EO), 3 drops lavender EO, 3 drops rosemary EO, 2 drops cedarwood EO diluted in 3mL jojoba oil and 20mL grapeseed oil.
- Outcomes: In this study, 54% of AA patients in the active group experienced hair regrowth over 7 months while 46% experienced no change (however, hair loss also did not get worse). A majority of these patients achieved hair regrowth in the 10-30% range, followed by 81-100%. In contrast, 78% of the placebo group did not improve, suggesting the essential oil mixture did, indeed, have an effect. It’s likely that the remaining 22% were experiencing spontaneous remission. Neither group experienced adverse side effects.
- Problems: It’s not clear just how many patients may benefit from EO application given that spontaneous resolution is a common occurrence. We see evidence of this in the placebo group, which may be a confounding factor in the measurement of treatment efficacy (since we don’t know how many in the active group would have resolved without intervention). Taking this into account, the response rate, when compared to other treatments for AA, is relatively low. Another issue is the fact that the study did not have a designated follow-up period to measure the rate of relapse. Therefore, we can’t be sure of just how effective this treatment is in the long run. Moreover, the treatment period was quite long in comparison to what is normally employed with other therapies. Given that AA can become more treatment-resistant as time goes on, using topical EOs may delay appropriate treatment and, as a result, require more aggressive therapies in the future.
Onion juice
- Best candidates: Men and women with patchy AA.
- Mechanisms of action: Unknown, but researchers believe it could work similarly to immunotherapy.
- Dosage: Application sufficient to cover the affected area(s) twice daily.
- Outcomes: This study found that patients with patchy AA were able to see hair regrowth as early as 2 weeks into the study period. Full hair regrowth was seen in 86.9% of patients after 8 weeks. Contrastingly, hair regrowth was only observed in 13% of the control group, making the findings of this study statistically significant.
- Problems: This study, unfortunately, had no follow-up period. As such, we don’t know how many patients experienced a relapse after cessation of treatment. Moreover, the smell of onion juice may make this treatment hard to adhere to long-term.
Garlic gel
- Best candidates: Men and women with mild patchy AA.
- Mechanisms of action: Unknown, but researchers believe it could work similarly to immunotherapy.
- Dosage: 5% garlic gel with 0.1% betamethasone valerate gel, twice daily.
- Outcomes: This study found that garlic was able to enhance the hair growth-promoting effects of a corticosteroid, betamethasone valerate. After 3 months, the active group was able to achieve a significant reduction of hair loss patches — more so than the corticosteroid topical alone.
- Problems: Like the onion juice study, this study (1) did not measure the rate of relapse after cessation of therapy and (2) fails to account for the smell, which may make the treatment difficult to adhere to in real-world settings.
Capsaicin
- Best candidates: Patients with patchy AA and, possibly, alopecia totalis.
- Mechanisms of action: Unknown, but researchers suspect neuroimmunological modulation in the hair follicle.
- Dosage: 0.075% capsaicin topical applied daily.
- Outcomes: Studies employing the use of capsaicin have show varying results. Some studies report the regrowth of vellus hairs, but no appreciable regrowth sufficient to justify its use over other treatments, while others report hair growth in just 3 weeks.
- Problems: Evidence suggests capsaicin may promote some degree of regrowth, but not enough to justify its use over other treatments — especially considering that AA becomes increasingly treatment-resistant over time. Thus, capsaicin use may delay appropriate treatment and, thus, increase the risk of refractory AA in the long-run.
Vitamin D repletion
- Best candidates: Patients with patchy AA and vitamin D deficiency and/or genetically reduced vitamin D receptor expression.
- Mechanisms of action: Likely a modulation of autoimmune activity in the follicle, due to vitamin D’s widespread effects on balancing the immune system.
- Dosage: For oral vitamin D use, the dosage will vary depending on the severity of vitamin D deficiency and whether your practitioner decides to opt for weekly bolus or daily doses. For topical vitamin D therapy, topical applications range from 0.005% calcipotriol twice daily to 50 micrograms/mL calcipotriol once daily.
- Outcomes: Evidence from meta-analyses show that AA patients are more likely to be vitamin D deficient than healthy controls. This would suggest that vitamin D could be beneficial to AA patients, however, no studies have been conducted to assess clinical benefit. The topical application of vitamin D-like, conversely, has been investigated as a treatment avenue. These studies show that twice daily application of various concentrations results that vary from 50% regrowth all the way to clinical remission (full hair regrowth). One study found that efficacy was associated with lower vitamin D levels at the beginning of the study, suggesting that lower vitamin D levels may be a marker of a good candidate. Additionally, one case report demonstrated full clinical remission in a patient with AA and reduced vitamin D receptor expression. Thus, AA patients with low vitamin D levels or reduced vitamin D receptor expression may have the best response to treatment. Studies also show minimal risk of adverse side effects.
- Problems: Studies do not currently show benefit in more severe cases of AA, like alopecia totalis or alopecia universalis. There is limited evidence investigating the therapeutic potential of oral supplements.
Zinc
- Best candidates: Patients with mild AA and zinc deficiency.
- Mechanisms of action: Unknown, but could be attributed to antioxidant regulation and anti-inflammatory activity.
- Dosage: Dosage depends on the severity of the deficiency, however, doses between 50 and 220mg have been used in the literature.
- Outcomes: Studies suggest AA patients have lower zinc levels compared to healthy controls. Interestingly, evidence also suggests a correlation between zinc levels and treatment resistance, meaning zinc deficiency may have an emerging role in refractory AA. However, some studies have failed to find a relationship between zinc and AA. Moreover, some studies show no benefit with zinc supplementation while others suggest zinc therapy may be beneficial in the context of mild AA with zinc levels below 70 μg/dL. Overall, the role of zinc therapy in AA is unclear other than zinc deficiency is more common among AA patients. Nonetheless, zinc repletion may confer health benefits in the presence of deficiency, even if clinical regrowth is not achieved.
- Problems: Research is mixed, with some studies suggesting benefit and others suggest a net zero effect. Thus, there is no conclusive evidence to support the use of zinc in AA.
Azelaic acid
- Best candidates: Patients with patchy AA.
- Mechanisms of action: Unknown, but preliminary evidence suggests it may act similarly to that of immunotherapy.
- Dosage: 20% azelaic acid topical applied twice daily.
- Outcomes: Evidence supporting the use of azelaic acid in patients with AA is lacking. However, one pilot study demonstrates efficacy on par with anthralin, a medication used to treat psoriasis (another autoimmune disease that affects the skin). Just over half of the patients tested achieved complete regrowth with both treatments with no report of adverse events.
- Problems: Research is limited and, as such, the true efficacy of azelaic acid is not known. Moreover, the aforementioned study did not employ a follow-up period, which is necessary to estimate the rate of relapse.
Platelet-rich plasma (PRP)
- Best candidates: Patients with ophiasis-pattern AA resistant to steroid treatment or AA patients who develop side effects with steroid treatment.
- Mechanisms of action: Unknown, possibly immunomodulatory effects.
- Dosage: 9 mL injection.
- Outcomes: In one case study of steroid-resistant ophiasis AA, a form of AA which is generally hard to treat, the patient was able to achieve regrowth by month 1 with significant regrowth by month 3. The patient reported no side effects. Another study demonstrated the superiority of PRP over steroid injections for patchy AA.
- Problems: Unfortunately, there is limited evidence available. The rate of relapse is unknown. The procedure is also costly.
Case study: ophiasis-type AA before and 3 months after PRP treatment.
Brotzu Lotion
Brotzu lotion is a topical formulated by Dr. Brotzu. It contains three main compounds: dihomo-gamma-linoleic acid, S-Equol, and propionyl-L-carnitine — ingredients designed to target inflammation and decreased blood flow in follicles.
There is currently no clinical evidence to support the efficacy of Brotzu lotion in AA. Nonetheless, some initial case studies do show promise. Take, for example, these two before-and-afters:
Brotzu Lotion: a child with alopecia universalis
And here’s a case of near-complete recovery of patchy AA in just 16 months from Dr. Brotzu’s presentation at this conference — start at 10:30):
Brotzu Lotion: alopecia areata recovery
While these are the only case studies we have pictures of, Dr. Brotzu’s patent cites more case studies. This is encouraging for AA patients — especially given it seems confer benefit even in more severe cases, of which are generally more likely to be resistant to treatment.
But it bears repeating: even Dr. Brotzu has claimed it’s difficult to know just how effective the lotion is for AA – mainly because of the spontaneous recoveries.
Helminthic therapy
Helminths, better known as hookworms, are tiny parasites that embed themselves in the small intestines of their hosts.
Helminths are unique in that they have a novel survival mechanism — one that might actually to a broader, modulatory effect on the whole immune system!
The specifics? Helminths “mute” the activity of T-cells, protecting them from destruction by the host’s immune system. This is accomplished through the stimulation of Tregs, a group of cells that reduce the inflammatory potential of the immune system.
As such, in theory, T-cell activity is modulated as a whole, reducing our reactivity to other reactive compounds — including our own tissue. Because auto-reactivity to our own tissue is what mediated autoimmunity (including in AA) reduced T-cell activity may also mean a reduced risk of autoimmunity.
And though research on helminth therapy is still in its infancy, preliminary studies suggest that this evidence might just translate to real-world efficacy. In fact, the therapy has shown promise for a variety of disorders, ranging from inflammatory bowel disorders to allergy all the way to mouse models of multiple sclerosis, an autoimmune disorder.
Considering this evidence, it’s not surprising that Moises Velasquez-Manoff, a male with alopecia totalis, reported hair growth for the first time in years following his experimentation with helminth therapy. He details his experience with helminth self-infection, alongside a historical perspective of helminth eradication, in his book: An Epidemic of Absence.
While this evidence alone is certainly not enough to warrant self-experimentation with helminth self-infection, this emerging research is compelling and underscores the growing importance of the symbiotic relationship of humans and microbes.
Success rates
As seen in the outcomes of the different studies, the likelihood of significant (or complete) recovery is relatively high. And, again, a large proportion of AA patients (34-50%) will spontaneously recover within one year.
This is great news! But, it also makes it difficult to effectively estimate the true success rate of treatments. So, is there any way that someone with AA might be able to gauge their likelihood of recovery (or lack thereof)?
Yes. In clinical practices, there are criteria for AA known as “poor prognostic factors” – i.e., things that might make you less likely to experience full hair recovery. According to the literature, these include:
- Bald patches that persist for longer than 1 year.
- Onset of hair loss before puberty.
- A family history of AA.
- Ophiasis pattern of AA.
- Associated nail changes, a.k.a when nail changes occur alongside AA.
- Atopy, a.k.a a propensity to developing allergic diseases like eczema, asthma, and allergic rhinitis.
So, if you fit into these categories, chances are your AA might be more treatment-resistant. That being said, it doesn’t mean you can’t recover your hair; it just means that you may need to explore more treatment avenues (or combination therapies) to find what works for your hair loss specifically. Your practitioner can help guide you through identifying these treatment avenues.
With that, you’ll also want to consult your doctor early into the process – as treatment resistance can increase as the condition progresses. As such, it’s better to forego experimental / home remedies and begin a treatment plan right away.
This isn’t to say natural therapies might not be an option for you, but, rather that you should discuss the evidence of those treatments with your doctor and, if suited to you, explore the therapy under their supervision.
This will help avoid treatment resistance that may result from delayed treatment, which would partly mitigate a major poor prognostic factor that is within your control.
Summary
Alopecia areata (AA) is a form of autoimmune hair loss characterized by inflammation, exclamation mark hairs, patchy hair loss (in early stages), and hair follicle miniaturization (in later stages). The condition can progress to alopecia totalis (loss of eyebrow and eyelash hairs) or alopecia universalis (loss of hair all over the body). But in many cases, it spontaneously reverses.
An autoimmune attack near the hair follicle stem cell bulge is what triggers AA-related hair loss. This results in inflammation, stem cell dysfunction, a malformed hair follicle, and thereby thiner, brittler hair that is prone to breakage. Eventually, hair cycling also becomes dysfunctional, leading to continued hair growth dysfunction and premature hair fall.
Thankfully, a large proportion of AA cases will spontaneously resolve within a year of onset. Having said that, it’s not a guarantee. So, while “waiting it out” may mean you need no treatment at all, it also poses a risk of progression. The further AA progresses, the higher the likelihood of treatment resistance.
So, it’s important that talk to your doctor when you first notice the hair loss. The earlier you catch it, the better your chances of regrowth. This is especially true if:
- Your hair loss began before puberty
- You have a family history of AA.
- Your hair loss is in the “ophiasis” pattern.
- Your hair loss is associated with nail changes.
- You have concurrent atopy (eczema, asthma, allergic rhintis).
Nevertheless, a wide array of treatment options do exist — both drug-based and non-drug-based – for manageable and refractory cases alike. Generally, corticosteroids are one of the first-line treatments. When corticosteroids aren’t effective, immunotherapy, methotrexate, JAK inhibitors, and alternative treatments (aromatherapy, vitamins/minerals, microbial modulation, and more) are usually explored.
Overall, the prognosis for most AA patients is good. Having said that, the risk of relapse is still high. This is mainly attributed to the fact that most treatments are confined to suppressing the signaling that leads to AA hair loss, as opposed to mitigating the root cause of AA. We just don’t know enough about the origin of AA to target these causes (yet).
The one exception to this rule might be fecal microbiota transplants (FMT) — a treatment that has shown major hair recoveries for long-standing AA patients (who typically don’t respond well to treatment), and no signs of relapse for those responders (at least within study windows of 1.5 to 3 years). However, evidence on FMT is incredibly limited. Moreover, the treatment is currently not readily accessible in the US (unless you have AA and you’re seeking treatment for a chronic C. difficile infection).
Overall, hair regrowth is absolutely possible for most AA patients — whether through natural or conventional means. Just make sure to get in touch with a doctor as soon as you notice your hair loss, so that they can help direct a treatment plan that’s going to be best suited to your condition.
If you have any questions, please feel free to leave them in the comments!
Scarring alopecias make up about 7% of patients seen in hair loss clinics. This means almost 1 in 10 hair loss cases are attributed to scarring alopecia.
In this article, we’ll outline what scarring alopecias are, what makes them unique, and why they might develop. Then we’ll uncover why this classification of hair loss – scarring vs. non-scarring – might be a bit outdated.
Finally, we’ll reveal new research that’s changing the way we think about scarring forms of hair loss. Historically, scarring alopecias have been considered irreversible. But new case reports are showing just the opposite: that some people with scarring alopecias can achieve significant – and sometimes complete – hair regrowth.
We’ll dive into why this is important, how this may impact treatment avenues, and what you can do to start combatting the progression of scarring alopecias today, both naturally and conventionally.
