- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
Scroll Down
Popular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Free CalculatorTopical Finasteride Calculator
- Free Interactive GuideInteractive Guide: What Causes Hair Loss?
- Free ResourceFree Guide: Standardized Scalp Massages
- Free Course7-Day Hair Loss Email Course
- Free DatabaseIngredients Database
- Free Interactive GuideInteractive Guide: Hair Loss Disorders
- Free DatabaseTreatment Guides
- Free Lab TestsProduct Lab Tests: Purity & Potency
- Free Video & Write-upEvidence Quality Masterclass
- Free Interactive GuideDermatology Appointment Guide
More
Articles100+ free articles.
-
Hims Hair Growth Reviews: The Pros, Cons, and Real Results
-
Topical Finasteride Before and After: Real Case Studies
-
How to Reduce the Risk of Finasteride Side Effects
-
10 Best DHT-Blocking Shampoos
-
Best Minoxidil for Men: Top Picks for 2026
-
7 Best Oils for Hair Growth
-
Switching From Finasteride to Dutasteride
-
Best Minoxidil for Women: Top 6 Brands of 2026
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
Before-Afters- Transformation Photos
Our library of before-after photos.
- Client Testimonials
Read the experiences of members
Before-Afters/ Client Testimonials- Popular Treatments
-
ArticlesScalp Psoriasis: Symptoms, Causes, and Effects on Hair Loss
First Published Mar 25 2025Last Updated Jun 14 2025Natural RemediesPharmaceutical Researched & Written By:Sarah King, PhD
Researched & Written By:Sarah King, PhD Reviewed By:Rob English, Medical Editor
Reviewed By:Rob English, Medical Editor
Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn MoreArticle Summary
Scalp psoriasis goes beyond surface-level flaking; it’s a chronic autoimmune condition driven by genetic and immune system factors. From thick plaques and itching to potential hair loss, it can seriously impact daily life. Curious about what causes it, how to tell it apart from similar conditions, and the best ways to treat it? Dive into our comprehensive guide to scalp psoriasis and discover how to manage symptoms and protect your scalp health
Full Article
From thick, scaly patches to itching and irritation, scalp psoriasis is an autoimmune condition that can be both uncomfortable and persistent. But what triggers it, and how can you manage flare-ups effectively? In this article, we’ll explore what scalp psoriasis is, its symptoms and causes, treatment options, how it affects hair health, and simple ways to support your scalp long-term.
Key Takeaways
- What is it? Scalp psoriasis is a chronic autoimmune skin condition that causes the skin on the scalp to produce cells too quickly, resulting in thick, scaly patches. These plaques can be itchy and painful and extend beyond the scalp to the forehead, neck, and ears. It’s a form of plaque psoriasis and is driven by an overactive immune response influenced by genetic and environmental factors.
- What are the symptoms? Common symptoms include raised red, salmon-colored, or purple patches, depending on skin tone, covered with silvery or gray scales. Other signs are flaking (often mistaken for dandruff), intense itching, soreness, burning, and sometimes temporary hair loss due to inflammation or scratching. In more severe cases, plaques can cover the entire scalp and cause sleep disturbances or discomfort.
- What is the prevalence? Scalp psoriasis affects an estimated 50–80% of people with psoriasis. While one study reported a 7.6% prevalence among psoriasis patients in Malaysia, this likely underrepresents the global burden. It can develop at any age, though most cases are diagnosed in adulthood, with women being slightly more affected than men.
- What are the most common treatments? Treatment often starts with topical corticosteroids and vitamin D analogs to reduce inflammation and slow cell turnover. Medicated shampoos with salicylic acid, coal tar, or ketoconazole are widely used. In more persistent or severe cases, systemic medications like methotrexate or biologics may be prescribed. Combination therapies such as Enstilar foam are also effective.
- How else can I improve it? Using gentle hair care products, avoiding scratching or picking, and alternating medication with moisturizing shampoos can help. Natural remedies like aloe vera or apple cider vinegar may provide soothing relief. Managing stress, avoiding known triggers (like smoking, certain medications, or cold weather), and making dietary adjustments may also reduce flare-ups.
- Final thoughts. Scalp psoriasis is a complex and often frustrating condition, but with the right treatment plan and supportive care, it can be effectively managed. Taking a proactive approach by addressing both medical treatment and lifestyle adjustments can significantly reduce symptoms and improve overall scalp health and quality of life.
What is Scalp Psoriasis?
Scalp psoriasis is a chronic autoimmune skin condition affecting the scalp but often spreading below the hairline to the forehead, ears, and neck.[1]Leong, W.C., Tang, J.J. (2022). Scalp psoriasis and Dermatology Life Quality Index: A retrospective study based on 12-year data from the Malaysian Psoriasis Registry. Malaysian Family Physician. … Continue reading It causes an overproduction of skin cells, leading to the formation of thick, scaly patches on the skin.
Scalp psoriasis is a form of plaque psoriasis that specifically targets the scalp region. It results from an overactive immune system, genetics, and environmental factors (which we will cover below). The condition causes skin cells to reproduce too quickly, creating raised, discolored plaques that can be dry, itchy, and irritating.[2]National Institute of Arthritis and Musculoskeletal and Skin Diseases. (no date). Psoriasis. NIH. Available at: https://www.niams.nih.gov/health-topics/psoriasis (Accessed: March 2025)
How Does Scalp Psoriasis Present?
Macroscopic Presentation
Scalp psoriasis typically presents as raised reddish or salmon-colored patches with white scales on light to medium skin tones.[3]NHS. (no date). Psoriasis). National Health Service. Available at: https://www.nhs.uk/conditions/psoriasis/ (Accessed: March) On darker skin, the patches may appear purple with gray scales. These lesions can be a single patch or multiple patches, or they may affect the entire scalp and extend to the forehead, back of the neck, and behind and inside the ears.[4]Blakely, K., Gooderham, M. (2016). Management of scalp psoriasis: current perspectives. Psoriasis. 29(6). 33-40. Available at: https://doi.org/10.2147/PTT.S85330
This condition can range from mild and almost unnoticeable to severe, with thick, crusted sores. Intense itching is common and can significantly impact sleep and daily life.[5]AAD. (no date). Scalp Psoriasis: Symptoms. American Academy of Dermatology Association. Available at: https://www.aad.org/public/diseases/psoriasis/treatment/genitals/scalp-symptoms (Accessed: March) Scalp psoriasis often results in skin flaking, which may be mistaken for dandruff, but it also includes additional symptoms such as red or purple bumpy patches, soreness, and burning.
Scalp psoriasis is typically diagnosed clinically by a dermatologist through a physical examination of the skin, scalp, and nails.[6]National Psoriasis Foundation. (2025). Scalp Psoriasis. National Psoriasis Foundation. Available at: https://www.psoriasis.org/scalp (Accessed: March 2025) Your healthcare provider may also refer you for a biopsy to confirm the diagnosis and rule out other conditions.
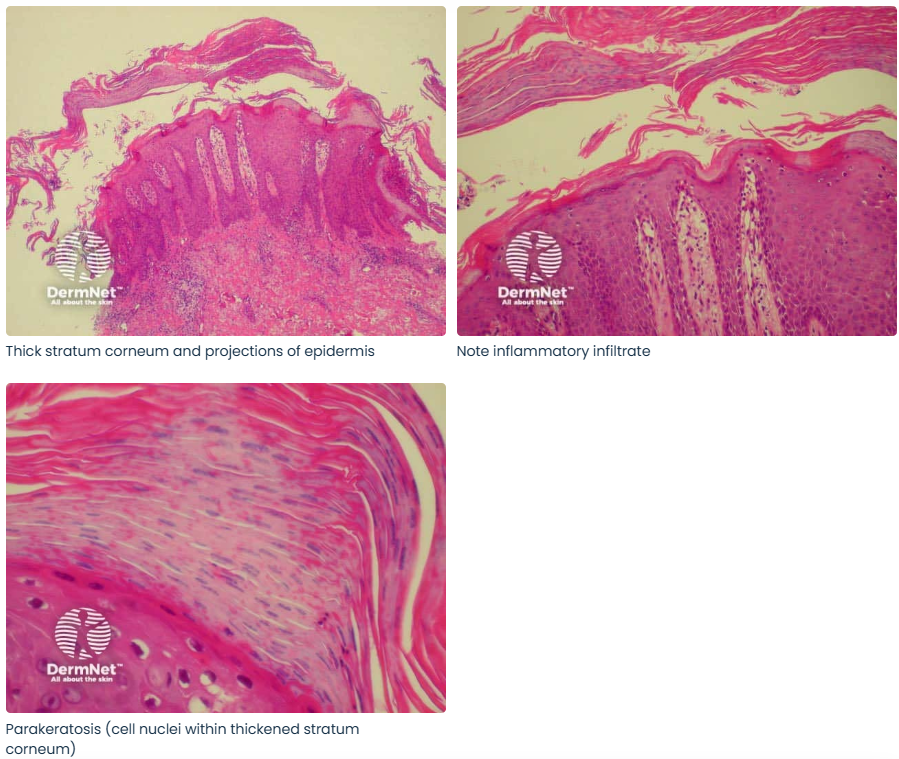
Figure 1: Scalp psoriasis in the scalp showing a silvery plaque extending outwards from the hairline.[7]Elghblawi, E., Stanway, A., Coulson, I. (2022). Scalp Psoriasis. DermNet. Available at: https://dermnetnz.org/topics/scalp-psoriasis (Accessed: March 2025)
Microscopic Presentation
Scalp psoriasis shows distinct microscopic features that reveal its underlying inflammatory nature and accelerated skin turnover.