What are scarring alopecias?
Scarring alopecias are an umbrella term for hair loss from the rapid destruction and scarring of hair follicles.
There are several types of scarring alopecias (1), and each type varies by its presentation and causes:
- Central centrifugal cicatricial alopecia (CCCA). A type of hair loss that occurs predominantly in African American women. Characterized by a progressive thinning that begins in the center of the scalp and gradually expands to the peripheral regions. The only feature that distinguishes it from female pattern hair loss is the lack of visible follicles in the affected areas and a shiny, smooth scalp. It was once believed to be caused by hair styling techniques; however, recent data (2) has refuted that claim.
- Frontal fibrosing alopecia. This type of scarring alopecia occurs in a band-like distribution in the front of the hair and may also be present in the eyebrows. It mostly affects postmenopausal women. It predominantly affects the hairline, leading to uniform recession as if the hairline marched backward.
- Lichen planopilaris. Patchy hair loss with itchiness, scaling, and visible redness in affected areas. It might also affect non-scalp areas. It sometimes presents as diffuse thinning.
- Chronic cutaneous lupus erythematosus. Patchy, scarring hair loss as a result of an autoimmune disorder: lupus. Onset of this type of scarring alopecia may result from UV exposure, though research hasn’t yet confirmed this.
- Pseudopelade of Brocq. Small and/or large irregular patches of hair loss with no signs of inflammation.
- Folliculitis decalvans. A single patch of hair loss that progressively expands. Typically found on the peripheral regions of the scalp. Affected areas may have pustules, honey-colored crusting, and tufting.
- Dissecting cellulitis of the scalp. Multiple, red, inflamed, and interconnected nodules that erupt from various scalp regions in somewhat of a web-like pattern. It may also be associated with acne conglobota.
How do scarring alopecias happen?
No one is quite sure. However, many researchers believe scarring alopecias are caused by an interaction between inflammation, our immune systems, and (potentially) our hormones.
Similar to other hair loss disorders, the step-process for developing a scarring alopecia seems to be:
Inflammation >> scarring >> hair loss
You might see this step-process and think it looks a lot similar to other hair loss disorders, like androgenic alopecia (AGA). At face-value, you’re right. But there are a few differences that make scarring alopecias unique.
- In scarring alopecias, the location of inflammation is in the hair follicle stem cell bulge; in androgenic alopecia, it’s in the infundibulum (upper third of the hair follicle) and likely deeper below the hair follicles, but above the galea aponeurotica.
- In scarring alopecias, the nature of inflammation in unknown and/or autoimmune-related; in androgenic alopecia, the inflammation is likely related to scalp tension, pathogenic microorganisms, and accelerated hair cycling.
It might seem absurd to distinguish scarring alopecias from androgenic alopecia by the nature and location of inflammation. After all, our hair follicles are already tiny “mini-organs”. What difference does it make if one hair loss disorder’s source of inflammation is just a couple of nanometers away from another’s?
Apparently, a lot. And this is because across hair loss disorders, the location of inflammation predicts where scarring will occur, which predicts what these hair loss disorders will end up looking like.
This is why, in the later stages, androgenic alopecia and scarring alopecias look so different:
With scarring alopecias, the inflammation is far more widespread, so the scarring ends up wiping out the entire hair follicle – the stem cell bulges, sebaceous glands, arrector pili muscles, and hair shaft.
In androgenic alopecia, the scarring remains clustered around the hair follicle. Subsequently, the scarring doesn’t wipe out these other components of our hair follicles until many years into AGA’s progression.
In scarring alopecias, why do a hair follicle’s stem cell bulges become inflamed?
No one is quite sure. While researchers have identified dozens of potential triggers (3) across patients with scarring alopecias…
- Sebaceous gland dysfunction
- Substance P transmission (a neuropeptide released during stress)
- Deficiency in PPAR signaling
- Collapse of hair follicle immune privilege (the hair follicle is generally resistant against to damage by the immune system)
- Bacterial infection
- Abnormal cellular changes
- Genetic factors
- Hairstyling
- Certain drugs (anticonvulsants, hepatitis B vaccine, cyclosporin)
- Autoimmunity
- Sunscreen use on the forehead
…It’s still unclear which causes might apply to each case, why our hair follicle’s stem cell bulges become inflamed, and why this inflammation becomes persistent in the first place.
It all seems to begin with a miscommunication between an inflammatory stimulant, our immune systems, and our hair.
The miscommunication: inflammatory stimulants, myofibroblasts, and beyond
During a normal inflammatory process, the body encounters some sort of inflammatory stimulus – a wound, a virus, or even an environmental irritant. This stimulus is identified by the immune system as foreign, at which point our immune system recruits cells to “attack” the foreign invader. This leads to inflammation (i.e., tissue swelling), which in many cases, is enough to kill off the foreign invader. Once the threat is gone, the immune system signals these cells to stop attacking, and the inflammation dissipates, leaving us the same as we were prior to the attack.
In scarring alopecias, this process does not go according to plan.
During scarring alopecias, our immune system picks up on a foreign threat and sends a group of cells called myofibroblasts to start attacking. These myofibroblasts have a number of roles in the body – three of which are (1) enhancing the inflammatory response, (2) supporting the healing process, and (3) producing proteins like collagen (which, if produced in a disorganized fashion, form the building blocks of scar tissue).
Under normal settings, myofibroblasts would help enhance the inflammatory response until the foreign threat is destroyed, at which point the myofibroblasts would no longer be needed. At this point, the myofibroblasts would then help to repair the damage caused by inflammation by laying down new collagen fibers (i.e., skin tissues). Then, these myofibroblasts would die off.
However, in the case of scarring alopecias, myofibroblasts fail to die off. To put it simply, there’s a disruption in the normal cell signaling that tells our myofibroblasts that they’re no longer needed. As a result, they continue to lay down collagen, which becomes excessive and disorganized, which then turns to scar tissue.
Subsequently, functional tissue begins to be replaced by poorly-functioning scar tissue. As the fibrosis continues, the affected organs continue to lose functionality. We see this in conditions like cirrhosis, scleroderma, and pulmonary fibrosis (fibrosis of the lungs) – for example, where fibrosis makes it difficult for the liver, skin, and lungs to do their job.
This is exactly what happens in the hair follicle during scarring alopecia.
Infection and sustained inflammation begin to severely damage the hair follicle. And unfortunately, this scarring process ends up destroying our hair follicle stem cell bulges. This stem cell bulge is incredibly important; it contains the “blueprints” – or the building blocks – of each hair follicle. And without a hair follicle stem cell bulge, our hair follicles have no blueprints to follow for replication.
This leads to the complete destruction of the hair follicle… and the scarring of its surrounding skin. And as you can imagine, this is not a position most hair loss sufferers want to be in.
Are scarring alopecias reversible?
Traditionally, researchers have generally held the stance that scarring alopecias aren’t reversible.
This is because of the fact that scarring alopecias (1) lead to widespread scarring of an entire skin region, and thereby (2) wipe out the hair follicle stem cell bulges. For these reasons, many researchers have held onto the belief that scarring alopecias are irreversible – and that the best we can do is slow or stop their progression.
Encouragingly, this belief is now changing. Why? Because new evidence is showing that scarring alopecias are not only theoretically reversible, but that we actually have case studies of this happening. It’s all a matter of unlocking how to do it on a consistent basis.
Here’s why we believe this is possible.
#1: AGA, which also leads to scarring, is reversible even in its latest stages.
To reiterate from earlier, end-stage AGA closely resembles that of end-stage scarring alopecias. In both conditions, we see so much fibrosis (scarring), that there’s a total loss of follicular integrity.
Having said that, even in late stages of androgenic alopecia, we’ve seen pretty significant hair regrowth. This is obvious with examples from a few of our case studies from our membership community – like Mike and Raul – who used natural methods to see regrowth beyond what is typically observed with conventional treatments.
Mike’s Regrowth
Raul’s Regrowth
But perhaps the most impressive example of hair regrowth from advanced AGA happened entirely by accident.
In 1986, a 78-year man who’d been bald for 30+ years fell asleep in his rocking chair. Inadvertently, he slumped over, landed head-first onto hot coals, and received second degree burns across much of his scalp.
He refused to be treated at the hospital and was eventually sent home as an outpatient. Four months later, he returned for a checkup. During that time from the injury, he’d accidentally regrown his entire juvenile hairline (4).
Remember: in advanced cases of AGA, a hair follicle’s stem cell bulges appear either scarred or completely depleted. This implies an inability for hair recovery. Yet here, we see a case of complete hair recovery… just the opposite of what we’d expect.
And as we dig deeper into the research on scarring alopecias, we can find plenty of cases where recoveries happen, too.
#2: scarring alopecias have been reversed before!
There are several case studies of people with scarring alopecias regrowing significant amounts of hair. In some cases, the hair recovers completely.
In some cases, this has happened with interventions as simple as stopping the use of facial sunscreen (5). In other cases, significant regrowth came after using topical metformin (6). In one case of lupus-related scarring alopecia, complete hair regrowth was observed within three months following the use of hydroxychloroquine (7). And in cases of frontal fibrosing alopecia, oral finasteride led to near-complete hairline regrowth after just 12 months (8).
In light of these findings, there are really only two explanations:
- In scarring alopecias, stem cell bulges aren’t totally lost. Therefore, the hair is still recoverable. Or…
- Our understanding of hair follicle stem cell bulges needs to be revised. Maybe hair follicles can regenerate in the absence of stem cells, and through not-yet-discussed processes, like that of follicle-to-follicle communication.
Let’s explore that second idea for a second, as it may shape the next decade of hair loss research.
What do we know about follicle-to-follicle communication?
Follicle-to-follicle communication is a phenomenon that was originally observed in one fascinating study (9) – the findings of which we described in this article. To summarize:
In 2015, researchers wanted to see if hair follicles could communicate with each other to coordinate behaviors – like making new hair follicles. So they set up a test…
They plucked 200 hairs from the backs of mice… but did so while controlling for the diameter of a plucking region. In some cases, 200 hairs were plucked in a 2.4mm region. In other cases, 200 hairs were plucked from an 8mm region. The smaller the region, the higher-density the plucking – and vice-versa.
The goal: to see if hair follicle behavior changed on how closely hairs were plucked from one another. So they measured hair growth over the next several weeks.
The results were fascinating.
With low-density plucking, hair follicles either didn’t grow back at all… or grew back to their normal pre-plucking densities. That’s what we would expect to happen.
But with higher-density plucking, additional hair follicles were created… to the tune of a five-fold increase.
What’s more interesting is why this happened. The researchers theorized that higher-density plucking created more inflammatory signaling, which led to more cross-communication between hair follicles directly next to each other, which signaled to hair follicles to start regenerating – regardless of whether they’d been plucked.
The end-result: a huge increase in hair.
The implications? That nearby hair follicles can communicate with one another (!), and that these communications must include signaling for hair follicle regeneration. Based on this study, it’s clear that healthy hair follicles can coordinate regeneration with damaged hair follicles.
So, how does this relate to scarring alopecia?
Considering hair loss from scarring alopecia is a result of complete hair follicle destruction, and considering that this destruction has puzzlingly reversed itself across many case studies…
We can presume that follicle-to-follicle communication is playing a role here, and that understanding this role (and harnessing this cellular crosstalk) is probably one way people with scarring alopecias can unlock huge hair recoveries.
So, how do we do this?
We don’t yet know! Research is still emerging, and as it continues to evolve, we’ll update this article.
In the meantime, there’s plenty we can do to stop the progression of scarring alopecias – and potentially even see major recoveries.
What are the current treatments for scarring alopecias?
Step 1: connect with a dermatologist
The first step is always making an appointment with a dermatologist. By understanding what kind of scarring alopecia you have, you can better target your treatment regimens to save yourself time, effort, and money.
Step 2: identify and remove any potential inflammatory “triggers”
Once you’ve scheduled your appointment, one of the most critical next steps is to make your best effort to identify and remove some of the most common triggers of scarring alopecias. This will be highly individual and dependent, again, on the type of scarring alopecia with which you’re diagnosed.
Here are a few of the common inflammatory stimulants suspected in scarring alopecias:
- Sunscreen use: there is a weak link between sunscreen use and frontal fibrosing alopecia (FFA) (5). Some researchers hypothesize this could be due to decreased sebum production during the time in which a woman is most likely to be affected by FFA, menopause. This results in an inability to clear topical products, like sunscreen, from the follicle, potentially leading to an autoimmune reaction. Other researchers have proposed an alternate view: with the anti-inflammatory, immunomodulatory effects of UV light, blocking UV light (using sunscreen) may actually encourage autoimmunity in the follicle. Cessation of sunscreen use has been shown to produce noticeable regrowth in as little as 6 months with an almost full recovery in 36+ months.
- Hairstyling: While studies have failed to establish hairstyling as the sole cause of CCCA, certain hairstyling techniques may contribute to at least some cases of scarring alopecia. If you find yourself dealing with a potential case of scarring alopecia and you regularly receive hair relaxant treatments, employ hot combing, or style your hair in braids, cornrows, or using other traction styling methods (10) – it might be best to avoid these treatments and/or stylings (or at least reduce their frequency) until you can rule out their potential involvement.
- Environmental toxins as inducers of autoimmunity: Autoimmunity is one of the purported causes underpinning the development of scarring alopecia. This is due to the fact that the stem cell bulge of the follicle is normally a site of immune privilege, meaning it is usually protected from the action of the immune system. However, autoimmune processes can actually cause this immune privilege to be lost. Interestingly, environmental toxins have the ability to induce autoimmunity. For this reason, avoidance of environmental triggers linked to autoimmunity, like rancid vegetable oils, mineral oils, and sources of heavy metals, is a good precautionary measure (11).
- UV exposure: Some causes of scarring alopecia, like chronic cutaneous lupus erythematosus, are exacerbated by UV exposure. Use of sunscreen or UV-blocking clothing/hats may be needed to prevent the worsening of lesions that contribute to hair loss.
Step 3: settle on a treatment approach
There are two ways we can approach this: drug-based treatments and non-drug treatments.
We’ve divided these interventions into their respective sections and described who these treatments might be best for, which dosages are used in the literature (where applicable), the outcomes of the research, and what potential issues might arise with each given treatment.
Drug-based treatments
Topical, intralesional, and oral corticosteroids:
- Best candidates: Most forms of scarring alopecia, patients with CCCA not related to traumatic hair styling.
- Dosages: 10mg/mL for intralesional injections every 6-8 weeks; 25-40mg per day for 2-4 months with oral corticosteroids (1).
- Outcomes: Corticosteroid treatment, in any form of administration is mostly limited to halting the progression of disease as it doesn’t address the scarring that impedes hair follicle regeneration. Can promote regrowth in some patients with dissecting cellulitis (12).