The epidermal changes are most noticeable with a thickened skin layer, known as regular acanthosis, with elongated “finer-like” extensions into the deeper tissue, referred to as rete ridges.[8]Raychaudri, S.K., Maverakis, E., Raychaudhri, S.P. (2014). Diagnosis and classification of psoriasis. Autoimmune Review. 13(4-5). 490-495. Available at: https://doi.org/10.101016/j.autrev.2014.01.008
Other common features are patchy areas with reduced or excess skin cell maturation (hypo- or hypergranulosis) and thinning of the upper skin layers, or supra papillary plates, making blood vessels more visible.[9]Basir, H.R.G., Alirezaei, P., Hamian, Z., Khanlarzadeh, E. (2018). Are quantitative histopathologic criteria capable of differentiating psoriasis from chronic dermatitis? Clinical, Cosmetic, and … Continue reading
Figure 2: Epidermal features of psoriasis.[10]DermNet. (2009). Psoriasis Overview. Available at: https://dermnetnz.org/cme/scaly-rashes/psoriasis-overview (Accessed: March 2025)
Furthermore, people with scalp psoriasis typically experience abnormal skin shedding with an accumulation of immature skin cells (parakeratosis) mixed with neutrophil immune cells, forming tiny abscesses called Munro microabscesses.[11]Butacu, A.I., Toma, C., Negulet, I-E., Manole, I., Banica, A.N., Plesea, A., Badircea, I.A., Iancu, I., Tiplica, G-S. (2024). Updates on Psoriasis in Special Areas. Journal of Clinical Medicine. … Continue reading
In the dermal layer, there are also significant changes. Immune cells accumulate around blood vessels in the middle skin layers, forming a perivascular lymphocytic infiltrate. The blood vessels themselves are dilated and twisted, contributing to the typical redness seen in psoriasis.
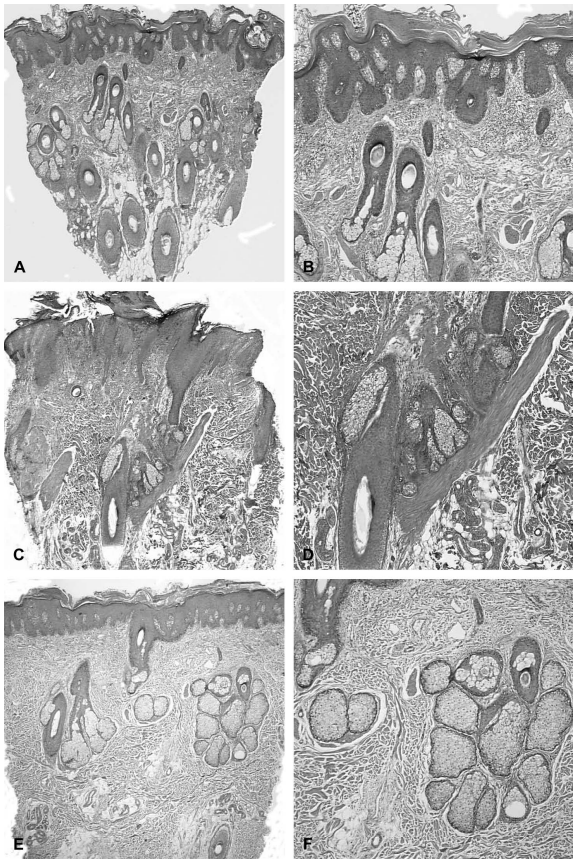
Other unique diagnostic clues help differentiate scalp psoriasis from other conditions. For instance, there are “spongy” pustules in the spinous later, known as Kogoj pustules, which are collections of neutrophils.[12]Mirza, H.A., Badri, T., Kwan, E. (2025). Generalized Pustular Psoriasis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: … Continue reading Another unique feature is the atrophy (shrinking) of sebaceous glands, which contrasts with the normal scalp, where these glands are active.[13]Werner, B., Brenner, F.M., Boer, A. (2008). Histopathologic Study of Scalp Psoriasis: Peculiar Features Including Sebaceous Gland Atrophy. The American Journal of Dermatopathology. 30(2). 93-100. … Continue reading
Figure 3: A-D: Atrophic sebaceous glands in scalp psoriasis. E-F: More “normal” looking sebaceous glands with larger lobules.[14]Werner, B., Brenner, F.M., Boer, A. (2008). Histopathologic Study of Scalp Psoriasis: Peculiar Features Including Sebaceous Gland Atrophy. The American Journal of Dermatopathology. 30(2). 93-100. … Continue reading
The epidermal surface also becomes irregular with scalp psoriasis, leading to wart-like bumps (papillomatosis) scaling around hair follicles and pinpoint bleeding (Auspitz’s sign).[15]Dias, M.F.R.G., Loures, A., El Kadi, N., Aranha, N.S., Machado, A., Fontinha, P.R.B., Dutra, H., Trueb, R.M. (2024). Trichoscopic pearl: dynamic trichoscopy sequence of scalp psoriasis before and … Continue reading
Figure 4: Left side: patients with scalp psoriasis showing thick scaling. Right side: Manifestation of Auspitz’s sign, showing as twisted capillary loops, comma vessels, and red dots.[16]Dias, M.F.R.G., Loures, A., El Kadi, N., Aranha, N.S., Machado, A., Fontinha, P.R.B., Dutra, H., Trueb, R.M. (2024). Trichoscopic pearl: dynamic trichoscopy sequence of scalp psoriasis before and … Continue reading
Affected areas of the scalp may also show reduced hair density, and the hair strand itself may have a fragile, damaged cuticle. Moreover, biofilms form on the scalp surface, consisting of clusters of bacteria and yeast linked by sticky strands.[17]Stepanova, A.A., Kornisheva, V.G., Raznatovskiy, K.I., Semolina, O.A. (2020). Scalp Psoriasis and Biofilms: Electron Microscopy. Journal of Microbiology & Experimentation. 8(5). 179-182. … Continue reading These biofilms can contribute to the disease’s persistence and severity.
What is the Difference Between Scalp Eczema and Scalp Psoriasis?
We cover some distinctions between scalp eczema and scalp psoriasis in our Scalp Eczema Ultimate Guide – here’s a summary:
Visual Distinctions
Scalp eczema and psoriasis have subtle visual differences.
Scalp eczema causes patches of dry skin that may be itchy and inflamed. The size and shape of these patches can change over time. The rash tends to blend into the surrounding skin and may be less well-defined.
Scalp psoriasis typically presents as thicker white scales with more well-defined areas of involvement. It often causes red patches with silvery scales that appear thick and raised. Psoriasis plaques usually extend beyond the hairline.
Differences in Causes and Triggers
The underlying causes and triggers for both conditions differ significantly.
Scalp eczema conditions can be caused by a combination of genetic and environmental factors, triggered by skin irritants like soaps, detergents, and disinfectants, exacerbated by allergens like dust, pollen, and certain foods, and heat exposure and increased sweating can lead to flare-ups.
Scalp psoriasis, however, results from an overactive immune system and is classified as an autoimmune disease.[18]Medical News Today (2025). How to tell the difference between scalp eczema and psoriasis. Available at: https://www.medicalnewstoday.com/articles/scalp-eczema-vs-psoriasis (Accessed: March 2025) It can be triggered by factors like stress, infections, skin injuries, and certain medications.
Treatment Approaches
Common treatments used to treat both scalp eczema and scalp psoriasis include:
- Topical corticosteroids to reduce inflammation and itching.
- Medicated shampoos.
- Moisturizers.
- Light therapy (phototherapy).
- Lifestyle changes to avoid triggers and reduce stress.
Several treatments for the two conditions differ, however.
Treatments typically used to treat scalp eczema include:
- Antihistamines to relieve itching.
- Topical calcineurin inhibitors (e.g., tacrolimus, pimecrolimus) for non-steroidal treatment.
- Wet wrap therapy for severe cases.
- Prescription anti-inflammatory creams.
Treatments typically used to treat scalp psoriasis include:[19]American Academy of Dermatology Association. (no date). Scalp Psoriasis: Shampoos, Scale Softeners, and Other Treatments. AAD. Available at: … Continue reading
- Salicylic acid-based products to help remove scales.
- Vitamin D analogs (e.g., calcipotriene) to slow skin cell growth.
- Tazarotene (a topical retinoid) slows cell growth and reduces inflammation.
- Systemic medications for severe cases, including methotrexate, cyclosporine, and biologics (e.g., adalimumab, etanercept, and ustekinumab).
- Excimer laser treatment for targeted therapy of psoriasis plaques.
What Are the Causes of Scalp Psoriasis?
Scalp psoriasis is a complex condition influenced by multiple factors.