- Problems: Oral corticosteroids are limited to severe/rapidly progressing disease; topical corticosteroid treatment can result in skin atrophy, a.k.a thinning of the skin.
Hydroxychloroquine:
- Best candidates: Patients with frontal fibrosing alopecia, lichen planopilaris, and chronic cutaneous lupus erythematosus.
- Dosages: Below 7.5/mg/kg for lichen planopilaris and frontal fibrosing alopecia, 400mg daily during summer months with chronic cutaneous lupus erythematosus and smaller doses during winter (1).
- Outcomes: Effective at decreasing signs and symptoms of lichen planopilaris and frontal fibrosing alopecia and preventing further hair loss, effectively resolve lesions related to chronic cutaneous lupus erythematosus (13), full hair regrowth has been observed with hydroxychloroquine in at least one case of lupus-related alopecia (7).
- Problems: Studies are often too short to estimate the true incidence of retinopathy at dosages used for these conditions.
Antibiotics (Minocycline, rifampicin, fusidic acid):
- Best candidates: Patients with folliculitis decalvans.
- Dosages: 300mg rifampicin 2x daily (should not be used as a monotherapy, which can promote antibiotic resistance), combination of 300mg rifampicin, 300mg clindamycin, and fusidic acid along with topical corticosteroid lotion for 3 months has been used with success, topical clindamycin or benzoyl peroxide can control mild cases, oral antibiotics are needed for more severe cases (1).
- Outcomes: Effective at addressing the infection that leads to folliculitis decalvans, but not restoring the hair lost.
- Problems: Rifampicin is the preferred antibiotic because it is highly lipid-soluble (the scalp environment is very lipidic) and accumulates in high quantities in the hair follicle, however, antibiotic resistance is a major issue with its use.
Topical metformin:
- Best candidates: Who topical metformin might be best for is still unclear, as research is preliminary, but case studies have demonstrated success in CCCA patients (6).
- Dosages: 10% topical metformin with the potential for higher concentrations if the patient responds well to the treatment.
- Outcomes: Although research is preliminary, there have been two cases of partial regrowth in CCCA – traditionally believed to be irreversible (and notoriously difficult to treat) (6).
- Problems: Preliminary research suggests there is little to no systemic side effects. Instead, side effects are usually superficial and limited to scalp dryness and irritation.
Oral Isotretinoin (Accutane®):
- Best candidates: Patients with dissecting cellulitis and cases of chronic cutaneous lupus erythematosus resistant to antimalarial therapies like hydroxychloroquine.
- Dosages: 0.5-1mg/kg daily for dissecting cellulitis (1).
- Outcomes: Usually produces rapid results in chronic cutaneous lupus erythematosus, treatment for 6-11 months in dissecting cellulitis shrinks lesions and can even induce periods of long remission.
- Problems: Oral isotretinoin can cause large quantities of hair follicles to prematurely enter the telogen phase, which can lead to diffuse shedding (1). The risk of disease progression should be weighed carefully against the potential risk of increased shedding.
Finasteride:
- Best candidates: Patients with frontal fibrosing alopecia.
- Dosages: 2.5mg daily (14).
- Outcomes: Some studies suggest finasteride is the most effective therapy for treating frontal fibrosing alopecia. Patients with this condition can expect a response rate of about 50% with finasteride alone (14). At least one case report demonstrated marked regrowth and a reversal of skin atrophy (i.e., skin thinning) (8).
- Problems: In women with already low or normal androgen levels, finasteride could produce sexual/mental side effects.
Non-drug treatments
Microneedling + platelet-rich plasma:
- Best candidates: Unknown.
- Methods: 20 sessions spaced 2 weeks apart.
- Outcomes: Clinical improvement in one case of general scarring alopecia – the details of this clinical improvement aren’t specified (i.e., improvement of inflammatory lesions vs. actual hair regrowth)
- Problems: Likely cannot be used to treat some forms of scarring alopecia like folliculitus decalvans, at least in their active infection phase, due to the bacterial nature of the condition.
Low level light/laser therapy (LLLT):
- Best candidates: Patients with lichen planopilaris.
- Methods: 272 pulsed laser diode cap with 1360 mW total output
- Outcomes: Case reports suggest lichen planopilaris patients may be able to achieve hair regrowth with the use of LLLT (15).
Excimer laser (UV-B light)
- Best candidates: Patients with lichen planopilaris and some cases of frontal fibrosing alopecia.
- Methods: Sessions as frequent as twice weekly with an average of 10 sessions reported in the literature.
- Outcomes: Studies have demonstrated a decrease in inflammation, as well as some instances of hair regrowth (16).
Hair Transplants
We know from the literature that there are some cases of scarring alopecia that are reversible. But, what if your hair doesn’t grow all the way back, even with the best-of-the-best treatment?
This is where hair transplants might be useful.
Hair transplants in scarring alopecias are different than hair transplants for non-scarring hair loss disorders. While grafts in non-scarring alopecias have a 90% survival rate, scarring alopecias may only have an average 50% survival rate.
But, transplants don’t have to be a stab in the dark. We can usually predict whether or not a transplant is going to be successful by (1) understanding what kind of scarring alopecia you have, and (2) performing a pre-surgery transplant test.
We’ve compiled the types of scarring alopecias that are more likely to see success from a transplant vs. those that might not:
Scarring alopecias more likely to receive transplants successfully
Scarring alopecias where hair transplants are less likely to survive Central centrifugal cicatrial alopecia (CCCA) Lichen planopilaris Discoid lupus erythematosus Frontal fibrosing alopecia Pseudopelade brocq Folliculitis decalvans However, the safest way to estimate your individual tolerance to a hair transplant is to have a dermatologist perform a pre-surgery transplant test.
But, what if your chances of hair transplant survival end up being low? Or what if hair transplants are too expensive? Or too invasive? What are the options, then?
In these cases, there is one additional option.
Artificial hair integrations
For treatment-resistant and/or transplant-intolerant cases or for those who aren’t comfortable with the price or the procedure, the next best option is artificial hair integrations.
The good news is that these are inexpensive and readily accessible – and something you can begin to use right away. But, you’ll want to be absolutely sure that these integrations aren’t putting any additional strain on existing hair, as this can do more harm than good. In some cases, it may trigger a case of traction alopecia or, worse, a new case of scarring alopecia.
So, to recap, here’s a sequential approach you should consider for treatment:
- Make a dermatologist appointment to identify what kind of scarring alopecia you might have (if any).
- Identify and remove any potential triggers.
- Based on what type of scarring alopecia you have, explore some treatment avenues provided and discuss them with your dermatologist.
- If you aren’t able to achieve full recovery, explore hair transplants. Performing a pre-surgery transplant test can help you gauge whether or not a transplant will survive on your scalp.
- If you are intolerant to transplants and/or aren’t comfortable with the price or the procedure itself, artificial hair integrations are relatively inexpensive and very accessible.
Summary
Scarring alopecias are relatively uncommon; they constitute just 7% of hair loss diagnoses in hair loss clinics. Having said that, they’re characterized by aggressive scarring. This scarring leads to the destruction of skin tissue surrounding hair follicles, as well as the destruction of stem cell bulges which make hair follicles and the hair follicles themselves. Consequently, many researchers have historically considered that scarring alopecias are irreversible.
This is no longer the case. Case reports of full hair recoveries from scarring alopecias, alongside evidence that healthy hair follicles and unhealthy hair follicles can actually communicate with each other, now leads researchers to believe that scarring alopecias are reversible… we just don’t know how to do it consistently (yet).
Because scarring alopecias are less common, there are still many questions researchers have yet to answer:
- Why are some cases of scarring alopecias reversible, if all scarring alopecias are believed to result in a loss of the stem cell bulge?
- If there are at least some scarring alopecias that happen to retain stem cells, could there be an overlap in treatments with AGA? In other words, could some scarring alopecia patients benefit from AGA treatments that address fibrosis?
- If stem cells aren’t retained, is there some other regenerative process, like follicle-to-follicle communication, at play?
As researchers attempt to answer these questions, there are still some great treatments out there for scarring alopecia patients – both drug-based and drug-free, that have shown clear benefit. While most are limited to improving symptoms and slowing or halting the progression of hair loss, some patients are seeing partial and/or full recoveries.
For those who find their hair loss is treatment-resistant or want to restore hair lost to scarring alopecia, hair transplants are a decent option. However, they can be a hit or miss, being that the transplant survival rate is around 50% (vs. 90% for other hair loss types). You can maximize your chances of survival by identifying what kind of scarring alopecia you’re dealing with as well as performing a pre-surgery transplant test.
Artificial hair integrations are also a great option — and one much cheaper and more accessible than hair transplants. However, it is of the utmost importance that these are applied correctly to avoid undue strain on healthy hair (which may trigger the onset of new hair loss).
Have any questions about the new treatments for or emerging research on scarring alopecia? Please let us know in the comments section below.
References
- Filbrandt R, Rufaut N, Jones L, Sinclair R. Primary cicatricial alopecia: diagnosis and treatment. CMAJ. 2013;185(18):1579-1585. doi:10.1503/cmaj.111570
- Subash J, Alexander T, Beamer V, McMichael A. A proposed mechanism for central centrifugal cicatricial alopecia. Exp Dermatol. 2020;29(2):190-195. doi:10.1111/exd.13664
- Harries MJ, Paus R. The pathogenesis of primary cicatricial alopecias. Am J Pathol. 2010;177(5):2152-2162. doi:10.2353/ajpath.2010.100454
- Buckland R, Wilson GR, Sully L. Effect of scalp burns on common male pattern baldness. Br Med J (Clin Res Ed). 1986;293(6562):1645. doi:10.1136/bmj.293.6562.1645-a
- Robinson G, McMichael A, Wang SQ, Lim HW. Sunscreen and frontal fibrosing alopecia: A review. J Am Acad Dermatol. 2020;82(3):723-728. doi:10.1016/j.jaad.2019.09.085
- Araoye EF, Thomas JAL, Aguh CU. Hair regrowth in 2 patients with recalcitrant central centrifugal cicatricial alopecia after use of topical metformin. JAAD Case Rep. 2020;6(2):106-108. Published 2020 Jan 22. doi:10.1016/j.jdcr.2019.12.008
- Igari S, Yamamoto T. Dramatic effect of hydroxychloroquine on lupus alopecia. J Dermatol. 2018;45(2):194-197. doi:10.1111/1346-8138.14069
- Donovan JC. Finasteride-mediated hair regrowth and reversal of atrophy in a patient with frontal fibrosing alopecia. JAAD Case Rep. 2015;1(6):353-355. Published 2015 Sep 30. doi:10.1016/j.jdcr.2015.08.003
- Chen CC, Wang L, Plikus MV, et al. Organ-level quorum sensing directs regeneration in hair stem cell populations. Cell. 2015;161(2):277-290. doi:10.1016/j.cell.2015.02.016
- Herskovitz I, Miteva M. Central centrifugal cicatricial alopecia: challenges and solutions. Clin Cosmet Investig Dermatol. 2016;9:175-181. Published 2016 Aug 17. doi:10.2147/CCID.S100816
- Pollard KM, Hultman P, Kono DH. Toxicology of autoimmune diseases. Chem Res Toxicol. 2010;23(3):455-466. doi:10.1021/tx9003787
- Whiting DA. Cicatricial alopecia: clinico-pathological findings and treatment. Clin Dermatol. 2001;19(2):211-225. doi:10.1016/s0738-081x(00)00132-2
- Takezawa K, Ueda-Hayakawa I, Yamazaki F, Kambe N, Son Y, Okamoto H. Successful treatment with hydroxychloroquine for systemic lupus erythematosus with cutaneous involvement accompanied by a xanthomatous reaction. Lupus. 2020;29(1):79-82. doi:10.1177/0961203319890677
- Fertig R, Tosti A. Frontal fibrosing alopecia treatment options. Intractable Rare Dis Res. 2016;5(4):314-315. doi:10.5582/irdr.2016.01065
- Randolph MJ, Salhi WA, Tosti A. Lichen Planopilaris and Low-Level Light Therapy: Four Case Reports and Review of the Literature About Low-Level Light Therapy and Lichenoid Dermatosis. Dermatol Ther (Heidelb). 2020;10(2):311-319. doi:10.1007/s13555-020-00359-x
- Gamret AC, Potluri VS, Krishnamurthy K, Fertig RM. Frontal fibrosing alopecia: efficacy of treatment modalities. Int J Womens Health. 2019;11:273-285. Published 2019 Apr 29. doi:10.2147/IJWH.S177308
Oral minoxidil for women with hair loss: an underutilized treatment?
Although topical minoxidil seems to get most of the attention as a hair loss treatment, its oral counterpart is also effective at promoting hair regrowth in both males and females.
Generally, higher dosing means better efficacy, but with a higher risk profile. As it relates to oral minoxidil, this means limb swelling, low blood pressure, and, potentially, heart palpitations. But, there’s one side effect that may be more concerning for women taking oral minoxidil than men: excessive body hair growth.
Considering this is something most women want to avoid or may also struggle with alongside their hair loss (in cases of female androgenic alopecia), this side effect could be of significant concern.
So, is there a way we can harness the hair-growing effects of oral minoxidil without the side effects?
Yes. This Quick Win dives into the research: the clinical evidence, the best dosages, and the best ways to avoid excessive body hair growth while taking this medication.
Note: Quick Wins are short articles focused on answering one question about hair loss. Given their specificity, these articles are written in a more scientific tone. If you’re new to hair loss education, start with these articles.
Interested in Oral Minoxidil?
Low-dose oral minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Oral minoxidil: research at a glance
What is oral minoxidil?
Oral minoxidil was initially developed as a treatment for ulcers, but later rebranded as a medication that might potentially lower blood pressure. During clinical trials, a lot of participants started reporting unexpected hair growth. This led researchers to reformulate minoxidil as a topical for hair loss, which eventually became FDA-approved in 1988.
Minoxidil’s structure
While no one is quite sure how minoxidil works to regrow hair, researchers suspect that it has something to do with minoxidil’s ability to (1) improves blood flow, and (2) increase prostaglandin E2 synthesis – a fatty acid derivative that likely plays a role in hair cycle maintenance.
Is oral minoxidil better than topical minoxidil?
Potentially. Both oral and topical minoxidil need to interact with an enzyme called sulfotransferase before becoming active and eliciting any effects on our hair follicles. Unfortunately, many men and women who are losing their hair also lack enough sulfotransferase in the scalp skin for topical minoxidil to do its job. This likely explains why for 30-40% of people, topical minoxidil doesn’t work at all (myself included).