Genetic predisposition plays a significant role, as the condition tends to run in families. Over two dozen genes have been identified that may contribute to psoriasis development, with the HLA-C*6:02 gene being the strongest genetic risk factor.[20]Patel, H.A., Revankar, R.R., Pedroza, S.T., Graham, S., Feldman, S.R. (2023). The Genetic Susceptibility to Psoriasis and the Relationship of Linked Genes to Our Treatment Options. International … Continue reading Other genetic variants, such as those in interleukins 17A, 12B, and 10 genes, are also associated with an increased risk of developing psoriasis.
Scalp psoriasis is mainly caused by a dysfunction in the immune system. In this condition, the immune system mistakenly attacks healthy skin cells, resulting in rapid cell turnover. T-cells, which are normally responsible for fighting infections, begin to target healthy skin cells instead.[21]Schadler, E.D., Ortel, B., Mehlis, S.L. (2019). Biologics for the primary care physician: Review and treatment of psoriasis. Disease-a-month:DM. 65(3). 51-90. Available at: … Continue reading This immune dysfunction leads to the overproduction of skin cells, which causes the characteristic plaques and scaling associated with psoriasis.
Several environmental triggers can also initiate or exacerbate scalp psoriasis. These include infections, particularly strep throat and skin infections, as well as skin trauma like cuts, scrapes, bug bits, or severe sunburns.[22]Zhou, S., Yao, Z. (2022). Roles of Infection in Psoriasis. International Journal of Molecular Sciences. 23(13). 6955. Available at: https://doi.org/10.3390/ijms23136955 Stress is another significant trigger, as it can initiate or worsen psoriasis symptoms.[23]Yang, H., Zheng, J. (2020). Influence of stress on the development of psoriasis. Clinical and Experimental Dermatology. 45(3). 284-288. Available at: https://doi.org/10.1111/ced.14105
Additionally, cold, dry weather conditions, smoking, exposure to secondhand smoke, and heavy alcohol consumption can also contribute to flare-ups.[24]Zheng, X., Wang, Q., Luo, Y., Lu, W., Jin, L., Chen, M., Zhu, W., Kuang, Y. (2021). Seasonal Variation of Psoriasis and Its Impact in the Therapeutic Management: A Retrospective Study on Chinese … Continue reading,[25]Miao, M., Yan, J., Sun, Y., Liu, J., Guo, S. (2025). Psoriasis: Unraveling Disease Mechanisms and Advancing Pharmacological and Nontechnological Treatments. Journal of Inflammation Research. 10(18). … Continue reading
In some cases, medications can trigger or worsen scalp psoriasis:
- Lithium.[26]Mayo Clinic. (no date). Psoriasis. Available at: https://www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840 (Accessed: March 2025)
- High blood pressure medications like ACE inhibitors.
- Antimalarials.
- Rapid withdrawal of oral or injected corticosteroids.
- Some anti-inflammatory medicines, including ibuprofen.[27]NHS. (2022). Psoriasis. Available at: https://www.nhs.uk/conditions/psoriasis/causes/ (Accessed: March 2025)
It should be noted that while these factors may contribute to the pathogenesis of scalp psoriasis, the condition usually results from a combination of multiple factors. Not everyone with genetic risk factors will develop scalp psoriasis, and the severity and frequency of flare-ups can vary widely among individuals.
What is the Prevalence of Scalp Psoriasis?
According to a study in Malaysia, scalp psoriasis is estimated to affect about 7.6% of patients with psoriasis in places other than the scalp.[28]Leong, W.C., Tang, J.J. (2022). Scalp psoriasis and Dermatology Life Quality Index: A retrospective study based on 12-year data from the Malaysian Psoriasis Registry. Malaysian Family Physician. … Continue reading However, this figure may be underestimated, as other sources suggest that scalp involvement occurs in 50-80% of psoriasis patients.[29]Blakely, K., Gooderham, M. (2016). Management of scalp psoriasis: current perspectives. Psoriasis. 29(6). 33-40. Available at: https://doi.org/10.2147/PTT.S85330
Scalp psoriasis can occur at any age, but it typically follows patterns similar to general psoriasis:
- The mean age of onset is ~29 years of age for women and ~36 years for men.
- More common in adults, but about one-third of cases are diagnosed before age 20.
- Slightly more prevalent in women, with a male-to-female ratio of 1:1.56.
What is the Impact of Scalp Psoriasis on Hair Loss?
While scalp psoriasis doesn’t directly cause permanent hair loss, there is a relationship between the condition and increased hair shedding.