Enter oral minoxidil. This drug is metabolized is activated in the liver – where there is plenty of sulfotransferase to go around – and then rapidly distributed to tissues throughout the body. This is why, when it comes to regrowing hair, oral minoxidil has a much higher response rate – typically 90-100%.
Unfortunately, with the rapid tissue distribution of oral minoxidil, we can also experience its hair-growing effects elsewhere in the body: namely, across our chests and faces.
This isn’t such a problem for men (in fact, many men enjoy the increased body and facial hair growth). But for women, this can be a dealbreaker – with the fear of unwanted body hair growth relegating them topical minoxidil or other treatment options.
So, for females, is there a way to mitigate any unwanted side effects of oral minoxidil while still maximizing its hair-promoting effects?
Yes.
Clinical studies
Unlike the research on topical minoxidil, oral minoxidil research is sparse (especially in women). Nevertheless, there do seem to be certain dosages of oral minoxidil – and combination therapies – that greatly reduce the risk of unwanted hair growth in women.
Here’s a table of the studies conducted on women taking oral minoxidil for hair loss.
Daily Dose (duration) Type of Hair Loss Results Side Effects 1mg daily (6 months) (1) Female Pattern Hair Loss 12% increase in hair count Limb Swelling: 4% Hypotension: 0%
Excess Hair Growth Outside the Scalp: 27%
0.25mg + 25mg spironolactone daily (12 months) (2) Female Pattern Hair Loss 72% improvement in hair loss severity Limb Swelling: Not reported Hypotension: 2%
Hives: 2%
Excess Hair Growth Outside the Scalp: 4%
0.25mg-2.5mg with most patients taking 1mg (12 months) (3) Chronic Telogen Effluvium 45% improvement in hair loss severity Limb Swelling: Not reported Hypotension: 5%
Excess Hair Growth Outside the Scalp: 38%
Looking at the results, we see that all doses of oral minoxidil are effective at promoting hair growth: 1.5-2 mg by itself, and 0.25 mg of oral minoxidil in combination with 25 mg of spironolactone (an anti-androgen drug).
When analyzing side effects, serious adverse events – like hypotension and limb swelling – are uncommon, even with doses as high as 1-2.5mg. But at these dosages, there are quite a few women (27-38%) reporting unwanted hair growth elsewhere on the body… which is exactly what we’d like to avoid.
But there’s an inflection point: a dosage that we can minimize the risk of unwanted hair growth (hypertrichosis) while maximizing oral minoxidil’s pro-hair effects on the scalp.
It’s with 0.25mg of oral minoxidil + 25mg of spironolactone daily.
With this daily dosage of oral minoxidil + oral spironolactone, only 4% of women report excess hair growth… while the majority of females in the study saw significant improvements to their scalp hair loss.
What this means: this combination therapy of low-dose minoxidil + low-dose spironolactone (an anti-androgen drug) is sort of the oral minoxidil “sweet spot” – at least in terms of lowering your risk of body hair growth, and raising your likelihood of scalp hair growth.
Low-dose oral minoxidil + low-dose oral spironolactone is a winning formula for female hair loss sufferers
But, what if you’re sensitive to spironolactone?
Although 0.25 mg of oral minoxidil alongside 25 mg of spironolactone daily might be a viable option for many women with hair loss, spironolactone can cause mild allergic reactions in sensitive individuals. (4, 5) While these effects are rare, we have had some members of our community echo these concerns and even report adverse reactions of their own.
So, maybe you’ve found that you’re sensitive to spironolactone and that combining low dose spironolactone + oral minoxidil isn’t an option for you. What’s the next best option?
At this point, it really depends on what your tolerance for higher dosages of oral minoxidil (and their potential for side effects). Higher doses of 1mg to 2.5mg will likely provide results, but also increase your risk of body/facial hair growth.
If you have milder hair loss or really aren’t comfortable with increased body/facial hair (or don’t want to manage it with other therapies), you can always start with 0.25mg of minoxidil on its own. If it still isn’t providing the results you’re looking for, you can always look into alternative oral or topical therapies to bolster your results. As always, discuss your options with your doctor before doing anything.
You may also decide to implement totally different therapies. After all, many females have seen success treating hair loss outside of the drug model, and with therapies like:
…and more. So, before you jump on any treatment, make sure that you have a firm understanding of 1) the drivers of your hair loss, and 2) your treatment options. Then, make an action plan for hair recovery that’s tailored to your needs and preferences.
What’s the bottom line?
If you’re a female with pattern hair loss, and your goal is to maximize the hair-promoting properties of oral minoxidil while minimizing your risks of hypertrichosis, research shows that combining 0.25mg of oral minoxidil with 2.5mg of spironolactone is likely your best option. At these dosages, you’re positioning yourself for scalp hair growth while minimizing the risk of body hair growth.
If spironolactone isn’t an option for you, that’s okay. Higher doses of oral minoxidil (1-2.5mg) don’t present with any increased risk of hypotension or limb swelling, but at these dosages, 27-38% of women do report excess body/facial hair growth in clinical studies. If this is a concern for you, consider combining low-dose oral minoxidil with alternative therapies or opting for another treatment altogether.
Lastly, oral minoxidil is a prescription medication. So be sure to consult your doctor before doing anything.
Question? Comments? Please reach out in the comments section.
References
- Ramos, Paulo Müller et al. Minoxidil 1 mg oral versus minoxidil 5% topical solution for the treatment of female-pattern hair loss: A randomized clinical trial. Journal of the American Academy of Dermatology, Volume 82, Issue 1, 252 – 253
- Sinclair, R.D. (2018), Female pattern hair loss: a pilot study investigating combination therapy with low‐dose oral minoxidil and spironolactone. Int J Dermatol, 57: 104-109. doi:1111/ijd.13838
- Perera E, Sinclair R. Treatment of chronic telogen effluvium with oral minoxidil: A retrospective study. F1000Res. 2017;6:1650. Published 2017 Sep 6. doi:10.12688/f1000research.11775.1
- Alonso JC, Ortega FJ, Gonzalo MJ, Palla PS. Cutaneous reaction to oral spironolactone with positive patch test. Contact Dermatitis. 2002;47:178–9.
- Corazza, M., Strumia, R., Lombardi, A.R. and Virgili, A. (1996), Allergic contact dermatitis from spironolactone. Contact Dermatitis, 35: 365-366. doi:1111/j.1600-0536.1996.tb02421.x
Ketoconazole shampoo is an anti-fungal, anti-inflammatory shampoo that is sometimes used to treat androgenic alopecia (AGA).
There are two formulations of ketoconazole shampoo: 1% and 2%. While 1% ketoconazole is sold over-the-counter as an ingredient in many hair loss shampoos, only 2% ketoconazole is clinically shown to improve pattern hair loss. And unfortunately, 2% ketoconazole requires a prescription from your doctor.
This leads a lot of pattern hair loss sufferers to opt for 1% ketoconazole shampoo, and mainly out of convenience. But if you’re opting for 1% ketoconazole instead of 2%, are you selling yourself short any potential hair gains?
More specifically, when it comes to 1% versus 2% ketoconazole for hair loss, does one percentage point really matter?
This Quick Win dives into the studies on ketoconazole to answer this question.
Note: Quick Wins are short articles focused on answering one question about hair loss. Given their specificity, these articles are written in a more scientific tone. If you’re new to hair loss education, start with these articles.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Is 2% ketoconazole better than 1% ketoconazole?
Currently, there are no studies directly comparing 1% to ketoconazole to 2% ketoconazole in their ability to promote hair growth.
However, we can look at some different studies that use either formulation and compare how each one performs in its respective studies. Then, we can compare the results of each study to get a feel for which one is more effective.
First, let’s look at 2% ketoconazole. This study investigated 2% ketoconazole’s ability to increase hair counts in AGA patients. They found that, after 6 months (and 3x per week of use), participants experienced an average 18% increase in hair count.
Now, let’s evaluate 1% ketoconazole. This study looked at the effectiveness of 1% ketoconazole for AGA. After 6 months of use 3x per week, 1% ketoconazole didn’t increase hair count, but it did decrease hair shedding. In other words, 1% ketoconazole is effective enough to slow or stop shedding, but not to promote hair regrowth.
Both studies employed the same frequency for the same amount of time and on subjects with the same condition. Because of this, we can assume that ketoconazole at a 2% concentration is likely more effective than at 1%.
An additional study also compared 1% versus 2% ketoconazole in their ability to combat the scalp yeast Malassezia and the condition seborrheic dermatitis. Malassezia overgrowths and seborrheic dermatitis are often observed alongside pattern hair loss. These conditions lead to excessive sebum production and scalp flaking (i.e., dandruff), and thereby may accelerate AGA by increasing overall scalp inflammation. Moreover, there’s also research suggesting that resolving Malassezia overgrowths and seborhheic dermatitis may enhance hair regrowth. Long-story short: if we’re going to use a ketoconazole formulation for hair loss, it only benefits us if that formulation also improves these conditions.
The findings from that research team? When it came to decreasing Malassezia load and scalp flakiness from seborrheic dermatitis, 2% ketoconazole outperformed 1% ketoconazole in both categories. Moreover, 2% ketoconazole led to fewer relapses of either condition.
“During follow-up [ketoconazole] 2% showed a trend to fewer relapses than [ketoconazole] 1%. [Ketoconazole] 2% had superior efficacy compared to [ketoconazole] 1% in the treatment of severe dandruff and scalp seborrhoeic dermatitis”
So, in summary: yes, there is evidence to suggest that when it comes to improving pattern hair loss, 2% ketoconazole is more effective over a six-month period versus 1% ketoconazole. The one percentage point difference does matter.
The questions then becomes: why?
Why is 2% ketoconazole better than 1% ketoconazole?
Ketoconazole is suspected to work in three ways to slow/stop hair loss and promote hair regrowth. The drug:
- Reduces inflammation related to microbial activity on the scalp.
- Reduces levels of dihydrotestosterone, the most powerful male hormone and the culprit behind AGA.
- Prolongs the anagen phase (i.e., growing phase) of the hair cycle, thereby reducing excessive shedding.
We don’t exactly know why 2% ketoconazole is better than 1% ketoconazole. But, chances are that the 2% dilution simply accomplishes these things more effectively and (maybe) more rapidly, meaning that it:
- Kills off more Malassezia, resulting in a more dramatic reduction in inflammation.
- Reduces scalp DHT more effectively and more rapidly, preventing further follicle miniaturization in AGA.
- Stimulates the transition to the anagen phase faster, thereby halting shedding and promoting hair regrowth in a shorter amount of time.
But with increasing efficacy, drugs often come with an increased risk of side effects. This is why clinical researchers often test several dilutions and doses of any drug: they’re trying to uncover which dilution or dose maximizes clinical efficacy while minimizing the risk of side effects.
So, with 1% versus 2% ketoconazole, does the increased concentration lead to an increased risk of side effects?
Does a 2% ketoconazole have a higher risk of side effects compared to 1% ketoconazole?
Although oral ketoconazole comes with significant side effects, these same side effects haven’t been reported with topical ketoconazole or ketoconazole shampoos.
This is because topical and shampoo formulations of ketoconazole are metabolized rapidly within the skin tissues, so very little (if any) topical ketoconazole actually reaches the bloodstream.
On that note, research continues to demonstrate that for the overwhelming majority of people, both 1% and 2% topical ketoconazole concentrations do not come with a notable risk of side effects.
Some individuals may experience a hypersensitivity reaction to ketoconazole topicals, however, this is relatively rare.
That being said, there is a small risk associated with the formulation of a 2% ketoconazole topical cream containing sodium sulfite. But this is a risk with the sodium sulfite, not the ketoconazole itself. And to be clear: sodium sulfite is not a standard ingredient in ketoconazole shampoo formulations (which are the ones prescribed for hair loss); it’s typically only found in topical formulations used to treat conditions like acne.
The bottom line: ketoconazole is rapidly metabolized in the skin, and therefore has minimal risks of side effects. This is why its 1% shampoo formulations are sold over-the-counter.
Should you use a 2% ketoconazole shampoo or topical?
Much like comparative studies between 1% and 2% ketoconazole, no studies have been conducted to assess whether a shampoo or a leave-on topical is more effective for hair growth.
But for now, the 2% shampoo formulation is probably the best way to go, and for two reasons:
- Topical ketoconazole hasn’t been studied for hair loss
- Topical ketocoanzole is not easy to find
In other words, 2% ketoconazole shampoo has several clinical studies demonstrating its efficacy, whereas topical ketconazole has only been evaluated in very small clinical studies (i.e., 6 participants), and typically for conditions like acne (not hair loss).
Moreover, 2% ketoconazole shampoo is readily available – all you need is a prescription from your doctor. Topical ketoconazole is typically only sold for research purposes. And while topical ketoconazole would remain on the skin for longer (and thereby potentially have a greater effect on the hair follicles), we don’t think the potential additional benefits of topical ketoconazole outweigh the risks associated with acquiring and using it.
And with 2% ketoconazole shampoo consistently demonstrating a significant benefit for AGA sufferers, it makes the most sense to opt for what we already know is safe and works.
2% ketoconazole shampoo: clinical efficacy for pattern hair loss
- This study demonstrated that a 2% ketoconazole shampoo improves hair counts in men with AGA. It also found that 2% ketoconazole is nearly twice as effective as minoxidil.
- This study compared a few singular and combination therapies: minoxidil alone, finasteride alone, minoxidil + finasteride, and 2% ketoconazole shampoo + finasteride. Although the minoxidil + finasteride combination outperformed the ketoconazole + finasteride combination, it demonstrates that 2% ketoconazole can enhance finasteride’s benefits.
- This study found that 2% ketoconazole shampoo works well in combination with finasteride in minoxidil. Participants experienced hair regrowth in as little as 30 days.
The verdict: opt for a 2% ketoconazole shampoo
The available evidence suggests that when it comes to treating pattern hair loss (AGA), a 2% ketoconazole shampoo produces better, more rapid results than a 1% ketoconazole shampoo.
Yes, you’ll need to get a prescription for 2% ketoconazole. Yes, this requires an appointment with a doctor. And yes, this is a hassle. But in all likelihood, the benefits of 2% ketoconazole outweigh the convenience of the 1% formulation.
Questions? Comments? Please reach out in the comments section.
This article explores the characteristics, causes, and unknowns of pattern hair loss – also known as androgenic alopecia (AGA).
If you’re new to hair loss research, this is a good starting point to learn the science behind AGA as well as the concepts that come up frequently in the literature.
- Hair follicle miniaturization
- Telogen:anagen ratios
- Dihydrotestosterone, 5-alpha reductase, androgen receptors, and androgen receptor co-activation
- Prostaglandin activity
- Wnt-ß catenin pathways
- Future research focuses: olfactory receptors, galea interaction, and more
After all, the better we understand a condition, the better equipped we are to treat it.
We’ll explore how the interplay between genetics and male hormones may lead to hair follicle miniaturization. Then, we’ll reveal what still puzzles researchers about AGA, despite 50+ years of study.
Finally, we’ll dive into more recent evidence on AGA that is paving a new direction of research – and reshaping the future of treatments.
Interested in Topical Finasteride?
Low-dose & full-strength finasteride available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

What is androgenic alopecia?
Androgenic alopecia (AGA), also known as pattern hair loss, is one of the most common hair loss disorder in the world. It’s chronic, progressive, and affects up to 50% of women and 80% of men at some point in their lives. In the U.S. alone, 30 million women and 50 million men are dealing with AGA that is severe enough to become diagnosable (NIH).
What does AGA look like?
AGA can occur both in men and women, but it manifests differently between the two sexes.
In men, classic pattern balding appears as:
- Recession of the hairline at the temples
- Loss of hair at the vertex (crown)
Norwood-Hamilton Scale (Male Pattern Hair Loss)
However, female pattern hair loss can present in a few different ways (Herskovitz et al., 2013):
- Diffuse, even thinning of the crown with preservation of the front hairline
- Christmas tree-pattern hair loss, with a widening of the scalp beginning at the front and tapering towards the crown
- Thinning at the temples
Ludwig Scale (Female Pattern Hair Loss)
What are the hallmark characteristics of AGA?
AGA has specific features that distinguish it from other types of hair loss.
For starters, it primarily affects hair at the top part of the scalp – above the galea aponeurotica (the dense fibrous membrane that stretches across the top of the scalp).
Secondly, scalp regions affected by AGA show three defining characteristics of the condition:
- Hair follicle miniaturization
- Increased telogen:anagen hairs
- Shortened anagen cycling
Each of these phases are covered below.
Hair follicle miniaturization
Follicle miniaturization is unique to AGA. It is a process by which AGA-affected hair follicles progressively get smaller until they produce fewer hairs. The hairs that are left may transition into fine, wispy hairs – known as vellus hairs.
Hair follicle miniaturization: a defining characteristic of AGA
While the causes and step-processes of hair follicle miniaturization are still debated, this process is often accompanied by histological (i.e. structural) changes – particularly to the tissues surrounding these hair follicles.
In fact, researchers believe these structural changes help to explain why pattern hair loss is a progressive condition – as they limit miniaturized hair follicles’ capabilities of returning back to full-size. They are:
- Dermal sheath thickening
- Perifollicular fibrosis
Both of these histological changes can be considered forms of scarring.
Dermal sheath thickening and perifollicular fibrosis
Dermal sheath is a term used to describe the skin tissues that surround our hair follicles. Dermal sheaths are comprised of collagen (i.e., skin), blood vessels, sweat glands, lymphatic networks, and more.
In men and women with AGA, dermal sheaths surrounding miniaturizing hair follicles have thickened. Specifically, their collagen bundles are up to 2.5 times larger – a characteristic of early scar tissue development (Jaworsky et al., 1992).
As dermal sheaths thicken, they widen into the space occupied by hair follicles – thereby impeding their growth space. And as AGA progresses, these dense collagen bundles turn into scar tissue – also known as perifollicular fibrosis.
Together, dermal sheath thickening and perifollicular fibrosis restrict the growth space of surrounding hair follicles, which creates a spacial barrier for miniaturizing hair follicles to recover back to their original size.
Fibrosis (scar tissue) surrounding an AGA-affected hair follicle
Dermal sheath thickening is consistently observed in AGA. However, its advancement to perifollicular fibrosis has been found, according to some studies, in over 71% of AGA sufferers – with moderate levels observed in at least 37% (Whiting et al., 1996).
By progressively restricting the growth space of miniaturizing hair follicles, these histological changes also explain the chronic, progressive nature of AGA – along with why most treatments are limited mainly to stopping the progression of pattern hair loss rather than fully reversing it (English, 2018).
Hair follicle miniaturization is a hallmark of AGA. This is when the size of each hair follicle shrinks and thus starts producing smaller, wispier hairs.
This process is accompanied by dermal sheath thickening around miniaturizing hair follicles. This skin thickening is an early step-process of scarring. In later stages of AGA, this turns to perifollicular fibrosis.
Dermal sheath thickening and perifollicular fibrosis prevent AGA-affected hair follicles from rebounding to their full size. They help to explain the chronic, progressive nature of AGA.
Increased telogen:anagen ratio
Beyond hair follicle miniaturization, the second defining characteristic of AGA is an increase in telogen versus anagen hairs.
Telogen and anagen are terms used to describe specific stages of the hair cycle.
The hair cycle is the natural, ever-repeating cycle of regeneration and degeneration of hair follicles. A hair grows, stops growing, and eventually falls out – at which point a new hair follicle reforms and a new hair starts growing again. In human scalps, these hair cycles last between two to seven years.
The Hair Cycle
In non-balding scalps, 80-85% of scalp hairs are in their growth (anagen) phase, 1-2% have stopped growing and are in their resting (catagen) phase, and 10-15% have already fallen out and entered their shedding (telogen) phase.
In healthy scalps, this cycle repeats indefinitely. Thus, many hair loss disorders can sometimes be identified by measuring the number of shedding versus growing hairs – and then comparing that ratio to what is seen in normal scalps. If the ratio is high, this suggests abnormal hair loss. If it’s low, this suggests normal, healthy hair.
This is the telogen:anagen ratio.
In normal scalps, there is generally one telogen hair for every 12 anagen hairs, or a 1:12 ratio.
However, in men with AGA, the telogen:anagen ratio can exceed 1:4 (or 25%). In women, this ratio often exceeds 2:5 (or 40%).
Shortened anagen cycling
Moreover, in balding scalps, the anagen phase of a miniaturizing hair is shortened. This means that rather than growing for 2-7 years, these hairs may only grow for a few months (Ho et al., 2019).
This is why so many AGA-affected men and women notice short terminal hairs near their hairline or vertex – hairs that won’t grow more than a few inches. This is the result of a shortened anagen phase and an increased telogen:anagen ratio.
In AGA, balding regions have an elevated ratio of shedding to growing hairs. This is called the telogen:anagen ratio.
While healthy scalps have a telogen:anagen ratio of 10-15%, balding regions will have a ratio of 25-40%, and sometimes higher.
Moreover, growing (anagen) hairs in balding regions often do not grow for more than a few months. This is called a shortened anagen phase. This helps to explain why so many balding men and women see shorter hairs in balding regions that never reach more than an inch or two in length.
What causes AGA?
While the exact step-processes of AGA aren’t yet determined, there is general consensus on two contributing factors: genetics and androgens (i.e., male hormones).
Genetics
AGA has an undisputed genetic component, with one study measuring a 2.5-fold increased risk of developing pattern hair loss in men whose fathers had pattern hair loss, as compared to those whose fathers didn’t (Chumlea et al., 2004). Moreover, women affected by AGA often report having other family members affected by the same condition (Ramos et al., 2015).
However, the exact genes involved in androgenic alopecia have not yet been discovered.
In fact, research suggests that there is no one gene involved in AGA. Rather, pattern hair loss is likely a polygenic disorder, meaning there are many gene variances that are involved in the predisposition of its development.
Scientists are still trying to uncover which polymorphisms may prompt individual susceptibility to AGA. Particular focus is on genes that code for androgen receptors (more on this soon).
Androgen activity
Male hormones (i.e., testosterone) are closely tied to AGA. In the 1940’s, researchers observed that (Hamilton et al., 1942):
- Men castrated before puberty (i.e., before their sex hormones spike) never develop AGA later in life.
- Men with AGA who are castrated (and thereby lose 95% of androgen production) also see a stop in AGA progression.
- Castrated men who are injected with testosterone begin to develop temple recession and/or vertex thinning.
Thirty years later, scientists uncovered the specific male hormone involved in AGA: dihydrotestosterone (DHT).
DHT: the main hormone implicated in pattern baldness
Dihydrotestosterone (DHT)
DHT – a metabolite of testosterone – is causally linked to pattern hair loss (English, 2018).
- Men who cannot make scalp DHT never develop AGA.
- Balding scalp regions have higher amounts of DHT versus non-balding regions.
- Drugs that reduce scalp DHT improve AGA outcomes in 80-90% of men.
DHT drives part of hair follicle miniaturization
However, not all types of DHT are implicated in pattern hair loss. Rather, research is focused more so on one specific type of DHT: DHT made from an enzyme called type II 5-alpha reductase.
Type II 5-alpha reductase
In the body, nearly all DHT is created when unbound testosterone comes into contact with the enzyme 5-alpha reductase. This enzyme binds to free testosterone and then changes testosterone’s structure into DHT.
There are different types of 5-alpha reductase, and most types correspond to a specific tissue or region in which the enzyme expresses (i.e., the skin, brain, prostate, etc.).
When it comes to AGA, the type II 5-alpha reductase is most heavily implicated.
This is because (1) type II 5-alpha reductase is greatly expressed in scalp tissues, and (2) men with a gene mutation who cannot produce type II 5-alpha reductase never go bald (Adachi et al., 1970). Moreover, drugs that inhibit the type II 5-alpha reductase enzyme (i.e., finasteride) help to improve pattern hair loss in men.
Together, these findings implicate DHT and the type II 5-alpha reductase enzyme in AGA. But there’s at least one more androgenic factor involved in the onset and progression of pattern hair loss: that of androgen receptors.
Androgen receptors
When free testosterone comes into contact with type II 5-alpha reductase and converts into DHT, that DHT needs a place to bind to a cell. Once DHT is bound to a cell, this hormone can begin to influence that cell’s functionality.
Androgen receptors are where DHT binds to cells. They’re considered cellular “landing pads” – a place for male hormones to attach, so that they can begin to change cellular behavior.
That means that for (most) scalp DHT to form, we need (1) free testosterone, (2) type II 5-alpha reductase, and (3) an androgen receptor.
This is why androgen receptors are a major focus of AGA research: without androgen receptors, DHT cannot bind to scalp cells and influence their functionality.
“DHT sensitivity”
Type II 5-alpha-DHT has a 5x higher affinity for the androgen receptor than other hormones like testosterone (Trüeb, 2002). This means that in balding scalps, DHT will begin preferentially bind to androgen receptors and exert more effects on cell function, at least compared to other male hormones.
This is why some researchers speak of AGA sufferers developing a “genetic sensitivity” to DHT. In the scalp, the more type II 5-alpha-DHT bound to androgen receptors, the more likely a person is to suffer from pattern hair loss.
Is DHT also involved in female pattern hair loss?
DHT is still involved, but there’s debate over its degree of involvement.
Some studies have demonstrated that both men and women have elevated levels of 5α-reductase in the frontal hair follicles (Orme et al, 1999, Sawaya et al., 1997). This suggests that DHT may play a role in at least some female AGA cases.
At the same time, case studies have demonstrated female pattern hair loss can occur in women who are androgen-deprived, meaning they lack the ability to produce any male hormones at all (Orme et al., 1999).
While some have argued that these instances are just cases of mistaken identity (i.e., not AGA), others have used these findings as starting points to explore other aspects of AGA – and what the DHT-genetic sensitivity argument might not be telling us.
Other potential factors: prostaglandin D2, retinoid receptors, and PPAR pathways
A new wave of AGA research is focusing more so on non-androgenic factors that might influence hair follicle functionality.
In 2014, excitement was generated over prostaglandin D2 and its potential connection to pattern hair loss. Prostaglandin D2 is a fatty acid derivative that, theoretically, can express as a result of androgenic activity (i.e., DHT) (Nieves et al., 2014).
Prostaglandin D2 was once found to be elevated in balding scalp regions and even impede hair lengthening. However, follow-up studies have shown conflicting findings – suggesting that prostaglandin D2 might be less involved in AGA than initially believed (Villarreal-Villarreal et al., 2019).
Interestingly, evidence is accumulating that in addition androgenic activity, retinoid receptors and the PPAR pathway are intimately tied to hair follicle miniaturization – and may even explain why some women develop AGA despite having normal scalp DHT levels (Siu-Yin Ho et al., 2019).
Evidence implicates genes and androgen activity in the onset of AGA.
The hormone DHT is causally linked to AGA. Men who can’t produce DHT never go bald, DHT levels are higher in the scalps of balding men, and drugs that reduce scalp DHT help to stop AGA’s progression.
Scalp DHT is formed when free testosterone comes into contact with the enzyme, type II 5-alpha reductase. This enzyme converts free testosterone into DHT, and then that DHT attaches to an androgen receptor in scalp tissues – thereby influencing cell function.
For these reasons, type II 5-alpha reductase and androgen receptors have been targets of both AGA research and AGA-related drugs. Finasteride is a type II 5-alpha reductase inhibitor; spironolactone and RU58841 are androgen receptor blockers. While these drugs don’t lead to complete AGA reversals, they do seem to improve AGA outcomes.
“DHT sensitivity” is a term used to describe how, in scalp tissues, DHT might begin to preferentially bind to androgen receptors – thereby having up to 5x greater influence over these cells’ behavior than other male hormones like testosterone.
While DHT is causally linked to AGA, it’s still unclear how this hormone causes hair follicle miniaturization. Research in female pattern hair loss brings to question DHT’s involvement in AGA – and suggests that in addition to androgens, other factors must be involved.
What don’t we know about AGA?
Despite AGA’s prevalence and decades of study, there are still a lot of unknowns about this hair loss disorder.
The specific genetics involved
As mentioned, AGA is a polygenic disorder. It has been unequivocally established that male pattern baldness is more likely to occur in men whose fathers suffer from AGA.
However, recent evidence suggests that genetic variances in the gene that encodes for androgen receptors are prevalent among men with male pattern baldness (Ellis et al., 2001). Because the androgen receptor gene is located on the X chromosome, which inherited by men from their mother, this raises questions about whether or not AGA is strictly related to paternal genetics.
Even more confounding is female AGA. Of the genetic components explore in male AGA, none seem to be present in women suffering from pattern hair loss (Ramos et al., 2015).
However, some research has demonstrated is that female pattern hair loss may be associated with polymorphisms in the aromatase gene (aromatase helps synthesize estrogen). Aromatase enzymes help convert testosterone into estrogen. However, it’s still unclear how (or why) these polymorphisms impact both female pattern hair loss – especially as this hair loss disorder has been characterized as “androgenic” since the 1970’s.
From the current body of evidence, it’s almost impossible to distinguish a specific gene or set of genes that is indisputably linked to all cases of AGA.
What causes DHT to increase in balding scalp regions?