Correlation with Hair Loss Conditions
Scalp psoriasis is associated with increased hair shedding and decreased hair density, particularly in areas affected by psoriatic plaques. These lesions can lead to diffuse hair loss, which may be exacerbated by inflammation and itching.[30]Almeida, M.C., Romiti, R., Doche, I., Valente, N.Y.S., Donati, A. (2013). Psoriatic scarring alopecia. Anais Brasileiros de Dermatologia. 88(6 Suppl 1). 29-31. Available at: … Continue reading It can also result in localized alopecia where the psoriatic plaques are located and generalized telogen effluvium.[31]Song, B., Liu, X., Jin, H. (2024). Ixekizumab Improved Refractory Erythrodermic Psoriasis with Comorbid Diffuse Alopecia: A Case Report with 52-Week Follow-Up. Clinical, Cosmetic and Investigational … Continue reading
The mechanism of hair loss in scalp psoriasis includes inflammatory destruction of the hair follicle, as seen in scarring alopecias. Histological studies have shown inflammatory destruction of the infundibular (upper) region of the hair follicle, leading to the loss of the hair follicle (follicular drop-out) and fibrosis.[32]Wright, A.L., Messenger, A.G. (1990). Scarring alopecia in psoriasis. Acta Dermato-Venereologica. 70(2). 156-159. Available at: PMID:1969203
Factors That May Worsen Hair Loss
- Scratching: Persistent itching and scratching damage hair shafts and follicles, potentially leading to scarring or infections that worsen hair loss.
- Harsh Treatments: Overuse of strong medicated shampoos or aggressive removal of scales can weaken hair and increase shedding.
- Plaque Build-Up: Thick plaques block follicles, preventing new hair growth and increasing breakage.
Preventive Measures
To minimize hair loss:
- Use gentle medicated shampoos and topical treatments.
- Avoid scratching or picking at plaques, and keep nails trimmed and smooth.
- Alternate between medicated and non-medicated shampoos to prevent dryness
- Avoid aggressive hair regrowth treatments that might increase local inflammation, like microneedling, topicals containing retinoic acid, scalp massages, PRP, and mesotherapy.
How Can I Treat Scalp Psoriasis?
Medical Treatments
There are a diverse array of medical treatments for scalp psoriasis. Topical corticosteroids and vitamin D analogs are commonly prescribed.[33]Kim, G.K. (2010). The Rationale Behind Topical Vitamin D Analogs in the Treatment of Psoriasis. Journal of Clinical and Aesthetic Dermatology. 3(8). 46-53. Available at: PMID: 2087752 Corticosteroids help reduce inflammation, while vitamin D analogs like calcipotriene (Dovonex) can be applied at night to promote healthy skin cell growth. Combination products such as Talconex Scalp or Enstilar Foam, which contain both a vitamin D analog and a strong steroid, are also effective.
Medicated shampoos play an important role in managing scalp psoriasis. Shampoos containing salicylic acid help soften and remove scales, while coal tar shampoos can reduce itching and inflammation.[34]National Psoriasis Foundation. (no date). Best Psoriasis Shampoos Your Scalp Will Love. Available at: https://www.psoriasis.org/advance/best-psoriasis-shampoos (Accessed: March 2025) Ketoconazole shampoos may be recommended for their anti-inflammatory properties.
For moderate to severe cases, systemic medications like biologics or small molecules may be prescribed. These include methotrexate, ciclosporin, and oral retinoids, which are used by about 10-20% of people with moderate or severe psoriasis.[35]Sbidian, E., Chaimani, A., Garcia-Doval, I., Doney, L., Dressler, C., Hua, C., Hughes, C., Naldi, L., Afach, S., Le Cleach, L. (2021). Systemic pharmacological treatments for chronic plaque … Continue reading
Natural and Home Remedies
Natural remedies can complement medical treatments by providing relief and soothing the scalp. Aloe vera gel and apple cider vinegar can help to relieve some of the irritation and assist in maintaining moisture levels.[36]Medical News Today. (2019). Can aloe vera treat psoriasis? Available at: https://www.medicalnewstoday.com/articles/320081 (Accessed: March 2025)
Stress management techniques like meditation or yoga may help prevent flare-ups. Some people report symptom improvement after removing dairy or gluten from the diet, although this varies from person to person.[37]National Psoriasis Foundation. (no date). Dietary Modifications. Available at: https://www.psoriasis.org/dietary-modifications (Accessed: March 2025)
Final Thoughts
Scalp psoriasis is a chronic, immune-mediated condition that can significantly impact the quality of life due to the inflammation and discomfort it causes. Rooted in genetic susceptibility and driven by immune dysfunction, scalp psoriasis is often worsened by environmental and lifestyle triggers. While it doesn’t directly cause permanent hair loss, inflammation, itching, and harsh treatments can lead to increased hair thinning. Managing scalp psoriasis effectively often requires a combination of medical therapies and supportive care, including gentle scalp practices and trigger avoidance.