If DHT is elevated in balding scalps of most men (and some women), what causes DHT to increase in these regions? This is one question researchers are still trying to answer.
One small-scale study indicates that whole-body DHT may not be the culprit – or that AGA patients don’t seem to have elevated serum DHT versus controls (Urysiak-Czubatka et al., 2014). This gives the impression that elevated DHT in balding scalp tissue is likely a local issue, and not a systemic problem.
So, then, what causes DHT to increase in scalp tissues, specifically? Elevated 5α-reductase activity has been implicated, which explains the ability of 5α-reductase inhibitors like finasteride to halt the progression of AGA (English, 2018). However, finasteride treatment doesn’t fully reverse AGA; it generally just stop its progression.
Findings that AGA is not associated with polymorphisms in the 5α-reductase genes suggest that this enzymatic upregulation is unrelated to genetic predisposition (Ellis et al., 1998). This indicates a possible environmental factor. This assumption is supported by studies showing that in genetically identical twins, one twin can bald faster than his counterpart – despite both twins having the same sets of genes (Nyholt et al., 2003).
Although research is sparse regarding environmental factors influencing 5α-reductase activity, there are some clues.
In women with PCOS, insulin resistance is related to increased 5α-reductase activity, possibly explaining why pattern hair loss is often a feature of the disorder (Wu et al., 2017). Male AGA is also associated with insulin resistance, however, whether this is a result of enhanced enzyme activity is unclear (González-González et al., 2009).
But again, no research team has discovered a definitive answer to this question.
How, exactly, does DHT miniaturize hair follicles?
No one is sure. The closest answers we have (so far) come from DHT and its link to a signaling protein called transforming growth factor beta 1 (TGF-β1).
Follicular miniaturization, as well as dermal sheath thickening and perifollicular fibrosis, are key features of AGA. In vitro studies strongly implicate the role of a growth factor, TGF-β1, in these processes (Yoo et al., 2006).
One of TGF-β1’s primary roles in the body is promoting both wound healing and the deposition of fibrous scar tissue (Pakyari et al., 2013). Thus, elevated TGF-β1 activity is likely involved in AGA follicle miniaturization and may even contribute to the process.
TGF-β1 expression can be triggered by the binding of androgens – like DHT – to androgen receptors, and in a potentially dose-dependent manner (Yoo et al., 2006). TGF-β1 may also enhance androgen activity through an androgen co-activator, Hic-5, that allows androgens like DHT to more effectively influence gene expression, like TGF-β1, within cells (Dabiri et al., 2008).
Essentially, increased androgen activity enhances TGF-β1 expression, and TGF-β1 exacerbates androgen activity. This feedback loop creates a vicious cycle that may underpin AGA progression.
Genetically-determined increased androgen receptor expression in AGA tissue contributes to this upregulated androgen activity, but this genetic component alone isn’t enough to dictate AGA progression (Nyholt et al., 2003).
This begs the question: in AGA, what causes androgen activity to increase?
If activity is dictated by androgen availability in the hair follicle, the rate of DHT conversion by 5α-reductase (which is controlled by the number of 5α-reductase enzymes and their activity), and the involvement of co-activators, then what, beyond genetics, could trigger any one of these factors?
Future research will hopefully begin to answer these questions.
Why is DHT also associated with body and facial hair growth?
DHT is linked to hair loss in AGA scalps. But ironically, this same hormone also enhances facial and body hair growth (Thornton et al.,1993). This occurs in spite of a 3-5 times higher 5α-reductase activity in beard follicles.
Given androgens and their negative impact on hair growth in the scalp, one would assume that elevated 5α-reductase activity would result in beard hair loss, not growth. But, this isn’t true for either case. Why might this be?
Why is there a pattern to androgenic alopecia?
No one is sure. Initially, researchers thought the pattern of AGA was due to different levels of androgen activity in balding regions. However, anecdotes of females with AGA and no androgen activity have raised questions about whether this actually makes sense.
In AGA scalps, there are differences in androgen receptor density and 5α-reductase activity in balding and non-balding regions (Cranwell et al., 2016). This may be explained by in vitro research that proposes individual follicles can “self-regulate”, modulating levels of androgen receptors and 5α-reductase enzymes.
Another question is then: what triggers these follicles to self-regulate? The current state of evidence leaves the answers to these questions purely speculative.
The activation of androgen co-activator, Hic-5, also increases follicle sensitivity to androgens, allowing androgens to more effectively influence hair loss-related gene expression (Tellez-Segura, 2015). Interestingly, stretching forces on follicle cells and oxidative stress have been shown to activate Hic-5 (Kim-Kaneyama et al., 2005, Shibanuma et al., 2003).
Elevated levels of reactive oxygen species (ROS, also known as free radicals) and increased stretching forces in these localized regions may explain increased androgen sensitivity, TGF-β activity, and, thus, the patterning of AGA.
What is not known is what events may trigger increased tension or free radical concentration in these areas. There’s still much to be explored.
The current model of AGA doesn’t fully explain (1) what causes DHT to increase in balding regions, (2) how DHT actually miniaturizes hair follicles, (3) why DHT is associated with scalp hair loss, but body and facial hair growth, and (4) why there is a unique pattern and progression to AGA.
Where is AGA research heading?
As scientists try to answer these questions, they’re beginning to stumble into new (and exciting) areas of AGA research.
Wnt/β-catenin signaling
The hair cycle is a degenerative and regenerative process that requires stem cells. Without the activity of these stem cells, the hair follicle can’t properly regenerate hair or maintain the integrity of the hair follicle itself.
Each compartment of the hair follicle possesses its own stem cell reservoir from which it draws. They are used to repair the epidermis around the hair follicle following injury, maintain the structure of the hair follicle, and help regulate hair follicle cycling (Yang et al., 2010).
Wnt/β-catenin signaling is essential for this process. These pathways help with the differentiation of stem cells in and around the hair follicle.
If this signaling pathway is blocked, hair follicle shaft regeneration is impaired. Blockade of this pathway may also impede the re-entry to the anagen phase from telogen.
In AGA, elevated levels of DHT effectively stimulate androgen-related gene transcription. One of the genes that androgens regulate is dickkopf 1 (DKK-1), a direct inhibitor of the Wnt/β-catenin pathway (Kwack et al., 2008).
When DHT binds to ARs in the dermal papilla cells, it enhances the expression and secretion of DKK-1. It acts in a paracrine fashion, meaning it affects hair components outside of the dermal papilla and may impair stem cell function throughout the hair follicle.
As a result, the hair follicle loses its integrity and may become inactive. However, evidence from animal studies indicates that, thankfully, even long-term DKK-1 inhibition of hair growth may be reversible (Choi et al., 2014).
Current Model Alternative Model How do androgens cause hair loss? Genetic predispositions Increased androgen activity and genetic sensitivity work synergistically to inhibit Wnt/β-catenin signaling, preventing hair follicle regeneration and anagen re-entry. Galea interaction
The galea aponeurotica is a fibrous connective tissue that extends over the top of the scalp. It is attached to and connects all the muscles surrounding it.
The galea is a key component of the scalp tension theory of AGA. Interestingly, the “pattern” observed in AGA directly correlates to the highest points of tension in the GA (English, 2018).
Hair follicles are fashioned within both the dermis and fatty tissue beneath the skin, which is directly fused with the GA. Tension in the galea may be transmitted to these tissues and the follicles that are housed within.
Stretch-induced mechanical tension can enhance free radical production and trigger chronic inflammation in various types of tissues, potentially including the GA and the tissues that surround it. Cellular mechanical tension, free radicals, and inflammation can all enhance androgen activity and the fibrosis-mediating TGF-β1 (English, 2018).
This may, in part, explain the origin of follicle miniaturization in AGA.
Other research groups have developed similar hypotheses, arguing that fibrosis may not only drive hair follicle miniaturization, but that this process is potentially mediated by interactions between the galea and cells that transition adipose (fat) tissue into scar tissue (Kruglikov et al., 2017).
Current Model Alternative Model What causes increased androgen activity in AGA follicles? Genetic predisposition to androgen sensitivity. Mechanical stretch, free radical production, and chronic inflammation as a result of galea tension enhance androgen activity. Why is there increased androgen activity in localized regions? Genetics don’t yet offer any direct explanation. The points of highest tension within the galea directly correlate to the pattern seen in AGA. The mechanical stretch, free radical production, and chronic inflammation may all upregulate androgen activity. Why does DHT cause hair loss on the scalp but not in facial or body hair? Genetics don’t yet offer any explanation. Mechanical stretch, free radical production, and chronic inflammation as a result of GA tension trigger TGF-β1 expression that leads to follicle miniaturization. Olfactory receptors
An interesting finding of one 2018 study was the identification of OR2AT4 receptors in human hair follicles. OR2AT4 is an olfactory or smell receptor that is activated by certain scents (Chéret, et al. 2018).
In this study, researchers demonstrated that activation of this receptor by a synthetic sandalwood scent prolonged the anagen phase of the hair cycle. In fact, their findings suggest that activation of OR2AT4 may actually be indispensable for maintaining anagen.
While OR2AT4 is primarily considered an olfactory receptor activated by scent, this study also suggests that it may be activated by other compounds such as scalp microflora (bacteria) metabolites and short-chain fatty acids.
Current Model Alternative Model Inhibition of androgen activity is the best way to treat AGA. Many different cellular receptors in the hair follicle, like olfactory receptors, may help counteract the effects of androgens in the scalp. In addition to PPAR pathways and retinoid receptors – Wnt-β catenin signaling, galea interactions, and olfactory receptors may help explain much of the unexplained phenomena in AGA pathology.
What are the treatment targets for AGA?
Most AGA treatments target to (1) decrease the telogen:anagen ratio, and (2) stop the progression of hair follicle miniaturization.
There are many ideas as to how to do this, but the most successful FDA-approved approach (so far) seems to be finasteride (Propecia®), a type II 5-alpha reductase inhibitor.
1mg daily of oral finasteride reduces scalp DHT levels by 50-70%. Subsequently, it stops AGA progression in 80-90% of men and leads to a 10% increase in hair count over two years, along with some additional hair thickening (English, 2018).
However, prolonged finasteride use is sometimes associated with sexual side effects. And, when considering all of the evidence that not just androgens are involved in AGA, it’s likely that finasteride is not a complete solution.
As such, here’s a list of current treatment targets in AGA research. Many of these targets overlap with one another.
- Type II 5-alpha reductase
- Androgen receptors
- Reactive oxygen species
- Wnt-β catenin pathways
- DKK-1
- TGF-β1
- Prostaglandin analogues
- Olfactory receptors
- PPAR pathways
- Retinoid receptors
- Potassium ion channels
- Mechanical tension
- Adipose-myofibroblast transitions
- Scalp microflora
In the years to come, this list will undoubtedly grow as researchers elucidate more of the molecular mechanisms behind AGA.
The bottom line
AGA can affect men and women, in both similar and completely different patterns.
AGA is characterized by (1) an increased telogen:anagen ratio, and (2) hair follicle miniaturization. Dermal sheath thickening and perifollicular fibrosis are also present in balding regions, and may partly explain the chronic, progressive nature of AGA.
Both genetics and androgens are established as causally linked to AGA. Androgen receptor density, type II 5α-reductase activity, and DHT are elevated in balding scalps.
The DHT “genetic sensitivity” argument for AGA is incomplete, and for several reasons. (1) Elevated whole-body DHT and polymorphisms in the 5α-reductase gene are not associated with AGA. (2) Female pattern hair loss has been observed in women who cannot produce androgens. (3) More recent research now implicates non-androgenic factors like retinoid receptors and PPAR pathways in the onset of hair follicle miniaturization from AGA.
The current model of AGA doesn’t fully explain (1) what causes DHT to increase in balding regions, (2) how DHT actually miniaturizes hair follicles, (3) why DHT is associated with scalp hair loss, but body and facial hair growth, and (4) why there is a unique pattern and progression to AGA.
Wnt-β catenin signaling, galea interactions, and olfactory receptors are a few new research areas in AGA that might help explain part of the unexplained phenomenon in AGA.
(1) Wnt/β-catenin signaling regulates the stem cell activity in hair follicles needed for follicle regeneration and anagen re-entry. Androgens stimulate DKK-1 secretion by dermal papilla cells which inhibits Wnt/β-catenin signaling and impairs stem cell activity.
(2) Mechanical tension in the galea, which directly corresponds to the patterning in AGA, may play some sort of regulatory role in the inflammation, free radical production, and TGF-β1 expression that seems to mediate scarring and hair follicle miniaturization. However, research here is limited.
(3) Activation of one olfactory receptor by short-chain fatty acids, scalp microflora metabolites, and specific scents may prolong the anagen phase, providing one possible avenue for counteracting AGA progression outside of the traditional anti-androgen treatment approach.
AGA researchers are now turning focus toward non-androgenic factors – PPAR pathways, retinoid receptors, and more – to explain the unexplainable in AGA pathology. If research keeps heading in this direction, newer treatment options will likely better target AGA’s step-processes, resulting in better hair recovery and with a greatly reduced potential for side effects.
References
- NIH Androgenetic Alopecia Stats https://ghr.nlm.nih.gov/condition/androgenetic-alopecia#statistics
- Herskovitz, I., & Tosti, A. (2013). Female pattern hair loss. International journal of endocrinology and metabolism, 11(4), e9860. doi:10.5812/ijem.9860
- JAWORSKY, C. , KLIGMAN, A. and MURPHY, G. (1992), Characterization of inflammatory infiltrates in male pattern alopecia: implications for pathogenesis. British Journal of Dermatology, 127: 239-246. doi:10.1111/j.1365-2133.1992.tb00121.x
- Whiting, D. A. (1996). Chronic telogen effluvium: Increased scalp hair shedding in middle-aged women. Journal of the American Academy of Dermatology, 35(6), 899–906. doi:10.1016/s0190-9622(96)90113-9
- English, R. S. (2018). A hypothetical pathogenesis model for androgenic alopecia: clarifying the dihydrotestosterone paradox and rate-limiting recovery factors. Medical Hypotheses, 111, 73–81. doi:10.1016/j.mehy.2017.12.027
- Hoelzel, F. (1942). Baldness and calcification of the ivory dome. Journal of the American Medical Association, 119(12), 968-968.