References[+]
References ↑1, ↑28 Leong, W.C., Tang, J.J. (2022). Scalp psoriasis and Dermatology Life Quality Index: A retrospective study based on 12-year data from the Malaysian Psoriasis Registry. Malaysian Family Physician. 17(3). 84-88. Available at: https://doi.org/10.51866/oa.146 ↑2 National Institute of Arthritis and Musculoskeletal and Skin Diseases. (no date). Psoriasis. NIH. Available at: https://www.niams.nih.gov/health-topics/psoriasis (Accessed: March 2025) ↑3 NHS. (no date). Psoriasis). National Health Service. Available at: https://www.nhs.uk/conditions/psoriasis/ (Accessed: March) ↑4, ↑29 Blakely, K., Gooderham, M. (2016). Management of scalp psoriasis: current perspectives. Psoriasis. 29(6). 33-40. Available at: https://doi.org/10.2147/PTT.S85330 ↑5 AAD. (no date). Scalp Psoriasis: Symptoms. American Academy of Dermatology Association. Available at: https://www.aad.org/public/diseases/psoriasis/treatment/genitals/scalp-symptoms (Accessed: March) ↑6 National Psoriasis Foundation. (2025). Scalp Psoriasis. National Psoriasis Foundation. Available at: https://www.psoriasis.org/scalp (Accessed: March 2025) ↑7 Elghblawi, E., Stanway, A., Coulson, I. (2022). Scalp Psoriasis. DermNet. Available at: https://dermnetnz.org/topics/scalp-psoriasis (Accessed: March 2025) ↑8 Raychaudri, S.K., Maverakis, E., Raychaudhri, S.P. (2014). Diagnosis and classification of psoriasis. Autoimmune Review. 13(4-5). 490-495. Available at: https://doi.org/10.101016/j.autrev.2014.01.008 ↑9 Basir, H.R.G., Alirezaei, P., Hamian, Z., Khanlarzadeh, E. (2018). Are quantitative histopathologic criteria capable of differentiating psoriasis from chronic dermatitis? Clinical, Cosmetic, and Investigational Dermatology. 11. 239-244. Available at: https://doi.org/10.2147/CCID.S160697 ↑10 DermNet. (2009). Psoriasis Overview. Available at: https://dermnetnz.org/cme/scaly-rashes/psoriasis-overview (Accessed: March 2025) ↑11 Butacu, A.I., Toma, C., Negulet, I-E., Manole, I., Banica, A.N., Plesea, A., Badircea, I.A., Iancu, I., Tiplica, G-S. (2024). Updates on Psoriasis in Special Areas. Journal of Clinical Medicine. 13(24). 7549. Available at: https://doi.org/10.3390/jcm13247549 ↑12 Mirza, H.A., Badri, T., Kwan, E. (2025). Generalized Pustular Psoriasis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK493189/ (Accessed: March 2025) ↑13, ↑14 Werner, B., Brenner, F.M., Boer, A. (2008). Histopathologic Study of Scalp Psoriasis: Peculiar Features Including Sebaceous Gland Atrophy. The American Journal of Dermatopathology. 30(2). 93-100. Available at: https://doi.org/10.1097/dad.0b013e31816421fd ↑15, ↑16 Dias, M.F.R.G., Loures, A., El Kadi, N., Aranha, N.S., Machado, A., Fontinha, P.R.B., Dutra, H., Trueb, R.M. (2024). Trichoscopic pearl: dynamic trichoscopy sequence of scalp psoriasis before and after the development of Auspitz’s sign. Archives of Dermatological Research. 316(39). 1-3. Available at: https://doi.org/10.1007/s00403-023-02788-y ↑17 Stepanova, A.A., Kornisheva, V.G., Raznatovskiy, K.I., Semolina, O.A. (2020). Scalp Psoriasis and Biofilms: Electron Microscopy. Journal of Microbiology & Experimentation. 8(5). 179-182. Available at: https://doi.org/10.15406/jmen.2020.08.00306 ↑18 Medical News Today (2025). How to tell the difference between scalp eczema and psoriasis. Available at: https://www.medicalnewstoday.com/articles/scalp-eczema-vs-psoriasis (Accessed: March 2025) ↑19 American Academy of Dermatology Association. (no date). Scalp Psoriasis: Shampoos, Scale Softeners, and Other Treatments. AAD. Available at: https://www.aad.org/public/diseases/psoriasis/treatment/genitals/scalp-shampoo (Accessed: March 2025) ↑20 Patel, H.A., Revankar, R.R., Pedroza, S.T., Graham, S., Feldman, S.R. (2023). The Genetic Susceptibility to Psoriasis and the Relationship of Linked Genes to Our Treatment Options. International Journal of Molecular Sciences. 24(15). 12310. Available at: https://doi.org/10.3390/ijms241512310 ↑21 Schadler, E.D., Ortel, B., Mehlis, S.L. (2019). Biologics for the primary care physician: Review and treatment of psoriasis. Disease-a-month:DM. 65(3). 51-90. Available at: https://doi.org/10.1016/j.disamonth.2018.06.001 ↑22 Zhou, S., Yao, Z. (2022). Roles of Infection in Psoriasis. International Journal of Molecular Sciences. 23(13). 6955. Available at: https://doi.org/10.3390/ijms23136955 ↑23 Yang, H., Zheng, J. (2020). Influence of stress on the development of psoriasis. Clinical and Experimental Dermatology. 45(3). 284-288. Available at: https://doi.org/10.1111/ced.14105 ↑24 Zheng, X., Wang, Q., Luo, Y., Lu, W., Jin, L., Chen, M., Zhu, W., Kuang, Y. (2021). Seasonal Variation of Psoriasis and Its Impact in the Therapeutic Management: A Retrospective Study on Chinese Patients. Clinical Cosmetic and Investigational Dermatology. 10(14). 459-465. Available at: https://doi.org/10.2147/CCID.S312556 ↑25 Miao, M., Yan, J., Sun, Y., Liu, J., Guo, S. (2025). Psoriasis: Unraveling Disease Mechanisms and Advancing Pharmacological and Nontechnological Treatments. Journal of Inflammation Research. 10(18). 2045-2072. Available at: https://doi.org/10.2147/JIR.S506103 ↑26 Mayo Clinic. (no date). Psoriasis. Available at: https://www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840 (Accessed: March 2025) ↑27 NHS. (2022). Psoriasis. Available at: https://www.nhs.uk/conditions/psoriasis/causes/ (Accessed: March 2025) ↑30 Almeida, M.C., Romiti, R., Doche, I., Valente, N.Y.S., Donati, A. (2013). Psoriatic scarring alopecia. Anais Brasileiros de Dermatologia. 88(6 Suppl 1). 29-31. Available at: https://doi.org/10.1590/abd1806-4841.20132241 ↑31 Song, B., Liu, X., Jin, H. (2024). Ixekizumab Improved Refractory Erythrodermic Psoriasis with Comorbid Diffuse Alopecia: A Case Report with 52-Week Follow-Up. Clinical, Cosmetic and Investigational Dermatology. 8(17). 1811-1814. Available at: https://doi.org/10.2147/CCID.S471582 ↑32 Wright, A.L., Messenger, A.G. (1990). Scarring alopecia in psoriasis. Acta Dermato-Venereologica. 70(2). 156-159. Available at: PMID:1969203 ↑33 Kim, G.K. (2010). The Rationale Behind Topical Vitamin D Analogs in the Treatment of Psoriasis. Journal of Clinical and Aesthetic Dermatology. 3(8). 46-53. Available at: PMID: 2087752 ↑34 National Psoriasis Foundation. (no date). Best Psoriasis Shampoos Your Scalp Will Love. Available at: https://www.psoriasis.org/advance/best-psoriasis-shampoos (Accessed: March 2025) ↑35 Sbidian, E., Chaimani, A., Garcia-Doval, I., Doney, L., Dressler, C., Hua, C., Hughes, C., Naldi, L., Afach, S., Le Cleach, L. (2021). Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database of Systematic Reviews. 2021(4): CD011535. Available at: https://doi.org/10.1002/14651858.CD011535.pub4 ↑36 Medical News Today. (2019). Can aloe vera treat psoriasis? Available at: https://www.medicalnewstoday.com/articles/320081 (Accessed: March 2025) ↑37 National Psoriasis Foundation. (no date). Dietary Modifications. Available at: https://www.psoriasis.org/dietary-modifications (Accessed: March 2025) Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn More
Sarah King, PhD
Dr. Sarah King is a researcher & writer who holds a BSc in Medical Biology, an MSc in Forensic Biology, and a Ph.D. in Molecular and Cellular Biology. While at university, Dr. King’s research focused on cellular aging and senescence through NAD-dependent signaling – along with research into prostaglandins and their role in hair loss. She is a co-author on several upcoming manuscripts with the Perfect Hair Health team.
"... Can’t thank @Rob (PHH) and @sanderson17 enough for allowing me to understand a bit what was going on with me and why all these [things were] happening ... "
— RDB, 35, New York, U.S.A."... There is a lot improvement that I am seeing and my scalp feel alive nowadays... Thanks everyone. "
— Aayush, 20’s, Boston, MA"... I can say that my hair volume/thickness is about 30% more than it was when I first started."
— Douglas, 50’s, Montréal, CanadaWant help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Join Now - Mission Statement
 Scroll Down
Scroll Down