- Ho CH, Zito PM. Androgenetic Alopecia. [Updated 2019 May 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430924/
- Chumlea, W. C., Rhodes, T., Girman, C. J., Johnson-Levonas, A., Lilly, F. R. W., Wu, R., & Guo, S. S. (2004). Family History and Risk of Hair Loss. Dermatology, 209(1), 33–39. doi:10.1159/000078584
- Ramos, P. M., & Miot, H. A. (2015). Female Pattern Hair Loss: a clinical and pathophysiological review. Anais brasileiros de dermatologia, 90(4), 529–543. doi:10.1590/abd1806-4841.20153370
- Hamilton, J. B. (1942), Male hormone stimulation is prerequisite and an incitant in common baldness. Am. J. Anat., 71: 451-480. doi:10.1002/aja.1000710306
- Adachi, K., & Kano, M. (1970). Adenyl cyclase in human hair follicles: Its inhibition by dihydrotestosterone. Biochemical and Biophysical Research Communications, 41(4), 884–890. doi:10.1016/0006-291x(70)90166-x
- Trüeb, R. M. (2002). Molecular mechanisms of androgenetic alopecia. Experimental Gerontology, 37(8-9), 981–990. doi:10.1016/s0531-5565(02)00093-1
- Orme, Cullen, & Messenger. (1999). Diffuse female hair loss: are androgens necessary? British Journal of Dermatology, 141(3), 521–523. doi:10.1046/j.1365-2133.1999.03049.x
- Sawaya, M. E., & Price, V. H. (1997). Different Levels of 5α-Reductase Type I and II, Aromatase, and Androgen Receptor in Hair Follicles of Women and Men with Androgenetic Alopecia. Journal of Investigative Dermatology, 109(3), 296–300. doi:10.1111/1523-1747.ep12335779
-
Nieves, A. and Garza, L. A. (2014), Does prostaglandin D2 hold the cure to male pattern baldness?. Exp Dermatol, 23: 224-227. doi:10.1111/exd.12348Villarreal‐Villarreal, C. , Sinclair, R. , Martínez‐Jacobo, L. , Garza‐Rodríguez, V. , Rodríguez‐León, S. , Lamadrid‐Zertuche, A. , Rodríguez‐Gutierrez, R. , Ortiz‐Lopez, R. , Rojas‐Martinez, A. and Ocampo‐Candiani, J. (2019), Prostaglandins in androgenetic alopecia in 12 men and four female. J Eur Acad Dermatol Venereol, 33: e214-e215. doi:10.1111/jdv.15479
- Siu-Yin Ho, B. et al. (2019). Progressive expression of PPARGC1α is associated with hair miniaturization in androgenetic alopecia. Nature Scientific Reports volume 9, Article number: 8771 (2019). https://www.nature.com/articles/s41598-019-43998-7
- Ellis, J. A., Stebbing, M., & Harrap, S. B. (2001). Polymorphism of the Androgen Receptor Gene is Associated with Male Pattern Baldness. Journal of Investigative Dermatology, 116(3), 452–455. doi:10.1046/j.1523-1747.2001.01261.x
- Urysiak-Czubatka, I., Kmieć, M. L., & Broniarczyk-Dyła, G. (2014). Assessment of the usefulness of dihydrotestosterone in the diagnostics of patients with androgenetic alopecia. Advances in Dermatology and Allergology, 4, 207–215. doi:10.5114/pdia.2014.40925
- Ellis, J. A., Stebbing, M., & Harrap, S. B. (1998). Genetic Analysis of Male Pattern Baldness and the 5α-Reductase Genes. Journal of Investigative Dermatology, 110(6), 849–853. doi:10.1046/j.1523-1747.1998.00224.x
- Nyholt, D.R., Gillespie, N. A., Heath, A. C., & Martin, N. G. (2003) Genetic basis of male pattern baldness. Journal of Investigative Dermatology, 121(6), pp. 1561-1564.
- Wu, C., Wei, K., & Jiang, Z. (2017). 5α-reductase activity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Reproductive biology and endocrinology : RB&E, 15(1), 21. doi:10.1186/s12958-017-0242-9
- González-González, J. G., Mancillas-Adame, L. G., Fernández-Reyes, M., Gómez-Flores, M., Lavalle-González, F. J., Ocampo-Candiani, J., & Villarreal-Pérez, J. Z. (2009). Androgenetic alopecia and insulin resistance in young men. Clinical Endocrinology, 71(4), 494–499. doi:10.1111/j.1365-2265.2008.03508.x
- Yoo, H. G., Kim, J. S., Lee, S. R., Pyo, H. K., Moon, H. I., Lee, J. H., … Cho, K. H. (2006). Perifollicular Fibrosis: Pathogenetic Role in Androgenetic Alopecia. Biological & Pharmaceutical Bulletin, 29(6), 1246–1250. doi:10.1248/bpb.29.1246
- Pakyari, M., Farrokhi, A., Maharlooei, M. K., & Ghahary, A. (2013). Critical Role of Transforming Growth Factor Beta in Different Phases of Wound Healing. Advances in wound care, 2(5), 215–224. doi:10.1089/wound.2012.0406
- Dabiri, G., Tumbarello, D. A., Turner, C. E., & Van de Water, L. (2008). Hic-5 promotes the hypertrophic scar myofibroblast phenotype by regulating the TGF-beta1 autocrine loop. The Journal of investigative dermatology, 128(10), 2518–2525. doi:10.1038/jid.2008.90
- Thornton, M. J., Laing, I. , Hamada, K. , Messenger, A. G. and Randall, V. A. (1993), Differences in testosterone metabolism by beard and scalp hair follicle dermal papilla cells. Clinical Endocrinology, 39: 633-639. doi:10.1111/j.1365-2265.1993.tb02420.x
- Rutberg, S. E., Kolpak, M. L., Gourley, J. A., Tan, G., Henry, J. P., & Shander, D. (2006). Differences in Expression of Specific Biomarkers Distinguish Human Beard from Scalp Dermal Papilla Cells. Journal of Investigative Dermatology, 126(12), 2583–2595. doi:10.1038/sj.jid.5700454
- Cranwell W, Sinclair R. Male Androgenetic Alopecia. [Updated 2016 Feb 29]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278957/
- Tellez-Segura R. (2015). Involvement of Mechanical Stress in Androgenetic Alopecia. International journal of trichology, 7(3), 95–99. doi:10.4103/0974-7753.167468
- Kim-Kaneyama, J. -r. (2005). Uni-axial stretching regulates intracellular localization of Hic-5 expressed in smooth-muscle cells in vivo. Journal of Cell Science, 118(5), 937–949. doi:10.1242/jcs.01683
- Shibanuma, M., Kim-Kaneyama, J. R., Ishino, K., Sakamoto, N., Hishiki, T., Yamaguchi, K., … Nose, K. (2003). Hic-5 communicates between focal adhesions and the nucleus through oxidant-sensitive nuclear export signal. Molecular biology of the cell, 14(3), 1158–1171. doi:10.1091/mbc.02-06-0099
- Yang, L., & Peng, R. (2010). Unveiling Hair Follicle Stem Cells. Stem Cell Reviews and Reports, 6(4), 658–664. doi:10.1007/s12015-010-9172-z
- Kwack, M. H., Sung, Y. K., Chung, E. J., Im, S. U., Ahn, J. S., Kim, M. K., & Kim, J. C. (2008). Dihydrotestosterone-Inducible Dickkopf 1 from Balding Dermal Papilla Cells Causes Apoptosis in Follicular Keratinocytes. Journal of Investigative Dermatology, 128(2), 262–269. doi:10.1038/sj.jid.5700999
- Choi, Y. S., Zhang, Y., Xu, M., Yang, Y., Ito, M., Peng, T., … Millar, S. E. (2013). Distinct functions for Wnt/β-catenin in hair follicle stem cell proliferation and survival and interfollicular epidermal homeostasis. Cell stem cell, 13(6), 720–733. doi:10.1016/j.stem.2013.10.003
-
Kruglikov, I. L. and Scherer, P. E. (2017), Adipocyte‐myofibroblast transition as a possible pathophysiological step in androgenetic alopecia. Exp Dermatol, 26: 522-523. doi:10.1111/exd.13379
- Chéret, J., Bertolini, M., Ponce, L., Lehmann, J., Tsai, T., Alam, M., … Paus, R. (2018). Olfactory receptor OR2AT4 regulates human hair growth. Nature communications, 9(1), 3624. doi:10.1038/s41467-018-05973-0
Can “the pill” cause hair loss in women?
Hormonal birth control is incredibly effective at achieving its intended effect: to prevent pregnancy. However, many online anecdotes suggest that birth control might also harbor unintended consequences: namely, hair loss.
So, do these anecdotes align with reality? Can hormonal contraceptives actually cause hair loss? Are there factors that increase (and decrease) this risk? And if so, what can we do to minimize our likelihood of hair thinning?
This in-depth article uncovers the evidence (and answers).
Key Takeaways
Some (but not all) forms of birth control may contribute to hair loss.
- Some forms of birth control may exacerbate pattern hair loss (androgenic alopecia)
- Certain oral contraceptives may cause temporary hair shedding – similar to what’s observed at the beginning of pregnancy.
- Certain oral contraceptives, when stopped, may lead to temporary hair shedding – similar to “postpartum molting” observed after pregnancy.
These effects are likely due to birth control’s impacts on progesterone, testosterone, and estrogen levels.
Interested in Topical Minoxidil?
High-strength topical minoxidil available, if prescribed*
Take the next step in your hair regrowth journey. Get started today with a provider who can prescribe a topical solution tailored for you.
*Only available in the U.S. Prescriptions not guaranteed. Restrictions apply. Off-label products are not endorsed by the FDA.

Some hormonal birth control is also linked to nutrient depletion and increased inflammatory biomarkers – which may increase the risk of hair loss for certain groups of women. However, research here is still ongoing.
Women with a familial history of female pattern hair loss (androgenic alopecia) should avoid birth control pills with a higher androgen index. Instead, they may want to try options like the NuvaRing®, the Depo-Provera shot, low-androgen implants, or low-androgen combination oral contraceptives (i.e., “the pill”).
Women concerned with all forms of hormonal birth control may want to seek alternative contraceptive options – like condoms or natural family planning (both of which have their own shortcomings, but aren’t connected to hair loss).
The rest of this guide dives deeper into the science behind hormonal birth control, its connection to hair loss, and which options are (and aren’t) as concerning for hair.
Note: we strive to provide content that is error-free and medically accurate. At the same time, it’s unrealistic to get things 100% right, 100% of the time. This is because evidence, opinions, and recommendations are constantly evolving in light of new research. Consider this guide a starting point for your own research, and not medical advice. As always, consult your physician before acting on any information from any resource – including this site.
What is hormonal birth control?
Hormonal birth control is a pharmaceutical intervention designed to prevent pregnancy. It works by suppressing ovulation.
If we were to grossly oversimplify things, female hormonal birth control changes hormone levels to better match what’s observed during pregnancy. This “tricks” the body into thinking it’s already pregnant, so that ovulation stops.
Hair loss & birth control: is there a connection?
Yes and no. The answer varies based on (1) the type of hair loss, and (2) the type of birth control.
For reference, nearly all forms of hormonal birth control use synthetic progesterone and/or estrogens to regulate menstruation and ovulation. Here are some examples:
- Intrauterine device (IUD): A progesterone-only form of hormonal birth control. It is a T-shaped device made of polyethylene that slowly releases progesterone into the uterus to prevent pregnancy.
- Implant: Another progesterone-only form of hormonal birth control placed under the skin of the arm. It is an ethylene device that releases progesterone progressively into the bloodstream directly.
- Depo-Provera Shot: The hormonal birth control shot is another progesterone-only option, administered directly to the bloodstream. It involves quarterly appointments for continued protection.
- Combined oral contraceptive pill (COCs): The combined oral contraceptive pill is a combination of both ethinyl estradiol (estrogen) and various forms of progesterone. Pill administration is every day, with each pill-pack consisting of 28 daily doses. It is administered orally where it is absorbed into the bloodstream via the gut lining.
- Mini-pill: The mini-pill is a progesterone-only hormonal birth control pill. Like COCs, the mini-pill is also absorbed via the digestive system.
- NuvaRing®: A vaginal ring that contains both ethinyl estradiol and progesterone. It is inserted once a month and progressively secretes these hormones to prevent pregnancy.
When it comes to hair loss, newer forms of birth control – i.e., the NuvaRing®, Depo-Provera Shot, and IUD’s – aren’t as well-studied as oral contraceptives. This is because oral contraceptives (i.e., “the pill”) have been around since the 1960’s, whereas newer birth control formulations have really only been on-the-market for the past 10-20 years.
Having said that, nearly all hormonal birth control use progesterone and/or estrogens to block ovulation. Consequently, physicians often apply data on oral contraceptives and hair loss (from the 1970’s) to generalize what we can expect for all hormonal birth control – both new and old.
So, what does the data have to say? The answers might surprise you.
Oral contraceptives
This 1973 literature review catalogued all clinical trials on oral contraceptives and their observed effects of hair health.
Across dozens of studies, the authors found three instances where oral contraceptives can contribute to hair thinning. One instance relates to pattern hair loss; two instances relate to temporary hair shedding.
Pattern hair loss (after starting)
Many oral contraceptives contain synthetic progesterone to help stop ovulation. Interestingly, synthetic progesterone is made from the male hormone testosterone.
Progesterone
Unfortunately, some testosterone-derived synthetic progestins still maintain a certain degree of androgenic (male hormone) activity… which means that in addition to stopping ovulation, they may increase a woman’s testosterone levels.
The male hormone dihydrotestosterone (DHT) is made from testosterone, and it’s believed to be the primary hormone involved in pattern hair loss. So, for women who have pattern hair loss (or a familial history of it), progesterone-containing contraceptives with a “high androgen index” can exacerbate or accelerate this condition.
What can we do about this?
According to that 1973 review, women at-risk of female pattern hair loss should avoid oral contraceptives made from progestins that have a “high androgenic index”. This includes progestins like:
- Levonorgestrel
- Dl-norgestrel
- Norethindrone
- Norgestrel
So, if you’re at-risk of female AGA, you may want to avoid the following hormonal birth control:
- IUD/vaginal rigs: The IUD contains levonorgestrel as its progesterone and may have especially androgenic effects in the absence of estrogen.
- COCs containing the most androgenic progestins.
- The mini-pill: The mini-pill contains norethindrone, an androgenic progestin, as its active ingredient. There are no other variations of the mini-pill.
But even if you’re not at-risk of female pattern hair loss, you might still see fluctuations to you hair health when starting (and stopping) oral contraceptives. Here’s why.
Hair shedding (after starting)
In early pregnancy, fluctuations in progesterone and estrogen levels (alongside increases to stress) can lead to temporary hair shedding. Oral contraceptives help to emulate the hormonal profile of a pregnant woman.
As such, it’s no surprise that one study found that 50% of women using them also experienced temporary hair shedding in the first few months (that usually resolved within six months).
Hair shedding (after quitting)
By mid-pregnancy, many women actually see increased hair density. This is believed to be due to a steady rise in estrogen levels, which may confer protective effects on hair and elongate the growth phase of the hair cycle. Post-pregnancy, estrogen levels drop, these protective effects dissipate, and, consequently, many women experience more hair shedding.
The same is true after quitting birth control: estrogen levels drop, a female experiences oestrogen withdrawal, and Hair typically recovers within 3-6 months.
What can we do about this?
According to that 1973 review, we shouldn’t worry about temporary shedding from “the pill” – because this shedding doesn’t present significantly at the population-level.
“The incidence of diffuse alopecia in women between 1952 and 1971 has remained unchanged although [oral contraceptive] use has increased. This suggests the effect of [oral contraceptives] on alopecia is insignificant.”
In some cases, that review even argues that birth control can improve hair growth… with one study showing that 22% of females on oral contraceptives saw increases to hair density.
Again, this aligns with observations during mid-to-late pregnancy when the protective effects of estrogen kick in, the hair growth cycle elongates, and hair counts increase (temporarily).
As such, the authors concluded that:
“Such findings suggest that when the pill produces any clinically significant effect on hair cycles it is likely to be a favourable one.”
Summary (so far)
According to a widely cited resource on birth control and hair loss (from 1973)…
- Most women should not be concerned about hair loss from oral contraceptives.
- Oral contraceptives with a high androgen index may exacerbate pattern hair loss (androgenic alopecia). For these women, low androgen index birth control is recommended (if any birth control is necessary).
- Upon starting oral contraceptives, 50% of women experience slight increases to hair shedding, which normalizes within six months.
- Upon stopping oral contraceptives, some women experience hair shedding as estrogen levels normalize (similar to postpartum molting). This is temporary.
- In 22% of women, oral contraceptives actually increase hair density.
Have expert opinions evolved since the 1970’s?
To our knowledge, not really.
Nearly forty years after that literature review was published, these conclusions still stand. That means if you visit a doctor with questions about birth control, you’ll likely hear:
- “If you’re at risk of female pattern hair loss, avoid high androgen index contraceptives. Otherwise, don’t worry…” (more on this later)
- “You might shed a little when you start and stop birth control. Otherwise, don’t worry…”
And that’s even despite the explosion of new birth control forms… and even despite the surge in anecdotes of a connection between contraceptive use and hair loss.
So, is it possible that we’re missing something – and these reports online of birth control-related hair loss are more than just anecdotes?
Maybe.
In the last forty years, our understanding of biology has evolved – as has our data on birth control and its myriad effects on the female body.
Not all of its effects are positive.
In fact, a few downstream effects of birth control may contribute to problems indirectly linked to hair loss, namely:
- Inflammation
- Nutrient depletion
…none of which were catalogued in that 1973 review (as we didn’t yet have the data).
Inflammation
When we examine the research on hair loss, there is a clear emerging trend: inflammation, one of the body’s natural immune responses.
The presence of chronic, unresolved inflammation seems to be a significant contributor to almost every form of hair loss, whether that be telogen effluvium (TE), diffuse hair loss, androgenic alopecia (AGA), or even alopecia areata (AA).
In AGA, inflammation seems to lead to hair follicle miniaturization (and thereby hair loss). In AA and TE, inflammatory mediators seem to signal the early transition of the hair follicle into the catagen phase, where hair stops growing. Eventually, these hairs shed.
The bottom-line: if we’re trying to fight hair loss, it may be in our best interest to lower our levels of systemic inflammation – as to not amplify any inflammation already present in the scalp.
So, how does this connect to birth control? Well, it all depends on which hormones are inside your contraceptive: estrogens and/or progestins.
Estrogen-based contraceptives
Preliminary research suggests that estrogen-containing birth controls – like COCs and the NuvaRing® – may have an amplifying effect on inflammation.
In PCOS patients, estrogen-based contraceptives may increase inflammation
For women with polycystic ovarian syndrome (PCOS), birth control – which is usually prescribed as a treatment for PCOS – may ironically exacerbate inflammatory biomarkers that are already elevated in the condition (more on this later).
This has been most notably demonstrated in PCOS patients taking oral contraceptives and subsequently seeing a rise in levels of c-reactive protein (here, here, and here) – one of the foremost biomarkers of inflammation.
It’s unclear what (if any) impact this might have on hair health. Having said that, PCOS is a condition closely tied to (and potentially even causative of) female pattern hair loss.
Knowing this, we probably want to keep any additional inflammation at bay – whether it’s derived from bad food choices or the wrong contraceptive.
Estrogen-based contraceptives may also exacerbate autoimmunity
This literature review found that estrogen-based contraceptive use was associated with an increased risk of various autoimmune conditions, including:
- Multiple sclerosis
- Ulcerative colitis
- Crohn’s disease
- Systemic Lupus Erythematosus
- Interstitial cystitis
Why could this be the case?
Generally, estrogens are proliferative, meaning they stimulate the division of cells. Interestingly, some researchers have hypothesized that the estrogen-autoimmunity connection is due to its potential proliferative effect on immune cells.
The idea: that estrogen may increase immune cell count, causing the immune system to go into overdrive. Estrogen might also promote the survival of these cells, potentially prolonging our immune responses.
On top of this, preliminary in vitro studies suggest that estrogen disrupts the gut lining by inhibiting an important barrier-protective protein, zonulin. This may lead to increased permeability of the intestinal barrier, allowing bacteria, toxins, and inflammatory bacteria membranes into systemic circulation.
As a result, you may experience system-wide inflammation as your body responds to these pathogens that were never supposed to reach our circulation in the first place.
But do these effects actually translate to hair health?
We don’t yet know. But for anyone dealing with hair loss alongside inflammatory-based conditions – like PCOS and/or autoimmunity – you may want to speak with your doctor before jumping on any birth control containing estrogen.
Nutrient depletion
Many drugs reduce our absorption of nutrients. Many drugs also increase our need for nutrients. But birth control pills (specifically, COCs) are one of the worst offenders.
This isn’t just because they’re so widely prescribed, but also because so few women are actually notified of the risks of nutrient repletion while taking them.
Specifically, COCs have been known to deplete the following nutrients:
- Folate. Depletion of folate impairs the cell division and DNA synthesis that promotes hair growth at the most basic level. However, folate is also needed for homocysteine detox and plays a role in metallothionein production, the protein needed for heavy metal detoxification. So, depletion of folate may contribute to the overall free radical load on the body.
- Vitamin B2. Vitamin B2 is needed for adenosine triphosphate (ATP; energy for the body and essential for fueling hair growth) production and is a co-factor in metallothionein synthesis.
- Vitamin B6. Much like B2, B6 is a co-factor in ATP and metallothionein production, along with a plethora of other enzymatic reactions.
- Vitamin B12. B12 is necessary for energy production, metallothionein synthesis, and cell proliferation.
- Vitamin C. Vitamin C is required for the production of collagen, carnitine (an amino acid that promotes metabolic health), wound healing, and reducing the free radical load on the body.
- Vitamin E. Vitamin E is a fat-soluble antioxidant that is especially important for skin and possibly hair health. One small human trial demonstrated that 100mg of vitamin E supplementation for 8 months resulted in an average increase of 98.3 in hair count.
- Selenium. Selenium is a mineral that acts as a co-factor in glutathione activity (that of which seems to be lowered in hair loss patients), supports the thyroid, and prevents oxidative stress.
- Magnesium. Magnesium is involved in so many reactions in the body, it’s hard to pick just a few to list. But, some of the noteworthy effects of magnesium include supporting healthy insulin levels, decreasing inflammation, and promoting skin health.
- Zinc. Zinc is an antioxidant, immune-supportive mineral and deficiency likely contributes to hair loss. Researchers hypothesize that zinc may regulate gene transcription required for hair growth, prevent regression into the catagen phase, and acceleration of hair follicle recovery.
Although it’s unclear just how much of a factor nutrient deficiencies are in hair loss, we know that some specific ones are likely to be an issue, especially in TE.
So, if have taken birth control in the past or are currently taking birth control, it’s important that you be made aware of potential increases in nutrient requirements and potential deficiencies you may encounter.
Birth control for PCOS: will it help my hair loss or make it worse?
Hormonal birth control, especially COCs, is often the first line of treatment for relieving the symptoms of PCOS.
In theory, this makes sense. The estrogen may interfere with androgen activity, ameliorating some of the symptoms associated with excess androgens in PCOS.
However, COCs don’t address the insulin resistance, inflammation, and oxidative stress that are a factor in a lot of the PCOS issues, even for lean patients. In fact, sometimes it may get worse (many women report this).
Considering the depletion of antioxidant nutrients, the potential inflammatory response of the body, the androgenic effect of some synthetic progestins, and the role these may all play in PCOS pathology, the reports of women whose PCOS symptoms get worse on COCs are not unfounded.
The truth is that every women’s experience on birth control will be different. Individual physiology and biochemical milieu determine the response.
So, determining whether COCs will benefit or worsen PCOS symptoms is kind of like Russian roulette. No one can predict how you may react to it. Your best bet is to work with your physician to assess the risks and benefits of utilizing COCs.
So, what are your options?
Navigating pregnancy prevention while avoiding side effects is no easy feat.
Based on the evidence provided, here is what seems to be the safest for preventing contraceptive-associated hair loss:
- NuvaRing®. The NuvaRing® contains a less-androgenic progesterone in combination with estrogen. However, the estrogen content may be problematic, considering some of its effects on the body.
- COCs with less-androgenic progestins. Like the Nuva-Ring, these oral contraceptives with less androgenic progestins avoid possible adverse effects on hair related to male hormones. Though it should be noted that estrogen may not necessarily be favorable for hair growth.
- Depo-Provera shot. This shot is progesterone-only and contains a progesterone with less androgenic activity.
- Implant. The implant is solely formulated with a low androgen activity progesterone.
There are also non-hormonal methods available, like the copper IUD and the natural family planning method (NFP). However, the copper IUD may throw off zinc levels and NFP is time-intensive, requires a lot of mental awareness, and has a failure rate of about 25%.
Deciding which birth control is for you is a really individual choice and should be made based on the time you have and how much concentration you are willing to commit to avoid possible issues with hair loss.
Final thoughts
Based on the evidence currently available to us, hormonal birth control can very well influence hair loss in certain groups of women.
However, there are mixed results. Some women experience hair loss after starting and/or stopping hormonal contraceptives, while others find that “the pill” can improve their hair density or even hair loss from PCOS.
In short, there’s no way to predict what could happen on the individual level. That means you’ll likely need to do some personal experimentation.
Your best bet is to talk over your concerns with your doctor who, with the knowledge of your individual physiology, can help you better understand your unique risk and what contraceptive option might be best for you.
It’s hard to predict who is (and isn’t) susceptible to contraceptive-related hair loss. Sometimes, it requires some personal experimentation. If you have a good doctor, it may help to speak with him or her about your unique risk profile.
IngredientsPharmaceuticalsNatural RemediesCompany ReviewsBy Sarah King, PhDJul 16, 2024GPR44: Can This Gene Predict Hair Regrowth From PGD2 Inhibitors?
Can your genes predict the effectiveness of PGD2 inhibitors for hair loss? The GPR44 gene, encoding the prostaglandin D2 receptor (DP2), is a potential target in hair loss treatment. Elevated levels of prostaglandin D2 (PGD2) have been linked to hair growth inhibition, making GPR44 a key player. How...By Sarah King, PhDJul 16, 2024SULT1A1: Can This Gene Predict Hair Regrowth From Minoxidil? | The Evidence
Can your genes predict minoxidil effectiveness? The SULT1A1 gene, which encodes sulfotransferase, might hold the key, at least according to gene testing companies. SULT1a1 codes for an enzyme that activates minoxidil, a common hair loss treatment. While some studies suggest certain SULT1A1 variants ...By Sarah King, PhDMay 31, 2024Microneedling the Scalp: Does it Cause Scarring?
Can repeated microneedling on the scalp cause scarring? There aren’t yet long-term studies answering this question. On the one hand, microneedling increases neocollagenesis (i.e., the formation of new collagen, or skin tissue). On the other hand, studies show that microneedling-induced collage...By Sarah King, PhDMay 9, 2024Pyrilutamide (KX-826): A Promising Future Treatment For Hair Loss?
Pyrilutamide, also known as KX-826, is an anti-androgen topical currently being tested for the treatment of androgenic alopecia (AGA). Initial studies suggested that pyrilutamide might help reverse hair loss. However, larger-scale clinical studies have found no significant differences in hair regrow...By Sarah King, PhDMay 9, 2024HMI-115: What We Know So Far
HMI-115 lowers prolactin levels and is currently in clinical trials for the treatment of androgenic alopecia (AGA). Internal, non-peer-reviewed research suggests that HMI-115 may promote hair regrowth in monkeys. Anecdotes from its phase I trials in humans imply that HMI-115 may also regrow hair in ...By Sarah King, PhDMay 2, 2024Green Tea: Is It An Effective Hair Loss Treatment?
Green tea extract contains epigallocatechin gallate (EGCG) and many other compounds that allegedly improve hair growth. On the one hand, in vitro studies suggest that EGCG might inhibit hair follicle damage. On the other hand, human studies do not yet exist showing that green tea – as a supplement o...By Sarah King, PhDApr 25, 2024Inositol: A Sugar That Supports Hair Growth? | Clinical Study Analysis
Inositol (in the form of myo-inositol or D-chiro-inositol) is found in many hair growth supplements. Clinical studies suggest inositol might normalize androgen levels in women with polycystic ovarian syndrome (PCOS). For these reasons, marketers often claim inositol can help regrow hair for those wi...By Sarah King, PhDApr 25, 2024Pea Sprout Extract: A Hair Growth Miracle? Little Evidence, Lots Of Hype
What does the science say about pea sprout extract and its ability to combat hair loss? On the on hand, pea sprouts might improve hair growth by reducing non-growing hairs and increasing hair density. On the other hand, the studies supporting pea sprout extract face methodological concerns, such as ...By Sarah King, PhDApr 25, 2024Zinc Supplements For Hair Loss: A Hard Look Into The Science
Zinc is a popular trace element found in hair growth supplements. Animal studies suggest that zinc is required for healthy hair cycling. Human studies suggest that zinc deficiencies can cause hair loss from telogen effluvium. One study found that zinc sulfate might help with non-descript hair loss i...By Sarah King, PhDApr 25, 2024Japanese Knotweed For Hair Loss: A Scientific Analysis
Japanese knotweed contains resveratrol and apigenin. In vitro studies suggest these compounds have antioxidant, anti-inflammatory, and anti-aging properties. Marketers claim these compounds support hair regrowth. So can Japanese knotweed regrow hair? In this article, we review the scientific literat... - Mission Statement
 Scroll Down
Scroll Down